-
Avastin IV (Genentech)
WARNINGS
Gastrointestinal Perforations/Wound Healing Complications
AVASTIN administration can result in the development of gastrointestinal perforation and wound dehiscence, in some instances resulting in fatality. Gastrointestinal perforation, sometimes associated with intra-abdominal abscess, occurred throughout treatment with AVASTIN (i.e., was not correlated to duration of exposure). The incidence of gastrointestinal perforation in patients receiving bolus-IFL with AVASTIN was 2%. The typical presentation was reported as abdominal pain associated with symptoms such as constipation and vomiting. Gastrointestinal perforation should be included in the differential diagnosis of patients presenting with abdominal pain on AVASTIN. AVASTIN therapy should be permanently discontinued in patients with gastrointestinal perforation or wound dehiscence requiring medical intervention. The appropriate interval between termination of AVASTIN and subsequent elective surgery required to avoid the risks of impaired wound healing/wound dehiscence has not been determined. (See WARNINGS : Gastrointestinal Perforations/Wound Healing Complications and DOSAGE AND ADMINISTRATION : Dose Modifications ).
Hemorrhage
Serious, and in some cases fatal, hemoptysis has occurred in patients with non-small cell lung cancer treated with chemotherapy and AVASTIN. In a small study, the incidence of serious or fatal hemoptysis was 31% in patients with squamous histology and 4% in patients with adenocarcinoma receiving AVASTIN as compared to no cases in patients treated with chemotherapy alone. Patients with recent hemoptysis should not receive AVASTIN. (See WARNINGS : Hemorrhage and DOSAGE AND ADMINISTRATION : Dose Modifications ).
DESCRIPTION
AVASTIN™ (Bevacizumab) is a recombinant humanized monoclonal IgG1 antibody that binds to and inhibits the biologic activity of human vascular endothelial growth factor (VEGF) in in vitro and in vivo assay systems. Bevacizumab contains human framework regions and the complementarity-determining regions of a murine antibody that binds to VEGF ( 1 ). Bevacizumab is produced in a Chinese Hamster Ovary mammalian cell expression system in a nutrient medium containing the antibiotic gentamicin and has a molecular weight of approximately 149 kilodaltons. AVASTIN is a clear to slightly opalescent, colorless to pale brown, sterile, pH 6.2 solution for intravenous (IV) infusion. AVASTIN is supplied in 100 mg and 400 mg preservative-free, single-use vials to deliver 4 mL or 16 mL of AVASTIN (25 mg/mL). The 100 mg product is formulated in 240 mg (alpha),(alpha)-trehalose dihydrate, 23.2 mg sodium phosphate (monobasic, monohydrate), 4.8 mg sodium phosphate (dibasic, anhydrous), 1.6 mg polysorbate 20, and Water for Injection, USP. The 400 mg product is formulated in 960 mg (alpha),(alpha)-trehalose dihydrate, 92.8 mg sodium phosphate (monobasic, monohydrate), 19.2 mg sodium phosphate (dibasic, anhydrous), 6.4 mg polysorbate 20, and Water for Injection, USP.
CLINICAL PHARMACOLOGY
Mechanism of Action
Bevacizumab binds VEGF and prevents the interaction of VEGF to its receptors (Flt-1 and KDR) on the surface of endothelial cells. The interaction of VEGF with its receptors leads to endothelial cell proliferation and new blood vessel formation in in vitro models of angiogenesis. Administration of Bevacizumab to xenotransplant models of colon cancer in nude (athymic) mice caused reduction of microvascular growth and inhibition of metastatic disease progression.
Pharmacokinetics
The pharmacokinetic profile of Bevacizumab was assessed using an assay that measures total serum Bevacizumab concentrations (i.e., the assay did not distinguish between free Bevacizumab and Bevacizumab bound to VEGF ligand). Based on a population pharmacokinetic analysis of 491 patients who received 1 to 20 mg/kg of AVASTIN weekly, every 2 weeks, or every 3 weeks, the estimated half-life of Bevacizumab was approximately 20 days (range 11-50 days). The predicted time to reach steady state was 100 days. The accumulation ratio following a dose of 10 mg/kg of Bevacizumab every 2 weeks was 2.8.
The clearance of Bevacizumab varied by body weight,by gender, and by tumor burden. After correcting for body weight, males had a higher Bevacizumab clearance (0.262 L/day vs. 0.207 L/day) and a larger V c (3.25 L vs. 2.66 L) than females. Patients with higher tumor burden (at or above median value of tumor surface area) had a higher Bevacizumab clearance (0.249 L/day vs. 0.199 L/day) than patients with tumor burdens below the median. In a randomized study of 813 patients (Study 1), there was no evidence of lesser efficacy (hazard ratio for overall survival) in males or patients with higher tumor burden treated with AVASTIN as compared to females and patients with low tumor burden. The relationship between Bevacizumab exposure and clinical outcomes has not been explored.
Special Populations
Analyses of demographic data suggest that no dose adjustments are necessary for age or sex.
Patients with renal impairment. No studies have been conducted to examine the pharmacokinetics of Bevacizumab in patients with renal impairment.
Patients with hepatic dysfunction. No studies have been conducted to examine the pharmacokinetics of Bevacizumab in patients with hepatic impairment.
CLINICAL STUDIES
The safety and efficacy of AVASTIN in the initial treatment of patients with metastatic carcinoma of the colon or rectum were studied in two randomized, controlled clinical trials in combination with intravenous 5-fluorouracil-based chemotherapy.
AVASTIN in Combination with Bolus-IFL
Study 1 was a randomized, double-blind, active-controlled clinical trial evaluating AVASTIN as first-line treatment of metastatic carcinoma of the colon or rectum. Patients were randomized to bolus-IFL (irinotecan 125 mg/m 2 IV, 5-fluorouracil 500 mg/m 2 IV, and leucovorin 20 mg/m 2 IV given once weekly for 4 weeks every 6 weeks) plus placebo (Arm 1), bolus-IFL plus AVASTIN (5 mg/kg every 2 weeks) (Arm 2), or 5-FU/LV plus AVASTIN (5 mg/kg every 2 weeks) (Arm 3). Enrollment in Arm 3 was discontinued, as pre-specified, when the toxicity of AVASTIN in combination with the bolus-IFL regimen was deemed acceptable.
Of the 813 patients randomized to Arms 1 and 2, the median age was 60, 40% were female, and 79% were Caucasian. Fifty-seven percent had an ECOG performance status of 0. Twenty-one percent had a rectal primary and 28% received prior adjuvant chemotherapy. In the majority of patients, 56%, the dominant site of disease was extra-abdominal, while the liver was the dominant site in 38% of patients. The patient characteristics were similar across the study arms. The primary endpoint of this trial was overall survival. Results are presented in Table 1 and Figure 1.
Table 1
Study 1 Efficacy ResultsIFL + Placebo IFL + AVASTIN
5 mg/kg
q 2 wksNumber of Patients411 402 Overall Survival aMedian (months)15.6 20.3 Hazard ratio0.66 Progression-Free Survival aMedian (months)6.2 10.6 Hazard ratio0.54 Overall Response Rate bRate (percent)35% 45% Duration of ResponseMedian (months)7.1 10.4 a p<0.001 by stratified logrank test.b p<0.01 by [khgr ] 2 test.
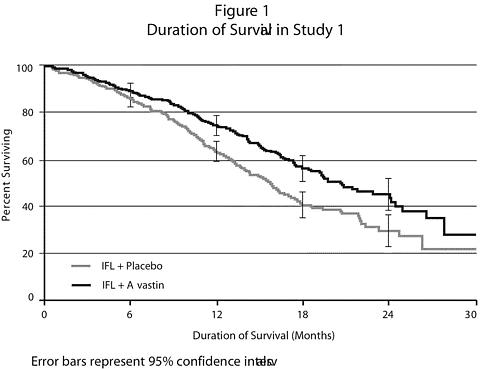
The clinical benefit of AVASTIN, as measured by survival in the two principal arms, was seen in all subgroups tested. The subgroups examined were based on age, sex, race, ECOG performance status, location of primary tumor, prior adjuvant therapy, number of metastatic sites, and tumor burden.
Among the 110 patients enrolled in Arm 3, median overall survival was 18.3 months, median progression-free survival was 8.8 months, overall response rate was 39%, and median duration of response was 8.5 months.
AVASTIN in Combination with 5-FU/LV Chemotherapy
Study 2 was a randomized, active-controlled clinical trial testing AVASTIN in combination with 5-FU/LV as first-line treatment of metastatic colorectal cancer. Patients were randomized to receive 5-FU/LV (5-fluorouracil 500 mg/m 2 , leucovorin 500 mg/m 2 weekly for 6 weeks every 8 weeks) or 5-FU/LV plus AVASTIN (5 mg/kg every 2 weeks) or 5-FU/LV plus AVASTIN (10 mg/kg every 2 weeks). Patients were treated until disease progression. The primary endpoints of the trial were objective response rate and progression-free survival. Results are presented in Table 2.
Table 2
Study 2 Efficacy Results5-FU/LV 5-FU/LV +
AVASTIN 5 mg/kg5-FU/LV +
AVASTIN 10 mg/kgNumber of Patients36 35 33 Overall SurvivalMedian (months)13.6 17.7 15.2 Progression-Free SurvivalMedian (months)5.2 9.0 7.2 Overall Response RateRate (percent)17 40 24 Progression-free survival was significantly better in patients receiving 5-FU/LV plus AVASTIN at 5 mg/kg when compared to those not receiving AVASTIN. However, overall survival and overall response rate were not significantly different. Outcomes for patients receiving 5-FU/LV plus AVASTIN at 10 mg/kg were not significantly different than for patients who did not receive AVASTIN.
AVASTIN as a Single Agent
The efficacy of AVASTIN as a single agent in colorectal cancer has not been established. However, in an ongoing, randomized study of patients with metastatic colorectal cancer that had progressed following a 5-fluorouracil and irinotecan-based regimen, the arm in which patients were treated with single-agent AVASTIN was closed early due to evidence of an inferior survival in that arm as compared with patients treated with the FOLFOX regimen of 5-fluorouracil, leucovorin, and oxaliplatin.
INDICATIONS AND USAGE
AVASTIN, used in combination with intravenous 5-fluorouracil-based chemotherapy, is indicated for first-line treatment of patients with metastatic carcinoma of the colon or rectum.
CONTRAINDICATIONS
There are no known contraindications to the use of AVASTIN.
WARNINGS
Gastrointestinal Perforations/Wound Healing Complications (See DOSAGE AND ADMINISTRATION : Dose Modifications )
Gastrointestinal perforation and wound dehiscence, complicated by intra-abdominal abscesses, occurred at an increased incidence in patients receiving AVASTIN as compared to controls. AVASTIN has also been shown to impair wound healing in pre-clinical animal models.
In Study 1, one of 396 (0.3%) patients receiving bolus-IFL plus placebo, six of 392 (2%) patients receiving bolus-IFL plus AVASTlN, and four of 109 (4%) patients receiving 5-FU/LV plus AVASTIN developed gastrointestinal perforation, in some instances with fatal outcome. These episodes occurred with or without intra-abdominal abscesses and at various time points during treatment. The typical presentation was reported as abdominal pain associated with symptoms such as constipation and vomiting.
In addition, two of 396 (0.5%) patients receiving bolus-IFL plus placebo, four of 392 (1%) patients receiving bolus-IFL plus AVASTIN, and one of 109 (1%) patients receiving 5-FU/LV plus AVASTIN developed a wound dehiscence during study treatment.
The appropriate interval between surgery and subsequent initiation of AVASTIN required to avoid the risks of impaired wound healing has not been determined. In Study 1, the clinical protocol did not permit initiation of AVASTIN for at least 28 days following surgery. There was one patient (among 501 patients receiving AVASTIN on Study 1) in whom an anastomotic dehiscence occurred when AVASTIN was initiated per protocol. In this patient, the interval between surgery and initiation of AVASTIN was greater than 2 months.
Similarly, the appropriate interval between termination of AVASTIN and subsequent elective surgery required to avoid the risks of impaired wound healing has not been determined. In Study 1, 39 patients who were receiving bolus-IFL plus AVASTIN underwent surgery following AVASTIN therapy and, of these patients, six (15%) had wound healing/bleeding complications. In the same study, 25 patients in the bolus-IFL arm underwent surgery and, of these patients, one of 25 (4%) had wound healing/bleeding complications. The longest interval between last dose of study drug and dehiscence was 56 days; this occurred in a patient on the bolus-IFL plus AVASTIN arm. The interval between termination of AVASTIN and subsequent elective surgery should take into consideration the calculated half-life of AVASTIN (approximately 20 days).
AVASTIN therapy should be discontinued in patients with gastrointestinal perforation or wound dehiscence requiring medical intervention.
Hemorrhage (See DOSAGE AND ADMINISTRATION : Dose Modifications )
Two distinct patterns of bleeding have occurred in patients receiving AVASTIN. The first is minor hemorrhage, most commonly Grade 1 epistaxis. The second is serious, and in some cases fatal, hemorrhagic events. Serious hemorrhagic events occurred primarily in patients with non-small cell lung cancer, an indication for which AVASTIN is not approved. In a randomized study in patients with non-small cell lung cancer receiving chemotherapy with or without AVASTIN, four of 13 (31%) AVASTIN-treated patients with squamous cell histology and two of 53 (4%) AVASTIN-treated patients with non-squamous histology experienced life-threatening or fatal pulmonary hemorrhage as compared to none of the 32 (0%) patients receiving chemotherapy alone. Of the patients experiencing events of life-threatening pulmonary hemorrhage, many had cavitation and/or necrosis of the tumor, either pre-existing or developing during AVASTIN therapy. These serious hemorrhagic events occurred suddenly and presented as major or massive hemoptysis.
The risk of central nervous system (CNS) bleeding in patients with CNS metastases receiving AVASTIN has not been evaluated because these patients were excluded from Genentech-sponsored studies following development of CNS hemorrhage in a patient with a CNS metastasis in Phase 1 studies.
Other serious bleeding events reported in patients receiving AVASTIN were uncommon and included gastrointestinal hemorrhage, subarachnoid hemorrhage, and hemorrhagic stroke.
Patients with serious hemorrhage i.e., requiring medical intervention, should have AVASTIN treatment discontinued and receive aggressive medical management. Patients with recent hemoptysis should not receive AVASTIN.
Arterial Thromboembolic Events (see DOSAGE AND ADMINISTRATION : Dose Modifications , and PRECAUTIONS : Geriatric Use )
Arterial thromboembolic events occurred at a higher incidence in patients receiving AVASTIN in combination with chemotherapy as compared to those receiving chemotherapy alone. Arterial thromboembolic events included cerebral infarction, transient ischemic attacks (TIAs), myocardial infarction (MI), angina, and a variety of other arterial thromboembolic events. These events were fatal in some instances.
In an exploratory analysis pooling the data from five randomized, controlled, clinical trials involving 1745 patients, the overall incidence of arterial thromboembolic events was increased (4.4% vs. 1.9%) among the 963 patients treated with AVASTIN in combination with chemotherapy as compared to 782 patients treated with chemotherapy alone. Fatal outcomes from arterial thromboembolic events occurred in 7 of 963 patients (0.7%) who were treated with AVASTIN in combination with chemotherapy, compared to 3 of 782 patients (0.4%) who were treated with chemotherapy alone. The incidences of both cerebrovascular arterial events (1.9% vs. 0.5%) and cardiovascular arterial events (2.1% vs. 1.0%) were increased in patients receiving AVASTIN. In addition, there was a correlation between age (65 years and over) and the increase in risk of thromboembolic events (See PRECAUTIONS : Geriatric Use ).
The safety of resumption of AVASTIN therapy after resolution of an arterial thromboembolic event has not been studied. AVASTIN therapy should be permanently discontinued in patients who experience a severe arterial thromboembolic event during treatment.
Hypertension (See DOSAGE AND ADMINISTRATION : Dose Modifications )
The incidence of hypertension and severe hypertension was increased in patients receiving AVASTIN in Study 1 (see Table 3).
Table 3
Incidence of Hypertension and Severe
Hypertension in Study 1Arm 1
IFL +
Placebo
(n = 394)Arm 2
IFL +
AVASTIN
(n = 392)Arm 3
5-FU/LV +
AVASTIN
(n = 109)Hypertension a
(>150/100 mmHg)43% 60% 67% Severe
Hypertension a
(>200/110 mmHg)2% 7% 10% a This includes patients with either a systolic or diastolic reading greater than the cutoff value on one or more occasions.
Among patients with severe hypertension in the AVASTIN arms, slightly over half the patients (51%) had a diastolic reading greater than 110 associated with a systolic reading less than 200.
Medication classes used for management of patients with Grade 3 hypertension receiving AVASTIN included angiotensin-converting enzyme inhibitors, beta blockers, diuretics, and calcium channel blockers. Four months after discontinuation of therapy, persistent hypertension was present in 18 of 26 patients that received bolus-IFL plus AVASTIN and 8 of 10 patients that received bolus-IFL plus placebo.
Across pooled clinical studies (n=1032), development or worsening of hypertension resulted in hospitalization or discontinuation of AVASTIN in 17 patients. Four of these 17 patients developed hypertensive encephalopathy. Severe hypertension was complicated by subarachnoid hemorrhage in one patient.
In the post-marketing experience, acute increases in blood pressure associated with initial or subsequent infusions of AVASTIN have been reported (see PRECAUTIONS , Infusion Reactions ). Some cases were serious and associated with clinical sequelae.
AVASTIN should be permanently discontinued in patients with hypertensive crisis. Temporary suspension is recommended in patients with severe hypertension that is not controlled with medical management.
Proteinuria (See DOSAGE AND ADMINISTRATION : Dose Modifications )
In Study 1, both the incidence and severity of proteinuria (defined as a urine dipstick reading of 1+ or greater) was increased in patients receiving AVASTIN as compared to those receiving bolus-IFL plus placebo. Urinary dipstick readings of 2+ or greater occurred in 14% of patients receiving bolus-IFL plus placebo, 17% receiving bolus-IFL plus AVASTIN, and in 28% of patients receiving 5-FU/LV plus AVASTIN. Twenty-four-hour urine collections were obtained in patients with new onset or worsening proteinuria. None of the 118 patients receiving bolus-IFL plus placebo, three of 158 patients (2%) receiving bolus-IFL plus AVASTIN, and two of 50 (4%) patients receiving 5-FU/LV plus AVASTIN who had a 24-hour collection experienced NCI-CTC Grade 3 proteinuria (>3.5 gm protein/24 hours).
In a dose-ranging, placebo-controlled, randomized study of AVASTIN in patients with metastatic renal cell carcinoma, an indication for which AVASTIN is not approved, 24-hour urine collections were obtained in approximately half the patients enrolled. Among patients in whom 24-hour urine collections were obtained, four of 19 (21%) patients receiving AVASTIN at 10 mg/kg every two weeks, two of 14 (14%) receiving AVASTIN at 3 mg/kg every two weeks, and none of the 15 placebo patients experienced NCI-CTC Grade 3 proteinuria (>3.5 gm protein/24 hours).
Nephrotic syndrome occurred in five of 1032 (0.5%) patients receiving AVASTIN in Genentech-sponsored studies. One patient died and one required dialysis. In three patients, proteinuria decreased in severity several months after discontinuation of AVASTIN. No patient had normalization of urinary protein levels (by 24-hour urine) following discontinuation of AVASTIN.
AVASTIN should be discontinued in patients with nephrotic syndrome. The safety of continued AVASTIN treatment in patients with moderate to severe proteinuria has not been evaluated. In most clinical studies, AVASTIN was interrupted for >/=2 grams of proteinuria/24 hours and resumed when proteinuria was <2 gm/24 hours. Patients with moderate to severe proteinuria based on 24-hour collections should be monitored regularly until improvement and/or resolution is observed.
Congestive Heart Failure
Congestive heart failure (CHF), defined as NCI-CTC Grade 2-4 left ventricular dysfunction, was reported in 22 of 1032 (2%) patients receiving AVASTIN in Genentech-sponsored studies. Congestive heart failure occurred in six of 44 (14%) patients receiving AVASTIN and concurrent anthracyclines. Congestive heart failure occurred in 13 of 299 (4%) patients who received prior anthracyclines and/or left chest wall irradiation. In a controlled study, the incidence was higher in patients receiving AVASTIN plus chemotherapy as compared to patients receiving chemotherapy alone. The safety of continuation or resumption of AVASTIN in patients with cardiac dysfunction has not been studied.
PRECAUTIONS
General
AVASTIN should be used with caution in patients with known hypersensitivity to AVASTIN or any component of this drug product.
Infusion Reactions
In clinical studies, infusion reactions with the first dose of AVASTIN were uncommon (<3%) and severe reactions occurred in 0.2% of patients. Infusion reactions reported in the clinical trials and postmarketing experience include hypertension, hypertensive crises associated with neurologic signs and symptoms, wheezing, oxygen desaturation, Grade 3 hypersensitivity, chest pain, headaches, rigors, and diaphoresis. Adequate information on rechallenge is not available. AVASTIN infusion should be interrupted in all patients with severe infusion reactions and appropriate medical therapy administered.
There are no data regarding the most appropriate method of identification of patients who may safely be retreated with AVASTIN after experiencing a severe infusion reaction.
Surgery
AVASTIN therapy should not be initiated for at least 28 days following major surgery. The surgical incision should be fully healed prior to initiation of AVASTIN. Because of the potential for impaired wound healing, AVASTIN should be suspended prior to elective surgery. The appropriate interval between the last dose of AVASTIN and elective surgery is unknown; however, the half-life of AVASTIN is estimated to be 20 days (see CLINICAL PHARMACOLOGY : Pharmacokinetics ) and the interval chosen should take into consideration the half-life of the drug. (See WARNINGS : Gastrointestinal Perforations/Wound Healing Complications ).
Cardiovascular Disease
Patients were excluded from participation in AVASTIN clinical trials if, in the previous year, they had experienced clinically significant cardiovascular disease. In an exploratory analysis pooling the data from five randomized, placebo-controlled, clinical trials conducted in patients without a recent history of clinically significant cardiovascular disease, the overall incidence of arterial thromboembolic events, the incidence of fatal arterial thromboembolic events, and the incidence of cardiovascular thromboembolic events were increased in patients receiving AVASTIN plus chemotherapy as compared to chemotherapy alone.
Immunogenicity
As with all therapeutic proteins, there is a potential for immunogenicity. The incidence of antibody development in patients receiving AVASTIN has not been adequately determined because the assay sensitivity was inadequate to reliably detect lower titers. Enzyme-linked immunosorbent assays (ELISAs) were performed on sera from approximately 500 patients treated with AVASTIN, primarily in combination with chemotherapy. High titer human anti-AVASTIN antibodies were not detected.
Immunogenicity data are highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody positivity in an assay may be influenced by several factors, including sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies to AVASTIN with the incidence of antibodies to other products may be misleading.
Laboratory Tests
Blood pressure monitoring should be conducted every two to three weeks during treatment with AVASTIN. Patients who develop hypertension on AVASTIN may require blood pressure monitoring at more frequent intervals. Patients with AVASTIN-induced or -exacerbated hypertension who discontinue AVASTIN should continue to have their blood pressure monitored at regular intervals.
Patients receiving AVASTIN should be monitored for the development or worsening of proteinuria with serial urinalyses. Patients with a 2+ or greater urine dipstick reading should undergo further assessment, e.g., a 24-hour urine collection. (See WARNINGS : Proteinuria and DOSAGE AND ADMINISTRATION : Dose Modifications ).
Drug Interactions
No formal drug interaction studies with anti-neoplastic agents have been conducted. In Study 1, patients with colorectal cancer were given irinotecan/5-FU/leucovorin (bolus-IFL) with or without AVASTIN. Irinotecan concentrations were similar in patients receiving bolus-IFL alone and in combination with AVASTIN. The concentrations of SN38, the active metabolite of irinotecan, were on average 33% higher in patients receiving bolus-IFL in combination with AVASTIN when compared with bolus-IFL alone. In Study 1, patients receiving bolus-IFL plus AVASTIN had a higher incidence of Grade 3-4 diarrhea and neutropenia. Due to high inter-patient variability and limited sampling, the extent of the increase in SN38 levels in patients receiving concurrent irinotecan and AVASTIN is uncertain.
Carcinogenesis, Mutagenesis, Impairment of Fertility
No carcinogenicity data are available for AVASTIN in animals or humans.
AVASTIN may impair fertility. Dose-related decreases in ovarian and uterine weights, endometrial proliferation, number of menstrual cycles, and arrested follicular development or absent corpora lutea were observed in female cynomolgus monkeys treated with 10 or 50 mg/kg of AVASTIN for 13 or 26 weeks. Following a 4- or 12-week recovery period, which examined only the high-dose group, trends suggestive of reversibility were noted in the two females for each regimen that were assigned to recover. After the 12-week recovery period, follicular maturation arrest was no longer observed, but ovarian weights were still moderately decreased. Reduced endometrial proliferation was no longer observed at the 12-week recovery time point, but uterine weight decreases were still notable, corpora lutea were absent in 1 out of 2 animals, and the number of menstrual cycles remained reduced (67%).
Pregnancy Category C
AVASTIN has been shown to be teratogenic in rabbits when administered in doses that are two-fold greater than the recommended human dose on a mg/kg basis. Observed effects included decreases in maternal and fetal body weights, an increased number of fetal resorptions, and an increased incidence of specific gross and skeletal fetal alterations. Adverse fetal outcomes were observed at all doses tested.
Angiogenesis is critical to fetal development and the inhibition of angiogenesis following administration of AVASTIN is likely to result in adverse effects on pregnancy. There are no adequate and well-controlled studies in pregnant women. AVASTIN should be used during pregnancy or in any woman not employing adequate contraception only if the potential benefit justifies the potential risk to the fetus. All patients should be counseled regarding the potential risk of AVASTIN to the developing fetus prior to initiation of therapy. If the patient becomes pregnant while receiving AVASTIN, she should be apprised of the potential hazard to the fetus and/or the potential risk of loss of pregnancy. Patients who discontinue AVASTIN should also be counseled concerning the prolonged exposure following discontinuation of therapy (half-life of approximately 20 days) and the possible effects of AVASTIN on fetal development.
Nursing Mothers
It is not known whether AVASTIN is secreted in human milk. Because human IgG1 is secreted into human milk, the potential for absorption and harm to the infant after ingestion is unknown. Women should be advised to discontinue nursing during treatment with AVASTIN and for a prolonged period following the use of AVASTIN, taking into account the half-life of the product, approximately 20 days [range 11-50 days]. (See CLINICAL PHARMACOLOGY : Pharmacokinetics ).
Pediatric Use
The safety and effectiveness of AVASTIN in pediatric patients has not been studied. However, physeal dysplasia was observed in juvenile cynomolgus monkeys with open growth plates treated for four weeks with doses that were less than the recommended human dose based on mg/kg and exposure. The incidence and severity of physeal dysplasia were dose-related and were at least partially reversible upon cessation of treatment.
Geriatric Use
In Study 1,NCI-CTC Grade 3-4 adverse events were collected in all patients receiving study drug (396 bolus-IFL plus placebo; 392 bolus-IFL plus AVASTIN; 109 5-FU/LV plus AVASTIN), while NCI-CTC Grade 1 and 2 adverse events were collected in a subset of 309 patients. There were insufficient numbers of patients 65 years and older in the subset in which Grade 1-4 adverse events were collected to determine whether the overall adverse event profile was different in the elderly as compared to younger patients. Among the 392 patients receiving bolus-IFL plus AVASTIN, 126 were at least 65 years of age. Severe adverse events that occurred at a higher incidence (>/=2%) in the elderly when compared to those less than 65 years were asthenia, sepsis, deep thrombophlebitis, hypertension, hypotension, myocardial infarction, congestive heart failure, diarrhea, constipation, anorexia, leukopenia, anemia, dehydration, hypokalemia, and hyponatremia. The effect of AVASTIN on overall survival was similar in elderly patients as compared to younger patients.
Of the 742 patients enrolled in Genentech-sponsored clinical studies in which all adverse events were captured, 212 (29%) were age 65 or older and 43 (6%) were age 75 or older. Adverse events of any severity that occurred at a higher incidence in the elderly as compared to younger patients, in addition to those described above, were dyspepsia, gastrointestinal hemorrhage, edema, epistaxis, increased cough, and voice alteration.
In an exploratory, pooled analysis of 1745 patients treated in five randomized, controlled studies, there were 618 (35%) patients age 65 or older and 1127 patients less than 65 years of age. The overall incidence of arterial thromboembolic events was increased in all patients receiving AVASTIN with chemotherapy as compared to those receiving chemotherapy alone, regardless of age. However, the increase in arterial thromboembolic events incidence was greater in patients 65 and over (8.5% vs. 2.9%) as compared to those less than 65 (2.1% vs. 1.4%). (See WARNINGS : Arterial Thromboembolic Events )
ADVERSE EVENTS
The most serious adverse events associated with AVASTIN were:
- Gastrointestinal Perforations/Wound Healing Complications (see WARNINGS )
- Hemorrhage (see WARNINGS )
- Arterial Thromboembolic Events (see WARNINGS )
- Hypertensive Crises (see WARNINGS ; Hypertension )
- Nephrotic Syndrome (see WARNINGS ; Proteinuria )
- Congestive Heart Failure (see WARNINGS )
The most common severe (NCI-CTC Grade 3-4) adverse events among 1032 patients receiving AVASTIN in Genentech-sponsored studies were asthenia, pain, hypertension, diarrhea, and leukopenia.
The most common adverse events of any severity among 742 patients receiving AVASTIN in Genentech-sponsored studies were asthenia, pain, abdominal pain, headache, hypertension, diarrhea, nausea, vomiting, anorexia, stomatitis, constipation, upper respiratory infection, epistaxis, dyspnea, exfoliative dermatitis, and proteinuria.
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. The adverse reaction information from clinical trials does, however, provide a basis for identifying the adverse events that appear to be related to drug use and for approximating rates.
In pooled safety data, 1032 patients with metastatic colorectal cancer (n=568) and with other cancers (n=464) received AVASTIN either as a single agent (n=157) or in combination with chemotherapy (n=875) in Genentech-sponsored clinical trials. All adverse events were collected in 742 of the 1032 patients; for the remaining 290, all NCI-CTC Grade 3 and 4 adverse events and only selected Grade 1 and 2 adverse events (hypertension, proteinuria, thromboembolic events) were collected. Adverse events across all Genentech-sponsored studies were used to further characterize specific adverse events. (See WARNINGS : Hemorrhage , Arterial Thromboembolic Events , Hypertension , Proteinuria , Congestive Heart Failure and PRECAUTIONS : Geriatric Use ).
Comparative data on adverse experiences, except where indicated, are limited to Study 1, a randomized, active-controlled study in 897 patients receiving initial treatment for metastatic colorectal cancer. All NCI-CTC Grade 3 and 4 adverse events and selected Grade 1 and 2 adverse events (hypertension, proteinuria, thromboembolic events) were reported for the overall study population. In Study 1, the median age was 60, 60% were male, 78% had colon primary lesion, and 29% had prior adjuvant or neoadjuvant chemotherapy. The median duration of exposure to AVASTIN in Study 1 was 8 months in Arm 2 and 7 months in Arm 3. All adverse events, including all NCI-CTC Grade 1 and 2 events, were reported in a subset of 309 patients. The baseline entry characteristics in the 309 patient safety subset were similar to the overall study population and well-balanced across the three study arms.
Severe and life-threatening (NCI-CTC Grade 3 and 4) adverse events, which occurred at a higher incidence (>/=2%) in patients receiving bolus-IFL plus AVASTIN as compared to bolus-IFL plus placebo, are presented in Table 4.
Table 4
NCI-CTC Grade 3 and 4 Adverse Events in Study 1
(Occurring at Higher Incidence (>/=2%) in AVASTIN vs. Control)Arm 1
IFL + Placebo
(n = 396)Arm 2
IFL + AVASTIN
(n = 392)Grade 3-4 Events295 (74%) 340 (87%) Body as a WholeAsthenia28 (7%) 38 (10%) Abdominal Pain20 (5%) 32 (8%) Pain21 (5%) 30 (8%) CardiovascularDeep Vein Thrombosis19 (5%) 34 (9%) Hypertension10 (2%) 46 (12%) Intra-Abdominal Thrombosis5 (1%) 13 (3%) Syncope4 (1%) 11 (3%) DigestiveDiarrhea99 (25%) 133 (34%) Constipation9 (2%) 14 (4%) Hemic/LymphaticLeukopenia122 (31%) 145 (37%) Neutropenia a41 (14%) 58 (21%) a Central laboratories were collected on Days 1 and 21 of each cycle. Neutrophil counts are available in 303 patients in Arm 1 and 276 in Arm 2.Adverse events of any severity,which occurred at a higher incidence (>/=5%) in the initial phase of the study in patients receiving AVASTIN (bolus-IFL plus AVASTIN or 5-FU/LV plus AVASTIN) as compared to the bolus-IFL plus placebo arm, are presented in Table 5.
Table 5
NCI-CTC Grade 1-4 Adverse Events in Study 1 Subset
(Occurring at Higher Incidence (>/=5%) in AVASTIN vs. Control)Arm 1
IFL + Placebo
(n = 98)Arm 2
IFL + AVASTIN
(n = 102)Arm 3
5-FU/LV + AVASTIN
(n = 109)Body as a WholeAsthenia68 (70%)75 (74%)80 (73%)Pain54 (55%)62 (61%)67 (62%)Abdominal Pain54 (55%)62 (61%)55 (50%)Headache19 (19%)27 (26%)30 (26%)CardiovascularHypertension14 (14%)23 (23%)37 (34%)Hypotension7 (7%)15 (15%)8 (7%)Deep Vein Thrombosis3 (3%)9 (9%)6 (6%)DigestiveVomiting46 (47%)53 (52%)51 (47%)Anorexia29 (30%)44 (43%)38 (35%)Constipation28 (29%)41 (40%)32 (29%)Stomatitis18 (18%)33 (32%)33 (30%)Dyspepsia15 (15%)25 (24%)19 (17%)Weight Loss10 (10%)15 (15%)18 (16%)Flatulence10 (10%)11 (11%)21 (19%)GI Hemorrhage6 (6%)25 (24%)21 (19%)Dry Mouth2 (2%)7 (7%)4 (4%)Colitis1 (1%)6 (6%)1 (1%)Hemic/LymphaticThrombocytopenia05 (5%)5 (5%)Metabolic/NutritionHypokalemia11 (11%)12 (12%)18 (16%)Bilirubinemia01 (1%)7 (6%)MusculoskeletalMyalgia7 (7%)8 (8%)16 (15%)NervousDizziness20 (20%)27 (26%)21 (19%)Confusion1 (1%)1 (1%)6 (6%)Abnormal Gait01 (1%)5 (5%)RespiratoryUpper Respiratory Infection38 (39%)48 (47%)44 (40%)Dyspnea15 (15%)26 (26%)27 (25%)Epistaxis10 (10%)36 (35%)35 (32%)Voice Alteration2 (2%)9 (9%)6 (6%)Skin/AppendagesAlopecia25 (26%)33 (32%)6 (6%)Dry Skin7 (7%)7 (7%)22 (20%)Exfoliative Dermatitis3 (3%)3 (3%)21 (19%)Nail Disorder3 (3%)2 (2%)9 (8%)Skin Discoloration3 (3%)2 (2%)17 (16%)Skin Ulcer1 (1%)6 (6%)7 (6%)Special SensesTaste Disorder9 (9%)14 (14%)23 (21%)Excess Lacrimation2 (2%)6 (6%)20 (18%)UrogenitalProteinuria24 (24%)37 (36%)39 (36%)Urinary Frequency/Urgency1 (1%)3 (3%)6 (6%)Mucocutaneous Hemorrhage
In Study 1, both serious and non-serious hemorrhagic events occurred at a higher incidence in patients receiving AVASTIN. (See WARNINGS : Hemorrhage ). In the 309 patients in which Grade 1-4 events were collected, epistaxis was common and reported in 35% of patients receiving bolus-IFL plus AVASTIN compared with 10% of patients receiving bolus-IFL plus placebo. These events were generally mild in severity (NCI-CTC Grade 1) and resolved without medical intervention. Other mild to moderate hemorrhagic events reported more frequently in patients receiving bolus-IFL plus AVASTIN when compared to those receiving bolus-IFL plus placebo included gastrointestinal hemorrhage (24% vs. 6%), minor gum bleeding (2% vs. 0), and vaginal hemorrhage (4% vs. 2%).
Venous Thromboembolic Events
In Study 1, 15.1% of patients receiving bolus-IFL plus AVASTIN and 13.6% of patients receiving bolus-IFL plus placebo experienced a Grade 3-4 venous thromboembolic event. The incidence of the following Grade 3 and 4 venous thromboembolic events was higher in patients receiving bolus-IFL plus AVASTIN as compared to patients receiving bolus-IFL plus placebo: deep venous thrombosis (34 vs. 19 patients) and intra-abdominal venous thrombosis (10 vs. 5 patients). The incidence of pulmonary embolism was higher in patients receiving bolus-IFL plus placebo (16 vs. 20 patients).
In Study 1, 53 of 392 (14%) patients who received bolus-IFL plus AVASTIN and 30 of 396 (8%) patients who received bolus-IFL plus placebo had a thromboembolic event and received full-dose warfarin. Two patients in each treatment arm (four total) developed bleeding complications. In the two patients treated with full-dose warfarin and AVASTIN, these events were associated with marked elevations in their INR. Eleven of 53 (21%) patients receiving bolus-IFL plus AVASTIN and one of 30 (3%) patients receiving bolus-IFL developed an additional thromboembolic event.
Other Serious Adverse Events
The following other serious adverse events are considered unusual in cancer patients receiving cytotoxic chemotherapy and occurred in at least one subject treated with AVASTIN in clinical studies.
Body as a Whole: polyserositis
Digestive: intestinal obstruction, intestinal necrosis, mesenteric venous occlusion, anastomotic ulceration
Hemic and lymphatic: pancytopenia
Metabolic and nutritional disorders: hyponatremia.
Urogenital: ureteral stricture
OVERDOSAGE
The maximum tolerated dose of AVASTIN has not been determined. The highest dose tested in humans (20 mg/kg IV) was associated with headache in nine of 16 patients and with severe headache in three of 16 patients.
DOSAGE AND ADMINISTRATION
The recommended dose of AVASTIN is 5 mg/kg given once every 14 days as an IV infusion until disease progression is detected.
AVASTIN therapy should not be initiated for at least 28 days following major surgery. The surgical incision should be fully healed prior to initiation of AVASTIN.
Dose Modifications
There are no recommended dose reductions for the use of AVASTIN. If needed, AVASTIN should be either discontinued or temporarily suspended as described below.
AVASTIN should be permanently discontinued in patients who develop gastrointestinal perforation, wound dehiscence requiring medical intervention, serious bleeding, a severe arterial thromboembolic event, nephrotic syndrome, or hypertensive crisis.
Temporary suspension of AVASTIN is recommended in patients with evidence of moderate to severe proteinuria pending further evaluation and in patients with severe hypertension that is not controlled with medical management. The risk of continuation or temporary suspension of AVASTIN in patients with moderate to severe proteinuria is unknown.
AVASTIN should be suspended at least several weeks prior to elective surgery. (See WARNINGS : Gastrointestinal Perforation/Wound Healing Complications and PRECAUTIONS : Surgery ). AVASTIN should not be resumed until the surgical incision is fully healed.
Preparation for Administration
AVASTIN should be diluted for infusion by a healthcare professional using aseptic technique. Withdraw the necessary amount of AVASTIN for a dose of 5 mg/kg and dilute in a total volume of 100 mL of 0.9% Sodium Chloride Injection, USP. Discard any unused portion left in a vial, as the product contains no preservatives. Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration.
Diluted AVASTIN solutions for infusion may be stored at 2-8°C (36-46°F) for up to 8 hours. No incompatibilities between AVASTIN and polyvinylchloride or polyolefin bags have been observed.
AVASTIN infusions should not be administered or mixed with dextrose solutions.
Administration
DO NOT ADMINISTER AS AN IV PUSH OR BOLUS. The initial AVASTIN dose should be delivered over 90 minutes as an IV infusion following chemotherapy. If the first infusion is well tolerated, the second infusion may be administered over 60 minutes. If the 60-minute infusion is well tolerated, all subsequent infusions may be administered over 30 minutes.
Stability and Storage
AVASTIN vials must be refrigerated at 2-8°C (36-46°F). AVASTIN vials should be protected from light. Store in the original carton until time of use. DO NOT FREEZE. DO NOT SHAKE.
HOW SUPPLIED
AVASTIN is supplied as 4 mL and 16 mL of a sterile solution in single-use glass vials to deliver 100 and 400 mg of Bevacizumab per vial, respectively.
Single unit 100 mg carton: Contains one 4 mL vial of AVASTIN (25 mg/mL). NDC 50242-060-01
Single unit 400 mg carton: Contains one 16 mL vial of AVASTIN (25 mg/mL). NDC 50242-061-01
REFERENCES
- Presta LG, Chen H, O'Connor SJ, Chisholm V, Meng YG, Krummen L, et al. Humanization of an anti-vascular endothelial growth factor monoclonal antibody for the therapy of solid tumors and other disorders. Cancer Res 1997;57:4593-9.
BIOONCOLOGY™
AVASTIN™
(Bevacizumab)
For Intravenous Use 7455303
Manufactured by:4829004
Genentech, Inc. FDA Approval Date: December 2004
1 DNA WayCode Revision Date: January 2005
South San Francisco, CA 94080-4990
©2004 Genentech, Inc.
Subscribe to the "News" RSS Feed 
TOP ۞
