-
Cancidas for Injection (Merck)
INTRAVENOUS INFUSION (not for IV Bolus Injection)
CANCIDAS®
(caspofungin acetate) FOR INJECTION
DESCRIPTION
CANCIDAS * is a sterile, lyophilized product for intravenous (IV) infusion that contains a semisynthetic lipopeptide (echinocandin) compound synthesized from a fermentation product of Glarea lozoyensis . CANCIDAS is the first of a new class of antifungal drugs (echinocandins) that inhibit the synthesis of (beta) (1,3)-D-glucan, an integral component of the fungal cell wall.
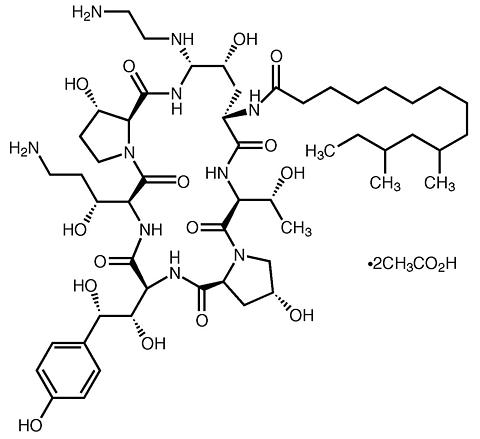
CANCIDAS (caspofungin acetate) is 1-[(4 R ,5 S )-5-[(2-aminoethyl)amino]- N 2 -(10,12-dimethyl-1-oxotetradecyl)-4-hydroxy-L-ornithine]-5-[(3 R )-3-hydroxy-L-ornithine] pneumocandin B 0 diacetate (salt). CANCIDAS 50 mg also contains: 39 mg sucrose, 26 mg mannitol, glacial acetic acid, and sodium hydroxide. CANCIDAS 70 mg also contains 54 mg sucrose, 36 mg mannitol, glacial acetic acid, and sodium hydroxide. Caspofungin acetate is a hygroscopic, white to off-white powder. It is freely soluble in water and methanol, and slightly soluble in ethanol. The pH of a saturated aqueous solution of caspofungin acetate is approximately 6.6. The empirical formula is C 52 H 88 N 10 O 15 ·2C 2 H 4 O 2 and the formula weight is 1213.42. The structural formula is:
*Registered trademark of Merck & CO., Inc.CLINICAL PHARMACOLOGY
Pharmacokinetics
Distribution
Plasma concentrations of caspofungin decline in a polyphasic manner following single 1-hour IV infusions. A short (alpha)-phase occurs immediately postinfusion, followed by a (beta)-phase (half-life of 9 to 11 hours) that characterizes much of the profile and exhibits clear log-linear behavior from 6 to 48 hours postdose during which the plasma concentration decreases 10-fold. An additional, longer half-life phase, (gamma)-phase, (half-life of 40-50 hours), also occurs. Distribution, rather than excretion or biotransformation, is the dominant mechanism influencing plasma clearance. Caspofungin is extensively bound to albumin (~97%), and distribution into red blood cells is minimal. Mass balance results showed that approximately 92% of the administered radioactivity was distributed to tissues by 36 to 48 hours after a single 70-mg dose of [ 3 H] caspofungin acetate. There is little excretion or biotransformation of caspofungin during the first 30 hours after administration.
Metabolism
Caspofungin is slowly metabolized by hydrolysis and N-acetylation. Caspofungin also undergoes spontaneous chemical degradation to an open-ring peptide compound, L-747969. At later time points (>/=5 days postdose), there is a low level (</=7 picomoles/mg protein, or </=1.3% of administered dose) of covalent binding of radiolabel in plasma following single-dose administration of [ 3 H] caspofungin acetate, which may be due to two reactive intermediates formed during the chemical degradation of caspofungin to L-747969. Additional metabolism involves hydrolysis into constitutive amino acids and their degradates, including dihydroxyhomotyrosine and N-acetyl-dihydroxyhomotyrosine. These two tyrosine derivatives are found only in urine, suggesting rapid clearance of these derivatives by the kidneys.
Excretion
Two single-dose radiolabeled pharmacokinetic studies were conducted. In one study, plasma, urine, and feces were collected over 27 days, and in the second study plasma was collected over 6 months. Plasma concentrations of radioactivity and of caspofungin were similar during the first 24 to 48 hours postdose; thereafter drug levels fell more rapidly. In plasma, caspofungin concentrations fell below the limit of quantitation after 6 to 8 days postdose, while radiolabel fell below the limit of quantitation at 22.3 weeks postdose. After single intravenous administration of [ 3 H] caspofungin acetate, excretion of caspofungin and its metabolites in humans was 35% of dose in feces and 41% of dose in urine. A small amount of caspofungin is excreted unchanged in urine (~1.4% of dose). Renal clearance of parent drug is low (~0.15 mL/min) and total clearance of caspofungin is 12 mL/min.
Special Populations
Gender
Plasma concentrations of caspofungin in healthy men and women were similar following a single 70-mg dose. After 13 daily 50-mg doses, caspofungin plasma concentrations in women were elevated slightly (approximately 22% in area under the curve [AUC]) relative to men. No dosage adjustment is necessary based on gender.
Geriatric
Plasma concentrations of caspofungin in healthy older men and women (>/=65 years of age) were increased slightly (approximately 28% AUC) compared to young healthy men after a single 70-mg dose of caspofungin. In patients who were treated empirically or who had candidemia or other Candida infections (intra-abdominal abscesses, peritonitis, or pleural space infections), a similar modest effect of age was seen in older patients relative to younger patients. No dosage adjustment is necessary for the elderly (see PRECAUTIONS , Geriatric Use ).
Race
Regression analyses of patient pharmacokinetic data indicated that no clinically significant differences in the pharmacokinetics of caspofungin were seen among Caucasians, Blacks, and Hispanics. No dosage adjustment is necessary on the basis of race.
Renal Insufficiency
In a clinical study of single 70-mg doses, caspofungin pharmacokinetics were similar in volunteers with mild renal insufficiency (creatinine clearance 50 to 80 mL/min) and control subjects. Moderate (creatinine clearance 31 to 49 mL/min), advanced (creatinine clearance 5 to 30 mL/min), and end-stage (creatinine clearance <10 mL/min and dialy-sis dependent) renal insufficiency moderately increased caspofungin plasma concentrations after single-dose administration (range: 30 to 49% for AUC). However, in patients with invasive aspergillosis, candidemia, or other Candida infections (intra-abdominal abscesses, peritonitis, or pleural space infections) who received multiple daily doses of CANCIDAS 50 mg, there was no significant effect of mild to end-stage renal impairment on caspofungin concentrations. No dosage adjustment is necessary for patients with renal insufficiency. Caspofungin is not dialyzable, thus supplementary dosing is not required following hemodialysis.
Hepatic Insufficiency
Plasma concentrations of caspofungin after a single 70-mg dose in patients with mild hepatic insufficiency (Child-Pugh score 5 to 6) were increased by approximately 55% in AUC compared to healthy control subjects. In a 14-day multiple-dose study (70 mg on Day 1 followed by 50 mg daily thereafter), plasma concentrations in patients with mild hepatic insufficiency were increased modestly (19 to 25% in AUC) on Days 7 and 14 relative to healthy control subjects. No dosage adjustment is recommended for patients with mild hepatic insufficiency. Patients with moderate hepatic insufficiency (Child-Pugh score 7 to 9) who received a single 70-mg dose of CANCIDAS had an average plasma caspofungin increase of 76% in AUC compared to control subjects. A dosage reduction is recommended for patients with moderate hepatic insufficiency (see DOSAGE AND ADMINISTRATION ). There is no clinical experience in patients with severe hepatic insufficiency (Child-Pugh score >9).
Pediatric Patients
CANCIDAS has not been adequately studied in patients under 18 years of age.
MICROBIOLOGY
Mechanism of Action
Caspofungin acetate, the active ingredient of CANCIDAS, inhibits the synthesis of (beta) (1,3)-D-glucan, an essential component of the cell wall of susceptible Aspergillus species and Candida species. (beta) (1,3)-D-glucan is not present in mammalian cells. Caspofungin has shown activity against Candida species and in regions of active cell growth of the hyphae of Aspergillus fumigatus .
Activity in vitro
Caspofungin exhibits in vitro activity against Aspergillus species ( Aspergillus fumigatus, Aspergillus flavus , and Aspergillus terreus ) and Candida species ( Candida albicans, Candida glabrata, Candida guilliermondii, Candida krusei, Candida parapsilosis , and Candida tropicalis ). Susceptibility testing was performed according to the National Committee for Clinical Laboratory Standards (NCCLS) method M38-A (for Aspergillus species) and M27-A (for Candida species). Standardized susceptibility testing methods for echinocandins have not been established for yeasts and filamentous fungi, and results of susceptibility studies do not correlate with clinical outcome.
Activity in vivo
Caspofungin was active when parenterally administered to immunocompetent and immunosuppressed mice as long as 24 hours after disseminated infections with C. albicans, in which the endpoints were prolonged survival of infected mice and reduction of C. albicans from target organs. Caspofungin, administered parenterally to immunocompetent and immunosuppressed rodents, as long as 24 hours after disseminated or pulmonary infection with Aspergillus fumigatus , has shown prolonged survival, which has not been consistently associated with a reduction in mycological burden.
Drug Resistance
Mutants of Candida with reduced susceptibility to caspofungin have been identified in some patients during treatment. Similar observations were made in a study in mice infected with C. albicans and treated with orally administered doses of caspofungin. MIC values for caspofungin should not be used to predict clinical outcome, since a correlation between MIC values and clinical outcome has not been established. The incidence of drug resistance by various clinical isolates of Candida and Aspergillus species is unknown.
Drug Interactions
Studies in vitro and in vivo of caspofungin, in combination with amphotericin B, suggest no antagonism of antifungal activity against either A. fumigatus or C. albicans . The clinical significance of these results is unknown.
CLINICAL STUDIES
Empirical Therapy in febrile, neutropenic patients
A double-blind study enrolled 1111 febrile, neutropenic (<500 cells/mm 3 ) patients who were randomized to treatment with daily doses of CANCIDAS (50 mg/day following a 70-mg loading dose on Day 1) or AmBisome® 1 (amphotericin B liposome for injection, 3.0 mg/kg/day). Patients were stratified based on risk category (high-risk patients had undergone allogeneic stem cell transplantation or had relapsed acute leukemia) and on receipt of prior antifungal prophylaxis. Twenty-four percent of patients were high risk and 56% had received prior antifungal prophylaxis. Patients who remained febrile or clinically deteriorated following 5 days of therapy could receive 70 mg/day of CANCIDAS or 5.0 mg/kg/day of AmBisome. Treatment was continued to resolution of neutropenia (but not beyond 28 days unless a fungal infection was documented).
1 Registered trademark of Gilead Sciences, Inc.
An overall favorable response required meeting each of the following criteria: no documented breakthrough fungal infections up to 7 days after completion of treatment, survival for 7 days after completion of study therapy, no discontinuation of the study drug because of drug-related toxicity or lack of efficacy, resolution of fever during the period of neutropenia, and successful treatment of any documented baseline fungal infection.
Based on the composite response rates, CANCIDAS was as effective as AmBisome in empirical therapy of persistent febrile neutropenia (see Table 1).
[See table below]TABLE 1
Favorable Response of Patients with Persistent Fever and NeutropeniaCANCIDAS * AmBisome * % Difference
(Confidence Interval) **Number of Patients (Modified Intention-To-Treat)556 539 Overall Favorable Response190 (33.9%) 181 (33.7%) 0.2 (-5.6, 6.0) No documented breakthrough fungal
infection527 (94.8%) 515 (95.5%) -0.8 Survival 7 days after end of treatment515 (92.6%) 481 (89.2%) 3.4 No discontinuation due to toxicity or lack of efficacy499 (89.7%) 461 (85.5%) 4.2 Resolution of fever during neutropenia229 (41.2%) 223 (41.4%) -0.2 *CANCIDAS: 70 mg on Day 1, then 50 mg daily for the remainder of treatment (daily dose increased to 70 mg for 73 patients); AmBisome: 3.0 mg/kg/day (daily dose increased to 5.0 mg/kg for 74 patients).**Overall Response: estimated % difference adjusted for strata and expressed as CANCIDAS - AmBisome (95.2% CI); Individual criteria presented above are not mutually exclusive. The percent difference calculated as CANCIDAS - AmBisome.
The rate of successful treatment of documented baseline infections, a component of the primary endpoint, was not statistically different between treatment groups.
The response rates did not differ between treatment groups based on either of the stratification variables: risk category or prior antifungal prophylaxis.
Candidemia and the following other Candida infections: intra-abdominal abscesses, peritonitis and pleural space infections
In a Phase III randomized, double-blind study, patients with a proven diagnosis of invasive candidiasis received daily doses of CANCIDAS (50 mg/day following a 70-mg loading dose on Day 1) or amphotericin B deoxycholate (0.6 to 0.7 mg/kg/day for non-neutropenic patients and 0.7 to 1.0 mg/kg/day for neutropenic patients). Patients were stratified by both neutropenic status and APACHE II score. Patients with Candida endocarditis, meningitis, or osteomyelitis were excluded from this study.
Patients who met the entry criteria and received one or more doses of IV study therapy were included in the primary (modified intention-to-treat [MITT]) analysis of response at the end of IV study therapy. A favorable response at this time point required both symptom/sign resolution/improvement and microbiological clearance of the Candida infection.
Two hundred thirty-nine patients were enrolled. Patient disposition is shown in Table 2.
[See table below]TABLE 2
Disposition in Candidemia and Other Candida Infections
(Intra-abdominal abscesses, peritonitis, and pleural space infections)CANCIDAS * Amphotericin B Randomized patients114 125 Patients completing study **63 (55.3%) 69 (55.2%) DISCONTINUATIONS OF STUDY **All Study Discontinuations51 (44.7%) 56 (44.8%) Study Discontinuations due to clinical adverse events39 (34.2%) 43 (34.4%) Study Discontinuations due to laboratory adverse events0 (0%) 1 (0.8%) DISCONTINUATIONS OF STUDY THERAPYAll Study Therapy Discontinuations48 (42.1%) 58 (46.4%) Study Therapy Discontinuations due to clinical adverse events30 (26.3%) 37 (29.6%) Study Therapy Discontinuations due to laboratory adverse events1 (0.9%) 7 (5.6%) Study Therapy Discontinuations due to all drug-related *** adverse events3 (2.6%) 29 (23.2%) *Patients received CANCIDAS 70 mg on Day 1, then 50 mg daily for the remainder of their treatment.**Study defined as study treatment period and 6-8 week follow-up period.***Determined by the investigator to be possibly, probably, or definitely drug-related.Of the 239 patients enrolled, 224 met the criteria for inclusion in the MITT population (109 treated with CANCIDAS and 115 treated with amphotericin B). Of these 224 patients, 186 patients had candidemia (92 treated with CANCIDAS and 94 treated with amphotericin B). The majority of the patients with candidemia were non-neutropenic (87%) and had an APACHE II score less than or equal to 20 (77%) in both arms. Most candidemia infections were caused by C. albicans (39%), followed by C. parapsilosis (20%), C. tropicalis (17%), C. glabrata (8%), and C. krusei (3%).
At the end of IV study therapy, CANCIDAS was comparable to amphotericin B in the treatment of candidemia in the MITT population. For the other efficacy time points (Day 10 of IV study therapy, end of all antifungal therapy, 2-week post-therapy follow-up, and 6- to 8-week post-therapy follow-up), CANCIDAS was as effective as amphotericin B.
Outcome, relapse and mortality data are shown in Table 3.
[See table below]TABLE 3
Outcomes, Relapse, & Mortality in Candidemia and Other Candida Infections
(Intra-abdominal abscesses, peritonitis, and pleural space infections)Number of
MITT **/* patientsCANCIDAS * Amphotericin B % Difference ** after adjusting for strata (Confidence Interval) *** 109 115 FAVORABLE OUTCOMES (MITT) AT THE END OF IV STUDY THERAPYAll MITT patients81/109 (74.3%) 78/115 (67.8%) 7.5 (-5.4, 20.3) Candidemia67/92 (72.8%) 63/94 (67.0%) 7.0 (-7.0, 21.1) Neutropenic6/14 (43%) 5/10 (50%) Non-neutropenic61/78 (78%) 58/84 (69%) Endophthalmitis0/1 2/3 Multiple Sites4/5 4/4 Blood / Pleural1/1 1/1 Blood / Peritoneal1/1 1/1 Blood / Urine- 1/1 Peritoneal / Pleural1/2 - Abdominal / Peritoneal- 1/1 Subphrenic / Peritoneal1/1 - DISSEMINATED INFECTIONS, RELAPSES AND MORTALITYDisseminated Infections in neutropenic patients4/14 (28.6%) 3/10 (30.0%) All relapses &7/81 (8.6%) 8/78 (10.3%) Culture-confirmed relapse5/81 (6%) 2/78 (3%) Overall study # mortality in MITT36/109 (33.0%) 35/115 (30.4%) Mortality during study therapy18/109 (17%) 13/115 (11%) Mortality attributed to Candida4/109 (4%) 7/115 (6%) *Patients received CANCIDAS 70 mg on Day 1, then 50 mg daily for the remainder of their treatment.**Calculated as CANCIDAS - amphotericin B***95% CI for candidemia, 95.6% for all patients**/* Modified intention-to-treat& Includes all patients who either developed a culture-confirmed recurrence of Candida infection or required antifungal therapy for the treatment of a proven or suspected Candida infection in the follow-up period.# Study defined as study treatment period and 6-8 week follow-up period.In this study, the efficacy of CANCIDAS in patients with intra-abdominal abscesses, peritonitis and pleural space Candida infections was evaluated in 19 non-neutropenic patients. Two of these patients had concurrent candidemia. Candida was part of a polymicrobial infection that required adjunctive surgical drainage in 11 of these 19 patients. A favorable response was seen in 9 of 9 patients with peritonitis, 3 of 4 with abscesses (liver, parasplenic, and urinary bladder abscesses), 2 of 2 with pleural space infections, 1 of 2 with mixed peritoneal and pleural infection, 1 of 1 with mixed abdominal abscess and peritonitis, and 0 of 1 with Candida pneumonia.
Overall, across all sites of infection included in the study, the efficacy of CANCIDAS was comparable to that of amphotericin B for the primary endpoint.
In this study, the efficacy data for CANCIDAS in neutropenic patients with candidemia were limited. In a separate compassionate use study, 4 patients with hepatosplenic candidiasis received prolonged therapy with CANCIDAS following other long-term antifungal therapy; three of these patients had a favorable response.
Esophageal Candidiasis (and information on oropharyngeal candidiasis)
The safety and efficacy of CANCIDAS in the treatment of esophageal candidiasis was evaluated in one large, controlled, noninferiority, clinical trial and two smaller dose-response studies.
In all 3 studies, patients were required to have symptoms and microbiological documentation of esophageal candidiasis; most patients had advanced AIDS (with CD4 counts <50/mm 3 ).
Of the 166 patients in the large study who had culture-confirmed esophageal candidiasis at baseline, 120 had Candida albicans and 2 had Candida tropicalis as the sole baseline pathogen whereas 44 had mixed baseline cultures containing C. albicans and one or more additional Candida species.
In the large, randomized, double-blind study comparing CANCIDAS 50 mg/day versus intravenous fluconazole 200 mg/day for the treatment of esophageal candidiasis, patients were treated for an average of 9 days (range 7-21 days). The primary endpoint was favorable overall response at 5 to 7 days following discontinuation of study therapy, which required both complete resolution of symptoms and significant endoscopic improvement. The definition of endoscopic response was based on severity of disease at baseline using a 4-grade scale and required at least a two-grade reduction from baseline endoscopic score or reduction to grade 0 for patients with a baseline score of 2 or less.
The proportion of patients with a favorable overall response for the primary endpoint was comparable for CANCIDAS and fluconazole as shown in Table 4.
[See table below]TABLE 4
Favorable Response Rates for
Patients with Esophageal CandidiasisCANCIDAS Fluconazole % Difference *
(95% CI)Day 5-7 post-treatment 66/81 (81.5%) 80/94 (85.1%) -3.6 (-14.7, 7.5) *calculated as CANCIDAS - fluconazole
The proportion of patients with a favorable symptom response was also comparable (90.1% and 89.4% for CANCIDAS and fluconazole, respectively). In addition, the proportion of patients with a favorable endoscopic response was comparable (85.2% and 86.2% for CANCIDAS and fluconazole, respectively).
As shown in Table 5, the esophageal candidiasis relapse rates at the Day 14 post-treatment visit were similar for the two groups. At the Day 28 post-treatment visit, the group treated with CANCIDAS had a numerically higher incidence of relapse, however, the difference was not statistically significant.
[See table below]TABLE 5
Relapse Rates at 14 and 28 Days Post-Therapy in Patients
with Esophageal Candidiasis at BaselineCANCIDAS Fluconazole % Difference *
(95% CI)Day 14 post-treatment 7/66 (10.6%) 6/76 (7.9%) 2.7 (-6.9, 12.3) Day 28 post-treatment 18/64 (28.1%) 12/72 (16.7%) 11.5 (-2.5, 25.4) *calculated as CANCIDAS - fluconazole In this trial, which was designed to establish noninferiority of CANCIDAS to fluconazole for the treatment of esophageal candidiasis, 122 (70%) patients also had oropharyngeal candidiasis. A favorable response was defined as complete resolution of all symptoms of oropharyngeal disease and all visible oropharyngeal lesions. The proportion of patients with a favorable oropharyngeal response at the 5- to 7-day post-treatment visit was numerically lower for CANCIDAS, however, the difference was not statistically significant. The results are shown in Table 6.
[See table below]TABLE 6
Oropharyngeal Candidiasis Response Rates at 5 to 7 Days
Post-Therapy in Patients with Oropharyngeal
and Esophageal Candidiasis at BaselineCANCIDAS Fluconazole % Difference *
(95% CI)Day 5-7 post-treatment 40/56 (71.4%) 55/66 (83.3%) -11.9 (-26.8, 3.0) *calculated as CANCIDAS - fluconazole
As shown in Table 7, the oropharyngeal candidiasis relapse rates at the Day 14 and the Day 28 post-treatment visits were statistically significantly higher for CANCIDAS than for fluconazole.
[See table below]TABLE 7
Oropharyngeal Candidiasis Relapse Rates at 14 and 28 Days Post-Therapy in Patients with Oropharyngeal
and Esophageal Candidiasis at BaselineCANCIDAS Fluconazole % Difference *
(95% CI)Day 14 post-treatment 17/40 (42.5%) 7/53 (13.2%) 29.3 (11.5, 47.1) Day 28 post-treatment 23/39 (59.0%) 18/51 (35.3%) 23.7 (3.4, 43.9) *calculated as CANCIDAS - fluconazole
The results from the two smaller dose-ranging studies corroborate the efficacy of CANCIDAS for esophageal candidiasis that was demonstrated in the larger study.
CANCIDAS was associated with favorable outcomes in 7 of 10 esophageal C. albicans infections refractory to at least 200 mg of fluconazole given for 7 days, although the in vitro susceptibility of the infecting isolates to fluconazole was not known.
Invasive Aspergillosis
Sixty-nine patients between the ages of 18 and 80 with invasive aspergillosis (IA) were enrolled in an open-label, noncomparative study to evaluate the safety, tolerability, and efficacy of CANCIDAS. Enrolled patients had previously been refractory to or intolerant of other antifungal therapy(ies). Refractory patients were classified as those who had disease progression or failed to improve despite therapy for at least 7 days with amphotericin B, lipid formulations of amphotericin B, itraconazole, or an investigational azole with reported activity against Aspergillus . Intolerance to previous therapy was defined as a doubling of creatinine (or creatinine >/=2.5 mg/dL while on therapy), other acute reactions, or infusion-related toxicity. To be included in the study, patients with pulmonary disease must have had definite (positive tissue histopathology or positive culture from tissue obtained by an invasive procedure) or probable (positive radiographic or computed tomography evidence with supporting culture from bronchoalveolar lavage or sputum, galactomannan enzyme-linked immunosorbent assay, and/or polymerase chain reaction) invasive aspergillosis. Patients with extrapulmonary disease had to have definite invasive aspergillosis. The definitions were modeled after the Mycoses Study Group Criteria. 2 Patients were administered a single 70-mg loading dose of CANCIDAS and subsequently dosed with 50 mg daily. The mean duration of therapy was 33.7 days, with a range of 1 to 162 days.
2 Denning DW, Lee JY, Hostetler JS, et al. NIAID Mycoses Study Group multicenter trial of oral itraconazole therapy for invasive aspergillosis. Am J Med 1994; 97:135-144.
An independent expert panel evaluated patient data, including diagnosis of invasive aspergillosis, response and tolerability to previous antifungal therapy, treatment course on CANCIDAS, and clinical outcome.
A favorable response was defined as either complete resolution (complete response) or clinically meaningful improvement (partial response) of all signs and symptoms and attributable radiographic findings. Stable, nonprogressive disease was considered to be an unfavorable response.
Among the 69 patients enrolled in the study, 63 met entry diagnostic criteria and had outcome data; and of these, 52 patients received treatment for >7 days. Fifty-three (84%) were refractory to previous antifungal therapy and 10 (16%) were intolerant. Forty-five patients had pulmonary disease and 18 had extrapulmonary disease. Underlying conditions were hematologic malignancy (N=24), allogeneic bone marrow transplant or stem cell transplant (N=18), organ transplant (N=8), solid tumor (N=3), or other conditions (N=10). All patients in the study received concomitant therapies for their other underlying conditions. Eighteen patients received tacrolimus and CANCIDAS concomitantly, of whom 8 also received mycophenolate mofetil.
Overall, the expert panel determined that 41% (26/63) of patients receiving at least one dose of CANCIDAS had a favorable response. For those patients who received >7 days of therapy with CANCIDAS, 50% (26/52) had a favorable response. The favorable response rates for patients who were either refractory to or intolerant of previous therapies were 36% (19/53) and 70% (7/10), respectively. The response rates among patients with pulmonary disease and extrapulmonary disease were 47% (21/45) and 28% (5/18), respectively. Among patients with extrapulmonary disease, 2 of 8 patients who also had definite, probable, or possible CNS involvement had a favorable response. Two of these 8 patients had progression of disease and manifested CNS involvement while on therapy.
There is substantial evidence that CANCIDAS is well tolerated and effective for the treatment of invasive aspergillosis in patients who are refractory to or intolerant of itraconazole, amphotericin B, and/or lipid formulations of amphotericin B. However, the efficacy of CANCIDAS has not been evaluated in concurrently controlled clinical studies, with other antifungal therapies.
INDICATIONS AND USAGE
CANCIDAS is indicated for:
- Empirical therapy for presumed fungal infections in febrile, neutropenic patients.
- Treatment of Candidemia and the following Candida infections: intra-abdominal abscesses, peritonitis and pleural space infections. CANCIDAS has not been studied in endocarditis, osteomyelitis, and meningitis due to Candida.
- Treatment of Esophageal Candidiasis (see CLINICAL STUDIES ).
- Treatment of Invasive Aspergillosis in patients who are refractory to or intolerant of other therapies (i.e., amphotericin B, lipid formulations of amphotericin B, and/or itraconazole). CANCIDAS has not been studied as initial therapy for invasive aspergillosis.
CONTRAINDICATIONS
CANCIDAS is contraindicated in patients with hypersensitivity to any component of this product.
WARNINGS
Concomitant use of CANCIDAS with cyclosporine should be limited to patients for whom the potential benefit outweighs the potential risk. In one clinical study, 3 of 4 healthy subjects who received CANCIDAS 70 mg on Days 1 through 10, and also received two 3 mg/kg doses of cyclosporine 12 hours apart on Day 10, developed transient elevations of alanine transaminase (ALT) on Day 11 that were 2 to 3 times the upper limit of normal (ULN). In a separate panel of subjects in the same study, 2 of 8 who received CANCIDAS 35 mg daily for 3 days and cyclosporine (two 3 mg/kg doses administered 12 hours apart) on Day 1 had small increases in ALT (slightly above the ULN) on Day 2. In both groups, elevations in aspartate transaminase (AST) paralleled ALT elevations, but were of lesser magnitude (see ADVERSE REACTIONS ).
In a retrospective study, 40 immunocompromised patients, including 37 transplant recipients, were treated during marketed use with CANCIDAS and cyclosporine for 1 to 290 days (median 17.5 days). Fourteen patients (35%) developed transaminase elevations >5 × upper limit of normal or >3 × baseline during concomitant therapy or the 14-day follow-up period; five were considered possibly related to concomitant therapy. One patient had elevated bilirubin considered possibly related to concomitant therapy. No patient developed clinical evidence of hepatotoxicity or serius hepatic events. Discontinuation due to laboratory abnormalities in hepatic enzymes from any cause occurred in four patients. Of these, 2 were considered possibly related to therapy with CANCIDAS and/or cyclosporine as well as to other possible causes.
In the prospective invasive aspergillosis and compassionate use studies, there were 4 patients treated with CANCIDAS (50 mg/day) and cyclosporine for 2 to 56 days. None of these patients experienced increases in hepatic enzymes.
Given the limitations of these data, CANCIDAS and cyclosporine should only be used concomitantly in those patients for whom the potential benefit outweighs the potential risk. Patients who develop abnormal liver function tests during concomitant therapy should be monitored and the risk/benefit of continuing therapy should be evaluated.
PRECAUTIONS
General
The efficacy of a 70-mg dose regimen in patients with invasive aspergillosis who are not clinically responding to the 50-mg daily dose is not known. Limited safety data suggest that an increase in dose to 70 mg daily is well tolerated. The safety and efficacy of doses above 70 mg have not been adequately studied in patients with Candida infections. However, CANCIDAS was generally well tolerated at a dose of 100 mg once daily for 21 days when administered to 15 healthy subjects.
The safety information on treatment durations longer than 4 weeks is limited; however, available data suggest that CANCIDAS continues to be well tolerated with longer courses of therapy (up to 162 days).
Hepatic Effects
Laboratory abnormalities in liver function tests have been seen in healthy volunteers and patients treated with CANCIDAS. In some patients with serious underlying conditions who were receiving multiple concomitant medications along with CANCIDAS, clinical hepatic abnormalities have also occurred. Isolated cases of significant hepatic dysfunction, hepatitis, or worsening hepatic failure have been reported in patients; a causal relationship to CANCIDAS has not been established. Patients who develop abnormal liver function tests during CANCIDAS therapy should be monitored for evidence of worsening hepatic function and evaluated for risk/benefit of continuing CANCIDAS therapy.
Drug Interactions
Studies in vitro show that caspofungin acetate is not an inhibitor of any enzyme in the cytochrome P450 (CYP) system. In clinical studies, caspofungin did not induce the CYP3A4 metabolism of other drugs. Caspofungin is not a substrate for P-glycoprotein and is a poor substrate for cytochrome P450 enzymes.
Clinical studies in healthy volunteers show that the pharmacokinetics of CANCIDAS are not altered by itraconazole, amphotericin B, mycophenolate, nelfinavir, or tacrolimus. CANCIDAS has no effect on the pharmacokinetics of itraconazole, amphotericin B, or the active metabolite of mycophenolate.
CANCIDAS reduced the blood AUC 0-12 of tacrolimus (FK-506, Prograf ® 3 ) by approximately 20%, peak blood concentration (C max ) by 16%, and 12-hour blood concentration (C 12hr ) by 26% in healthy subjects when tacrolimus (2 doses of 0.1 mg/kg 12 hours apart) was administered on the 10th day of CANCIDAS 70 mg daily, as compared to results from a control period in which tacrolimus was administered alone. For patients receiving both therapies, standard monitoring of tacrolimus blood concentrations and appropriate tacrolimus dosage adjustments are recommended.
3 Registered trademark of Fujisawa Healthcare, Inc.
In two clinical studies, cyclosporine (one 4 mg/kg dose or two 3 mg/kg doses) increased the AUC of caspofungin by approximately 35%. CANCIDAS did not increase the plasma levels of cyclosporine. There were transient increases in liver ALT and AST when CANCIDAS and cyclosporine were co-administered (see WARNINGS and ADVERSE REACTIONS ).
A drug-drug interaction study with rifampin in healthy volunteers has shown a 30% decrease in caspofungin trough concentrations. Patients on rifampin should receive 70 mg of CANCIDAS daily. In addition, results from regression analyses of patient pharmacokinetic data suggest that co-administration of other inducers of drug clearance (efavirenz, nevirapine, phenytoin, dexamethasone, or carbamazepine) with CANCIDAS may result in clinically meaningful reductions in caspofungin concentrations. It is not known which drug clearance mechanism involved in caspofungin disposition may be inducible. When CANCIDAS is co-administered with inducers of drug clearance, such as efavirenz, nevirapine, phenytoin, dexamethasone, or carbamazepine, use of a daily dose of 70 mg of CANCIDAS should be considered.
Carcinogenesis, Mutagenesis, Impairment of Fertility
No long-term studies in animals have been performed to evaluate the carcinogenic potential of caspofungin.
Caspofungin did not show evidence of mutagenic or genotoxic potential when evaluated in the following in vitro assays: bacterial (Ames) and mammalian cell (V79 Chinese hamster lung fibroblasts) mutagenesis assays, the alkaline elution/rat hepatocyte DNA strand break test, and the chromosome aberration assay in Chinese hamster ovary cells. Caspofungin was not genotoxic when assessed in the mouse bone marrow chromosomal test at doses up to 12.5 mg/kg (equivalent to a human dose of 1 mg/kg based on body surface area comparisons), administered intravenously.
Fertility and reproductive performance were not affected by the intravenous administration of caspofungin to rats at doses up to 5 mg/kg. At 5 mg/kg exposures were similar to those seen in patients treated with the 70-mg dose.
Pregnancy
Pregnancy Category C. CANCIDAS was shown to be embryotoxic in rats and rabbits. Findings included incomplete ossification of the skull and torso and an increased incidence of cervical rib in rats. An increased incidence of incomplete ossifications of the talus/calcaneus was seen in rabbits. Caspofungin also produced increases in resorptions in rats and rabbits and periimplantation losses in rats. These findings were observed at doses which produced exposures similar to those seen in patients treated with a 70-mg dose. Caspofungin crossed the placental barrier in rats and rabbits and was detected in the plasma of fetuses of pregnant animals dosed with CANCIDAS. There are no adequate and well-controlled studies in pregnant women. CANCIDAS should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Nursing Mothers
Caspofungin was found in the milk of lactating, drug-treated rats. It is not known whether caspofungin is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when caspofungin is administered to a nursing woman.
Patients with Hepatic Insufficiency
Patients with mild hepatic insufficiency (Child-Pugh score 5 to 6) do not need a dosage adjustment. For patients with moderate hepatic insufficiency (Child-Pugh score 7 to 9), CANCIDAS 35 mg daily is recommended. However, where recommended, a 70-mg loading dose should still be administered on Day 1 (see DOSAGE AND ADMINISTRATION ). There is no clinical experience in patients with severe hepatic insufficiency (Child-Pugh score >9).
Pediatric Use
Safety and effectiveness in pediatric patients have not been established.
Geriatric Use
Clinical studies of CANCIDAS did not include sufficient numbers of patients aged 65 and over to determine whether they respond differently from younger patients. Although the number of elderly patients was not large enough for a statistical analysis, no overall differences in safety or efficacy were observed between these and younger patients. Plasma concentrations of caspofungin in healthy older men and women (>/=65 years of age) were increased slightly (approximately 28% in AUC) compared to young healthy men.
A similar effect of age on pharmacokinetics was seen in patients with candidemia or other Candida infections (intra-abdominal abscesses, peritonitis, or pleural space infections). No dose adjustment is recommended for the elderly; however, greater sensitivity of some older individuals cannot be ruled out.
ADVERSE REACTIONS
General
Possible histamine-mediated symptoms have been reported including reports of rash, facial swelling, pruritus, sensation of warmth, or bronchospasm. Anaphylaxis has been reported during administration of CANCIDAS.
Clinical Adverse Experiences
The overall safety of caspofungin was assessed in 1440 individuals who received single or multiple doses of caspofungin acetate: 564 febrile, neutropenic patients (empirical therapy study); 125 patients with candidemia and/or intra-abdominal abscesses, peritonitis, or pleural space infections (including 4 patients with chronic disseminated candidiasis); 285 patients with esophageal and/or oropharyngeal candidiasis; 72 patients with invasive aspergillosis; and 394 individuals in phase I studies. In the empirical therapy study patients had undergone hematopoietic stem-cell transplantation or chemotherapy. In the studies involving patients with documented Candida infections, the majority of the patients had serious underlying medical conditions (e.g., hematologic or other malignancy, recent major surgery, HIV) requiring multiple concomitant medications. Patients in the noncomparative Aspergillus study often had serious predisposing medical conditions (e.g., bone marrow or peripheral stem cell transplants, hematologic malignancy, solid tumors or organ transplants) requiring multiple concomitant medications.
Empirical Therapy
In the randomized, double-blinded empirical therapy study, patients received either CANCIDAS 50 mg/day (following a 70-mg loading dose) or AmBisome (3.0 mg/kg/day). In this study clinical or laboratory hepatic adverse events were reported in 39% and 45% of patients in the CANCIDAS and AmBisome groups, respectively, regardless of causality. Also reported was an isolated, serious adverse experience of hyperbilirubinemia considered possibly related to CANCIDAS. Drug-related clinical adverse experiences occurring in >/=2% of the patients in either treatment group are presented in Table 8.
TABLE 8
Drug-Related * Clinical Adverse Experiences Among
Patients with Persistent Fever and Neutropenia
Incidence >/=2% for at least one treatment group by
Body SystemCANCIDAS **
N=564 (percent)AmBisome ***
N=547 (percent)Body as a WholeAbdominal Pain1.4 2.4 Chills13.8 24.7 Fever17.0 19.4 Flushing1.8 4.2 Perspiration/Diaphoresis2.8 2.2 Cardiovascular SystemHypertension1.1 2.0 Tachycardia1.4 2.4 Digestive SystemDiarrhea2.7 2.4 Nausea3.5 11.3 Vomiting3.5 8.6 Metabolism and NutritionHypokalemia3.7 4.2 Musculoskeletal SystemBack Pain0.7 2.7 Nervous System &
PsychiatricHeadache4.3 5.7 Respiratory SystemDyspnea2.0 4.2 Tachypnea0.4 2.0 Skin & Skin AppendageRash6.2 5.3 * Determined by the investigator to be possibly, probably, or definitely drug-related.** 70 mg on Day 1, then 50 mg daily for the remainder of treatment; daily dose was increased to 70 mg for 73 patients.*** 3.0 mg/kg/day; daily dose was increased to 5.0 mg/kg for 74 patients.The proportion of patients who experienced an infusion-related adverse event was significantly lower in the group treated with CANCIDAS (35.1%) than in the group treated with AmBisome (51.6%).
Drug-related laboratory adverse experiences occurring in >/=2% of the patients in either treatment group are presented in Table 9.
[See table below]TABLE 9
Drug-Related * Laboratory Adverse Experiences Among Patients
with Persistent Fever and Neutropenia
Incidence >/=2% for at least one treatment group by Laboratory Test CategoryCANCIDAS **
N=564 (percent)AmBisome ***
N=547 (percent)Blood ChemistryAlanine aminotransferase increased8.7 8.9 Alkaline phosphatase increased7.0 12.0 Aspartate aminotransferase increased7.0 7.6 Direct serum bilirubin increased2.6 5.2 Total serum bilirubin increased3.0 5.2 Hypokalemia7.3 11.8 Hypomagnesemia2.3 2.6 Serum creatinine increased1.2 5.5 * Determined by the investigator to be possibly, probably, or definitely drug-related.** 70 mg on Day 1, then 50 mg daily for the remainder of treatment; daily dose was increased to 70 mg for 73 patients.*** 3.0 mg/kg/day; daily dose was increased to 5.0 mg/kg for 74 patients.
The percentage of patients with either a drug-related clinical or a drug-related laboratory adverse experience was significantly lower among patients receiving CANCIDAS (54.4%) than among patients receiving AmBisome (69.3%). Furthermore, the incidence of discontinuation due to a drug-related clinical or laboratory adverse experience was significantly lower among patients treated with CANCIDAS (5.0%) than among patients treated with AmBisome (8.0%).
To evaluate the effect of CANCIDAS and AmBisome on renal function, nephrotoxicity was defined as doubling of serum creatinine relative to baseline or an increase of >/=1 mg/dL in serum creatinine if baseline serum creatinine was above the upper limit of the normal range. Among patients whose baseline creatinine clearance was >30 mL/min, the incidence of nephrotoxicity was significantly lower in the group treated with CANCIDAS (2.6%) than in the group treated with AmBisome (11.5%). Serious clinical renal events, regardless of causality, were similar between CANCIDAS (11/564, 2.0%) and AmBisome (12/547, 2.2%).
Candidemia and other Candida infections (see CLINICAL STUDIES )
In the randomized, double-blinded invasive candidiasis study, patients received either CANCIDAS 50 mg/day (following a 70-mg loading dose) or amphotericin B 0.6 to 1.0 mg/kg/day. Drug-related clinical adverse experiences occurring in >/=2% of the patients in either treatment group are presented in Table 10.
TABLE 10
Drug-Related * Clinical Adverse Experiences Among
Patients with Candidemia or other Candida Infections **
Incidence >/=2% for at least one treatment group by Body SystemCANCIDAS 50 mg ***
N=114 (percent)Amphotericin B
N=125 (percent)Body as a WholeChills5.3 26.4 Fever7.0 23.2 Cardiovascular SystemHypertension1.8 6.4 Hypotension0.9 2.4 Tachycardia1.8 10.4 Peripheral Vascular
SystemPhlebitis/thrombophlebitis3.5 4.8 Digestive SystemDiarrhea2.6 0.8 Jaundice0.9 3.2 Nausea1.8 5.6 Vomiting3.5 8.0 Metabolic/Nutritional/
ImmuneHypokalemia0.9 5.6 Nervous System &
PsychiatricTremor1.8 2.4 Respiratory SystemTachypnea0.0 10.4 Skin & Skin AppendageErythema0.0 2.4 Rash0.9 3.2 Sweating0.9 3.2 Urogenital SystemRenal insufficiency0.9 5.6 Renal insufficiency, acute0.0 5.6 *Determined by the investigator to be possibly, probably, or definitely drug-related.**Intra-abdominal abscesses, peritonitis and pleural space infections***Patients received CANCIDAS 70 mg on Day 1, then 50 mg daily for the remainder of their treatment.
The incidence of drug-related clinical adverse experiences was significantly lower among patients treated with CANCIDAS (28.9%) than among patients treated with amphotericin B (58.4%). Also, the proportion of patients who experienced an infusion-related adverse event was significantly lower in the group treated with CANCIDAS (20.2%) than in the group treated with amphotericin B (48.8%).
Drug-related laboratory adverse experiences occurring in >/=2% of the patients in either treatment group are presented in Table 11.
TABLE 11
Drug-Related * Laboratory Adverse Experiences Among
Patients with Candidemia or other Candida Infections **
Incidence >/=2% for at least one treatment group by
Laboratory Test CategoryCANCIDAS 50 mg ***
N=114 (percent)Amphotericin B
N=125 (percent)Blood ChemistryALT increased3.7 8.1 AST increased1.9 9.0 Blood urea
increased1.9 15.8 Direct serum bilirubin
increased3.8 8.4 Serum alkaline
phosphatase increased8.3 15.6 Serum bicarbonate
decreased0.0 3.6 Serum creatinine
increased3.7 22.6 Serum phosphate
increased0.0 2.7 Serum potassium
decreased9.9 23.4 Serum potassium
increased0.9 2.4 Total serum bilirubin
increased2.8 8.9 HematologyHematocrit decreased0.9 7.3 Hemoglobin decreased0.9 10.5 UrinalysisUrine protein increased0.0 3.7 *Determined by the investigator to be possibly, probably, or definitely drug-related.**Intra-abdominal abscesses, peritonitis and pleural space infections***Patients received CANCIDAS 70 mg on Day 1, then 50 mg daily for the remainder of their treatment.
The incidence of drug-related laboratory adverse experiences was significantly lower among patients receiving CANCIDAS (24.3%) than among patients receiving amphotericin B (54.0%).
The percentage of patients with either a drug-related clinical adverse experience or a drug-related laboratory adverse experience was significantly lower among patients receiving CANCIDAS (42.1%) than among patients receiving amphotericin B (75.2%). Furthermore, a significant difference between the two treatment groups was observed with regard to incidence of discontinuation due to drug-related clinical or laboratory adverse experience; incidences were 3/114 (2.6%) in the group treated with CANCIDAS and 29/125 (23.2%) in the group treated with amphotericin B.
To evaluate the effect of CANCIDAS and amphotericin B on renal function, nephrotoxicity was defined as doubling of serum creatinine relative to baseline or an increase of >/=1 mg/dL in serum creatinine if baseline serum creatinine was above the upper limit of the normal range. In a subgroup of patients whose baseline creatinine clearance was >30 mL/min, the incidence of nephrotoxicity was significantly lower in the group treated with CANCIDAS than in the group treated with amphotericin B.
Esophageal Candidiasis and Oropharyngeal Candidiasis
Drug-related clinical adverse experiences occurring in >/=2% of patients with esophageal and/or oropharyngeal candidiasis are presented in Table 12.
TABLE 12
Drug-Related Clinical Adverse Experiences Among Patients with
Esophageal and/or Oropharyngeal Candidiasis *
Incidence >/=2% for at least one treatment dose (per comparison) by Body SystemCANCIDAS
50 mg **
N=83
(percent)Fluconazole IV
200 mg **
N=94
(percent)CANCIDAS
50 mg ***
N=80
(percent)CANCIDAS
70 mg ***
N=65
(percent)Amphotericin B
0.5 mg/kg ***
N=89
(percent)Body as a WholeAsthenia/fatigue0.0 0.0 0.0 0.0 6.7 Chills0.0 0.0 2.5 1.5 75.3 Edema/swelling0.0 0.0 0.0 0.0 5.6 Edema, facial0.0 0.0 0.0 3.1 0.0 Fever3.6 1.1 21.3 26.2 69.7 Flu-like illness0.0 0.0 0.0 3.1 0.0 Malaise0.0 0.0 0.0 0.0 5.6 Pain0.0 0.0 1.3 4.6 5.6 Pain, abdominal3.6 2.1 2.5 0.0 9.0 Warm sensation0.0 0.0 0.0 1.5 4.5 Peripheral Vascular SystemInfused vein complication12.0 8.5 2.5 1.5 0.0 Phlebitis/thrombophlebitis15.7 8.5 11.3 13.8 22.5 Cardiovascular SystemTachycardia0.0 0.0 1.3 0.0 4.5 Vasculitis0.0 0.0 0.0 0.0 3.4 Digestive SystemAnorexia0.0 0.0 1.3 0.0 3.4 Diarrhea3.6 2.1 1.3 3.1 11.2 Gastritis0.0 2.1 0.0 0.0 0.0 Nausea6.0 6.4 2.5 3.1 21.3 Vomiting1.2 3.2 1.3 3.1 13.5 Hemic & Lymphatic SystemAnemia0.0 0.0 3.8 0.0 9.0 Metabolic/Nutritional/ImmuneAnaphylaxis0.0 0.0 0.0 0.0 2.2 Musculoskeletal SystemMyalgia1.2 0.0 0.0 3.1 2.2 Pain, back0.0 0.0 0.0 0.0 2.2 Pain, musculoskeletal0.0 0.0 1.3 0.0 4.5 Nervous System & PsychiatricDizziness0.0 2.1 0.0 1.5 1.1 Headache6.0 1.1 11.3 7.7 19.1 Insomnia1.2 0.0 0.0 0.0 2.2 Paresthesia0.0 0.0 1.3 3.1 1.1 Tremor0.0 0.0 0.0 0.0 7.9 Respiratory SystemTachypnea0.0 0.0 1.3 0.0 4.5 Skin & Skin AppendageErythema1.2 0.0 1.3 1.5 7.9 Induration0.0 0.0 0.0 3.1 6.7 Pruritus1.2 0.0 2.5 1.5 0.0 Rash0.0 0.0 1.3 4.6 3.4 Sweating0.0 0.0 1.3 0.0 3.4 *Relationship to drug was determined by the investigator to be possibly, probably or definitely drug-related.**Derived from a Phase III comparator-controlled clinical study.***Derived from Phase II comparator-controlled clinical studies.Laboratory abnormalities occurring in >/=2% of patients with esophageal and/or oropharyngeal candidiasis are presented in Table 13.
TABLE 13
Drug-Related Laboratory Abnormalities Reported Among Patients with
Esophageal and/or Oropharyngeal Candidiasis *
Incidence >/=2% (for at least one treatment dose) by Laboratory Test CategoryCANCIDAS
50 mg **
N=163
(percent)CANCIDAS
70 mg ***
N=65
(percent)Fluconazole IV
200 mg **
N=94
(percent)Amphotericin B
0.5 mg/kg ***
N=89
(percent)Blood ChemistryALT increased10.6 10.8 11.8 22.7 AST increased13.0 10.8 12.9 22.7 Blood urea increased0.0 0.0 1.2 10.3 Direct serum bilirubin increased0.6 0.0 3.3 2.5 Serum albumin decreased8.6 4.6 5.4 14.9 Serum alkaline phosphatase increased10.5 7.7 11.8 19.3 Serum bicarbonate decreased0.9 0.0 0.0 6.6 Serum calcium decreased1.9 0.0 3.2 1.1 Serum creatinine increased0.0 1.5 2.2 28.1 Serum potassium decreased3.7 10.8 4.3 31.5 Serum potassium increased0.6 0.0 2.2 1.1 Serum sodium decreased1.9 1.5 3.2 1.1 Serum uric acid increased0.6 0.0 0.0 3.4 Total serum bilirubin increased0.0 0.0 3.2 4.5 Total serum protein decreased3.1 0.0 3.2 3.4 HematologyEosinophils increased3.1 3.1 1.1 1.1 Hematocrit decreased11.1 1.5 5.4 32.6 Hemoglobin decreased12.3 3.1 5.4 37.1 Lymphocytes increased0.0 1.6 2.2 0.0 Neutrophils decreased1.9 3.1 3.2 1.1 Platelet count decreased3.1 1.5 2.2 3.4 Prothrombin time increased1.3 1.5 0.0 2.3 WBC count decreased6.2 4.6 8.6 7.9 UrinalysisUrine blood increased0.0 0.0 0.0 4.0 Urine casts increased0.0 0.0 0.0 8.0 Urine pH increased0.8 0.0 0.0 3.6 Urine protein increased1.2 0.0 3.3 4.5 Urine RBCs increased1.1 3.8 5.1 12.0 Urine WBCs increased0.0 7.7 0.0 24.0 *Relationship to drug was determined by the investigator to be possibly, probably or definitely drug-related.**Derived from Phase II and Phase III comparator-controlled clinical studies.***Derived from Phase II comparator-controlled clinical studies.Invasive Aspergillosis
In the open-label, noncomparative aspergillosis study, in which 69 patients received CANCIDAS (70-mg loading dose on Day 1 followed by 50 mg daily), the following drug-related clinical adverse experiences were observed with an incidence of >/=2%: fever (2.9%), infused-vein complications (2.9%), nausea (2.9%), vomiting (2.9%) and flushing (2.9%).
Also reported infrequently in this patient population were pulmonary edema, ARDS, and radiographic infiltrates.
Drug-related laboratory abnormalities reported with an incidence >/=2% in patients treated with CANCIDAS in the noncomparative aspergillosis study were: serum alkaline phosphatase increased (2.9%), serum potassium decreased (2.9%), eosinophils increased (3.2%), urine protein increased (4.9%), and urine RBCs increased (2.2%).
Postmarketing Experience:
The following postmarketing adverse events have been reported:
Hepatobiliary: rare cases of clinically significant hepatic dysfunction
Cardiovascular: swelling and peripheral edema
Metabolic: hypercalcemia
Concomitant Therapy
In one clinical study, 3 of 4 subjects who received CANCIDAS 70 mg daily on Days 1 through 10, and also received two 3 mg/kg doses of cyclosporine 12 hours apart on Day 10, developed transient elevations of ALT on Day 11 that were 2 to 3 times the upper limit of normal (ULN). In a separate panel of subjects in the same study, 2 of 8 subjects who received CANCIDAS 35 mg daily for 3 days and cyclosporine (two 3 mg/kg doses administered 12 hours apart) on Day 1 had small increases in ALT (slightly above the ULN) on Day 2. In another clinical study, 2 of 8 healthy men developed transient ALT elevations of less than 2 × ULN. In this study, cyclosporine (4 mg/kg) was administered on Days 1 and 12, and CANCIDAS was administered (70 mg) daily on Days 3 through 13. In one subject, the ALT elevation occurred on Days 7 and 9 and, in the other subject, the ALT elevation occurred on Day 19. These elevations returned to normal by Day 27. In all groups, elevations in AST paralleled ALT elevations but were of lesser magnitude. In these clinical studies, cyclosporine (one 4 mg/kg dose or two 3 mg/kg doses) increased the AUC of caspofungin by approximately 35% (see WARNINGS ).
OVERDOSAGE
In clinical studies the highest dose was 210 mg, administered as a single dose to 6 healthy subjects. This dose was generally well tolerated. In addition, 100 mg once daily for 21 days has been administered to 15 healthy subjects and was generally well tolerated. Caspofungin is not dialyzable. The minimum lethal dose of caspofungin in rats was 50 mg/kg, a dose which is equivalent to 10 times the re-commended daily dose based on relative body surface area comparison.
ANIMAL PHARMACOLOGY AND TOXICOLOGY
In one 5-week study in monkeys at doses which produced exposures approximately 4 to 6 times those seen in patients treated with a 70-mg dose, scattered small foci of subcapsular necrosis were observed microscopically in the livers of some animals (2/8 monkeys at 5 mg/kg and 4/8 monkeys at 8 mg/kg); however, this histopathological finding was not seen in another study of 27 weeks duration at similar doses.
DOSAGE AND ADMINISTRATION
Do not mix or co-infuse CANCIDAS with other medications, as there are no data available on the compatibility of CANCIDAS with other intravenous substances, additives, or medications. DO NOT USE DILUENTS CONTAINING DEXTROSE ((alpha)-D-GLUCOSE), as CANCIDAS is not stable in diluents containing dextrose. CANCIDAS should be administered by slow IV infusion over approximately 1 hour.
Empirical Therapy
A single 70-mg loading dose should be administered on Day 1, followed by 50 mg daily thereafter. Duration of treatment should be based on the patient's clinical response. Empirical therapy should be continued until resolution of neutropenia. Patients found to have a fungal infection should be treated for a minimum of 14 days; treatment should continue for at least 7 days after both neutropenia and clinical symptoms are resolved. If the 50-mg dose is well tolerated but does not provide an adequate clinical response, the daily dose can be increased to 70 mg. Although an increase in efficacy with 70 mg daily has not been demonstrated, limited safety data suggest that an increase in dose to 70 mg daily is well tolerated.
Candidemia and other Candida infections (see CLINICAL STUDIES )
A single 70-mg loading dose should be administered on Day 1, followed by 50 mg daily thereafter. Duration of treatment should be dictated by the patient's clinical and microbiological response. In general, antifungal therapy should continue for at least 14 days after the last positive culture. Patients who remain persistently neutropenic may warrant a longer course of therapy pending resolution of the neutropenia.
Esophageal Candidiasis
The dose should be 50 mg daily. Because of the risk of relapse of oropharyngeal candidiasis in patients with HIV infections, suppressive oral therapy could be considered (see CLINICAL STUDIES ). A 70-mg loading dose has not been studied with this indication.
Invasive Aspergillosis
A single 70-mg loading dose should be administered on Day 1, followed by 50 mg daily thereafter. Duration of treatment should be based upon the severity of the patient's underlying disease, recovery from immunosuppression, and clinical response. The efficacy of a 70-mg dose regimen in patients who are not clinically responding to the 50-mg daily dose is not known. Limited safety data suggest that an increase in dose to 70 mg daily is well tolerated. The safety and efficacy of doses above 70 mg have not been adequately studied.
Hepatic Insufficiency
Patients with mild hepatic insufficiency (Child-Pugh score 5 to 6) do not need a dosage adjustment. For patients with moderate hepatic insufficiency (Child-Pugh score 7 to 9), CANCIDAS 35 mg daily is recommended. However, where recommended, a 70-mg loading dose should still be administered on Day 1. There is no clinical experience in patients with severe hepatic insufficiency (Child-Pugh score >9).
Concomitant Medication with Inducers of Drug Clearance
Patients on rifampin should receive 70 mg of CANCIDAS daily. Patients on nevirapine, efavirenz, carbamazepine, dexamethasone, or phenytoin may require an increase in dose to 70 mg of CANCIDAS daily (see PRECAUTIONS , Drug Interactions ).
Preparation of CANCIDAS for use:
Do not mix or co-infuse CANCIDAS with other medications, as there are no data available on the compatibility of CANCIDAS with other intravenous substances, additives, or medications. DO NOT USE DILUENTS CONTAINING DEXTROSE ((alpha)-D-GLUCOSE), as CANCIDAS is not stable in diluents containing dextrose.
Preparation of the 70-mg infusion
- Equilibrate the refrigerated vial of CANCIDAS to room temperature.
- Aseptically add 10.5 mL of 0.9% Sodium Chloride Injection, Sterile Water for Injection, Bacteriostatic Water for Injection with methylparaben and propylparaben, or Bacteriostatic Water for Injection with 0.9% benzyl alcohol to the vial. a This reconstituted solution may be stored for up to one hour at </=25°C (</=77°F). b
- Aseptically transfer 10 mL c of reconstituted CANCIDAS to an IV bag (or bottle) containing 250 mL 0.9%, 0.45%, or 0.225% Sodium Chloride Injection, or Lactated Ringer's Injection. This infusion solution must be used within 24 hours if stored at </=25°C (</=77°F) or within 48 hours if stored refrigerated at 2 to 8°C (36 to 46°F). (If a 70-mg vial is unavailable, see below: Alternative Infusion Preparation Methods, Preparation of 70-mg dose from two 50-mg vials .)
Preparation of the daily 50-mg infusion
- Equilibrate the refrigerated vial of CANCIDAS to room temperature.
- Aseptically add 10.5 mL of 0.9% Sodium Chloride Injection, Sterile Water for Injection, Bacteriostatic Water for Injection with methylparaben and propylparaben, or Bacteriostatic Water for Injection with 0.9% benzyl alcohol to the vial. a This reconstituted solution may be stored for up to one hour at </=25°C (</=77°F). b
- Aseptically transfer 10 mL c of reconstituted CANCIDAS to an IV bag (or bottle) containing 250 mL 0.9%, 0.45%, or 0.225% Sodium Chloride Injection, or Lactated Ringer's Injection. This infusion solution must be used within 24 hours if stored at </=25°C (</=77°F) or within 48 hours if stored refrigerated at 2 to 8°C (36 to 46°F). (If a reduced infusion volume is medically necessary, see below: Alternative Infusion Preparation Methods, Preparation of 50-mg daily doses at reduced volume .)
Alternative Infusion Preparation Methods
Preparation of 70-mg dose from two 50-mg vials
Reconstitute two 50-mg vials with 10.5 mL of diluent each (see Preparation of the daily 50-mg infusion ). Aseptically transfer a total of 14 mL of the reconstituted CANCIDAS from the two vials to 250 mL of 0.9%, 0.45%, or 0.225% Sodium Chloride Injection, or Lactated Ringer's Injection.
Preparation of 50-mg daily doses at reduced volume
When medically necessary, the 50-mg daily doses can be prepared by adding 10 mL of reconstituted CANCIDAS to 100 mL of 0.9%, 0.45%, or 0.225% Sodium Chloride Injection, or Lactated Ringer's Injection (see Preparation of the daily 50-mg infusion ).
Preparation of a 35-mg daily dose for patients with moderate Hepatic Insufficiency
Reconstitute one 50-mg vial (see above: Preparation of the daily 50-mg infusion ). Aseptically transfer 7 mL of the reconstituted CANCIDAS from the vial to 250 mL or, if medically necessary, to 100 mL of 0.9%, 0.45%, or 0.225% Sodium Chloride Injection, or Lactated Ringer's Injection.
Preparation notes:
a The white to off-white cake will dissolve completely. Mix gently until a clear solution is obtained.
b Visually inspect the reconstituted solution for particulate matter or discoloration during reconstitution and prior to infusion. Do not use if the solution is cloudy or has precipitated.
c CANCIDAS is formulated to provide the full labeled vial dose (70 mg or 50 mg) when 10 mL is withdrawn from the vial.
TABLE 14
CANCIDAS ConcentrationsDoseReconstituted Solution Concentration Infusion Volume Infusion Solution Concentration 70-mg initial dose7.2 mg/mL 260 mL 0.28 mg/mL 50-mg daily dose5.2 mg/mL 260 mL 0.20 mg/mL 70-mg initial dose *(from two 50 mg vials)5.2 mg/mL 264 mL 0.28 mg/mL 50-mg daily dose *(reduced volume)5.2 mg/mL 110 mL 0.47 mg/mL 35-mg daily dose *5.2 mg/mL 257 mL 0.14 mg/mL (from one 50 mg vial) for Moderateor or or Hepatic Insufficiency5.2 mg/mL 107 mL 0.34 mg/mL *See preceding text for these special situations.HOW SUPPLIED
No. 3822 -- CANCIDAS 50 mg is a white to off-white powder/cake for infusion in a vial with a red aluminum band and a plastic cap.
NDC 0006-3822-10 supplied as one single-use vial.
No. 3823 -- CANCIDAS 70 mg is a white to off-white powder/cake for infusion in a vial with a yellow/orange aluminum band and a plastic cap.
NDC 0006-3823-10 supplied as one single-use vial.
Storage
Vials
The lyophilized vials should be stored refrigerated at 2° to 8°C (36° to 46°F).
Reconstituted Concentrate
Reconstituted CANCIDAS may be stored at </=25°C (</=77°F) for one hour prior to the preparation of the patient infusion solution.
Diluted Product
The final patient infusion solution in the IV bag or bottle can be stored at </=25°C (</=77°F) for 24 hours or at 2 to 8°C (36 to 46°F) for 48 hours.
Manufactured for:Merck & CO., INC., Whitehouse Station, NJ 08889, USA
Manufactured by:
Merck & CO., INC., Whitehouse Station, NJ 08889, USA
or
Cardinal Health
Albuquerque, NM 87109
9344307 Issued February 2005
COPYRIGHT© Merck & CO., Inc., 2001
All rights reserved
Subscribe to the "News" RSS Feed 
TOP ۞
