-
Coreg Tablets (Glaxosmithkline)
DESCRIPTION
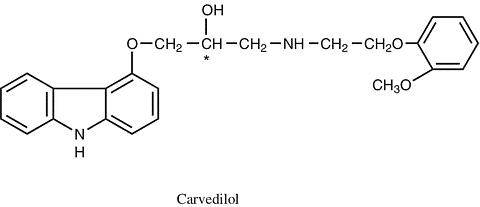
Carvedilol is a nonselective (beta)-adrenergic blocking agent with (alpha) 1 -blocking activity. It is (±)-1-(Carbazol-4-yloxy)-3-[[2-(o-methoxyphenoxy)ethyl]amino]-2-propanol. It is a racemic mixture with the following structure:
Tablets for Oral Administration: COREG (carvedilol) is a white, oval, film-coated tablet containing 3.125 mg, 6.25 mg, 12.5 mg, or 25 mg of carvedilol. The 6.25 mg, 12.5 mg, and 25 mg tablets are TILTAB® tablets. Inactive ingredients consist of colloidal silicon dioxide, crospovidone, hypromellose, lactose, magnesium stearate, polyethylene glycol, polysorbate 80, povidone, sucrose, and titanium dioxide.
Carvedilol is a white to off-white powder with a molecular weight of 406.5 and a molecular formula of C 24 H 26 N 2 O 4 . It is freely soluble in dimethylsulfoxide; soluble in methylene chloride and methanol; sparingly soluble in 95% ethanol and isopropanol; slightly soluble in ethyl ether; and practically insoluble in water, gastric fluid (simulated, TS, pH 1.1), and intestinal fluid (simulated, TS without pancreatin, pH 7.5).
CLINICAL PHARMACOLOGY
COREG is a racemic mixture in which nonselective (beta)-adrenoreceptor blocking activity is present in the S(-) enantiomer and (alpha)-adrenergic blocking activity is present in both R(+) and S(-) enantiomers at equal potency. COREG has no intrinsic sympathomimetic activity.
Pharmacokinetics: COREG is rapidly and extensively absorbed following oral administration, with absolute bioavailability of approximately 25% to 35% due to a significant degree of first-pass metabolism. Following oral administration, the apparent mean terminal elimination half-life of carvedilol generally ranges from 7 to 10 hours. Plasma concentrations achieved are proportional to the oral dose administered. When administered with food, the rate of absorption is slowed, as evidenced by a delay in the time to reach peak plasma levels, with no significant difference in extent of bioavailability. Taking COREG with food should minimize the risk of orthostatic hypotension.
Carvedilol is extensively metabolized. Following oral administration of radiolabelled carvedilol to healthy volunteers, carvedilol accounted for only about 7% of the total radioactivity in plasma as measured by area under the curve (AUC). Less than 2% of the dose was excreted unchanged in the urine. Carvedilol is metabolized primarily by aromatic ring oxidation and glucuronidation. The oxidative metabolites are further metabolized by conjugation via glucuronidation and sulfation. The metabolites of carvedilol are excreted primarily via the bile into the feces. Demethylation and hydroxylation at the phenol ring produce three active metabolites with (beta)-receptor blocking activity. Based on preclinical studies, the 4'-hydroxyphenyl metabolite is approximately 13 times more potent than carvedilol for (beta)-blockade.
Compared to carvedilol, the three active metabolites exhibit weak vasodilating activity. Plasma concentrations of the active metabolites are about one-tenth of those observed for carvedilol and have pharmacokinetics similar to the parent.
Carvedilol undergoes stereoselective first-pass metabolism with plasma levels of R(+)-carvedilol approximately 2 to 3 times higher than S(-)-carvedilol following oral administration in healthy subjects. The mean apparent terminal elimination half-lives for R(+)-carvedilol range from 5 to 9 hours compared with 7 to 11 hours for the S(-)-enantiomer.
The primary P450 enzymes responsible for the metabolism of both R(+) and S(-)-carvedilol in human liver microsomes were CYP2D6 and CYP2C9 and to a lesser extent CYP3A4, 2C19, 1A2, and 2E1. CYP2D6 is thought to be the major enzyme in the 4'- and 5'-hydroxylation of carvedilol, with a potential contribution from 3A4. CYP2C9 is thought to be of primary importance in the O-methylation pathway of S(-)-carvedilol.
Carvedilol is subject to the effects of genetic polymorphism with poor metabolizers of debrisoquin (a marker for cytochrome P450 2D6) exhibiting 2- to 3-fold higher plasma concentrations of R(+)-carvedilol compared to extensive metabolizers. In contrast, plasma levels of S(-)-carvedilol are increased only about 20% to 25% in poor metabolizers, indicating this enantiomer is metabolized to a lesser extent by cytochrome P450 2D6 than R(+)-carvedilol. The pharmacokinetics of carvedilol do not appear to be different in poor metabolizers of S-mephenytoin (patients deficient in cytochrome P450 2C19).
Carvedilol is more than 98% bound to plasma proteins, primarily with albumin. The plasma-protein binding is independent of concentration over the therapeutic range. Carvedilol is a basic, lipophilic compound with a steady-state volume of distribution of approximately 115 L, indicating substantial distribution into extravascular tissues. Plasma clearance ranges from 500 to 700 mL/min.
Congestive Heart Failure: Steady-state plasma concentrations of carvedilol and its enantiomers increased proportionally over the 6.25 to 50 mg dose range in patients with congestive heart failure. Compared to healthy subjects, congestive heart failure patients had increased mean AUC and C max values carvedilol and its enantiomers, with up to 50% to 100% higher values observed in 6 patients with NYHA class IV heart failure. The mean apparent terminal elimination half-life for carvedilol was similar to that observed in healthy subjects.
Pharmacokinetic Drug-Drug Interactions: Since carvedilol undergoes substantial oxidative metabolism, the metabolism and pharmacokinetics of carvedilol may be affected by induction or inhibition of cytochrome P450 enzymes.
Rifampin: In a pharmacokinetic study conducted in 8 healthy male subjects, rifampin (600 mg daily for 12 days) decreased the AUC and C max of carvedilol by about 70%.
Cimetidine: In a pharmacokinetic study conducted in 10 healthy male subjects, cimetidine (1000 mg/day) increased the steady-state AUC of carvedilol by 30% with no change in C max .
Glyburide: In 12 healthy subjects, combined administration of carvedilol (25 mg once daily) and a single dose of glyburide did not result in a clinically relevant pharmacokinetic interaction for either compound.
Hydrochlorothiazide: A single oral dose of carvedilol 25 mg did not alter the pharmacokinetics of a single oral dose of hydrochlorothiazide 25 mg in 12 patients with hypertension. Likewise, hydrochlorothiazide had no effect on the pharmacokinetics of carvedilol.
Digoxin: Following concomitant administration of carvedilol (25 mg once daily) and digoxin (0.25 mg once daily) for 14 days, steady-state AUC and trough concentrations of digoxin were increased by 14% and 16%, respectively, in 12 hypertensive patients.
Torsemide: In a study of 12 healthy subjects, combined oral administration of carvedilol 25 mg once daily and torsemide 5 mg once daily for 5 days did not result in any significant differences in their pharmacokinetics compared with administration of the drugs alone.
Warfarin: Carvedilol (12.5 mg twice daily) did not have an effect on the steady-state prothrombin time ratios and did not alter the pharmacokinetics of R(+)- and S(-)-warfarin following concomitant administration with warfarin in 9 healthy volunteers.
Special Populations: Elderly: Plasma levels of carvedilol average about 50% higher in the elderly compared to young subjects.
Hepatic Impairment: Compared to healthy subjects, patients with cirrhotic liver disease exhibit significantly higher concentrations of carvedilol (approximately 4- to 7-fold) following single-dose therapy.
Renal Insufficiency: Although carvedilol is metabolized primarily by the liver, plasma concentrations of carvedilol have been reported to be increased in patients with renal impairment. Based on mean AUC data, approximately 40% to 50% higher plasma concentrations of carvedilol were observed in hypertensive patients with moderate to severe renal impairment compared to a control group of hypertensive patients with normal renal function. However, the ranges of AUC values were similar for both groups. Changes in mean peak plasma levels were less pronounced, approximately 12% to 26% higher in patients with impaired renal function.
Consistent with its high degree of plasma protein-binding, carvedilol does not appear to be cleared significantly by hemodialysis.
Pharmacodynamics: Congestive Heart Failure: The basis for the beneficial effects of COREG in congestive heart failure is not established.
Two placebo-controlled studies compared the acute hemodynamic effects of COREG to baseline measurements in 59 and 49 patients with NYHA class II-IV heart failure receiving diuretics, ACE inhibitors, and digitalis. There were significant reductions in systemic blood pressure, pulmonary artery pressure, pulmonary capillary wedge pressure, and heart rate. Initial effects on cardiac output, stroke volume index, and systemic vascular resistance were small and variable.
These studies measured hemodynamic effects again at 12 to 14 weeks. COREG significantly reduced systemic blood pressure, pulmonary artery pressure, right atrial pressure, systemic vascular resistance, and heart rate, while stroke volume index was increased.
Among 839 patients with NYHA class II-III heart failure treated for 26 to 52 weeks in 4 US placebo-controlled trials, average left ventricular ejection fraction (EF) measured by radionuclide ventriculography increased by 9 EF units (%) in COREG patients and by 2 EF units in placebo patients at a target dose of 25-50 mg twice daily. The effects of carvedilol on ejection fraction were related to dose. Doses of 6.25 mg twice daily, 12.5 mg twice daily, and 25 mg twice daily were associated with placebo-corrected increases in EF of 5 EF units, 6 EF units, and 8 EF units, respectively; each of these effects were nominally statistically significant.
Left Ventricular Dysfunction Following Myocardial Infarction: The basis for the beneficial effects of COREG in patients with left ventricular dysfunction following an acute myocardial infarction is not established.
Hypertension: The mechanism by which (beta)-blockade produces an antihypertensive effect has not been established.
(beta)-adrenoreceptor blocking activity has been demonstrated in animal and human studies showing that carvedilol (1) reduces cardiac output in normal subjects; (2) reduces exercise- and/or isoproterenol-induced tachycardia; and (3) reduces reflex orthostatic tachycardia. Significant (beta)-adrenoreceptor blocking effect is usually seen within 1 hour of drug administration.
(alpha) 1 -adrenoreceptor blocking activity has been demonstrated in human and animal studies, showing that carvedilol (1) attenuates the pressor effects of phenylephrine; (2) causes vasodilation; and (3) reduces peripheral vascular resistance. These effects contribute to the reduction of blood pres-sure and usually are seen within 30 minutes of drug administration.
Due to the (alpha) 1 -receptor blocking activity of carvedilol, blood pressure is lowered more in the standing than in the supine position, and symptoms of postural hypotension (1.8%), including rare instances of syncope, can occur. Following oral administration, when postural hypotension has occurred, it has been transient and is uncommon when COREG is administered with food at the recommended starting dose and titration increments are closely followed (see DOSAGE AND ADMINISTRATION ).
In hypertensive patients with normal renal function, therapeutic doses of COREG decreased renal vascular resistance with no change in glomerular filtration rate or renal plasma flow. Changes in excretion of sodium, potassium, uric acid, and phosphorus in hypertensive patients with normal renal function were similar after COREG and placebo.
COREG has little effect on plasma catecholamines, plasma aldosterone, or electrolyte levels, but it does significantly reduce plasma renin activity when given for at least 4 weeks. It also increases levels of atrial natriuretic peptide.
CLINICAL TRIALS
Congestive Heart Failure: A total of 6,975 patients with mild to severe heart failure were evaluated in placebo-controlled studies of carvedilol.
Trials in Mild-to-Moderate Heart Failure: Carvedilol was studied in 5 multicenter, placebo-controlled studies, and in 1 active-controlled study (COMET study) involving patients with mild-to-moderate heart failure.
Four US multicenter, double-blind, placebo-controlled studies enrolled 1,094 patients (696 randomized to carvedilol) with NYHA class II-III heart failure and ejection fraction </=0.35. The vast majority were on digitalis, diuretics, and an ACE inhibitor at study entry. Patients were assigned to the studies based upon exercise ability. An Australia-New Zealand double-blind, placebo-controlled study enrolled 415 patients (half randomized to carvedilol) with less severe heart failure. All protocols excluded patients expected to undergo cardiac transplantation during the 7.5 to 15 months of double-blind follow-up. All randomized patients had tolerated a 2-week course on carvedilol 6.25 mg twice daily.
In each study, there was a primary end point, either progression of heart failure (1 US study) or exercise tolerance (2 US studies meeting enrollment goals and the Australia-New Zealand study). There were many secondary end points specified in these studies, including NYHA classification, patient and physician global assessments, and cardiovascular hospitalization. Other analyses not prospectively planned included the sum of deaths and total cardiovascular hospitalizations. In situations where the primary end points of a trial do not show a significant benefit of treatment, assignment of significance values to the other results is complex, and such values need to be interpreted cautiously.
The results of the US and Australia-New Zealand trials were as follows:
Slowing Progression of Heart Failure: One US multicenter study (366 subjects) had as its primary end point the sum of cardiovascular mortality, cardiovascular hospitalization, and sustained increase in heart failure medications. Heart failure progression was reduced, during an average follow-up of 7 months, by 48% (p = 0.008).
In the Australia-New Zealand study, death and total hospitalizations were reduced by about 25% over 18 to 24 months. In the 3 largest US studies, death and total hospitalizations were reduced by 19%, 39%, and 49%, nominally statistically significant in the last 2 studies. The Australia-New Zealand results were statistically borderline.
Functional Measures: None of the multicenter studies had NYHA classification as a primary end point, but all such studies had it as a secondary end point. There was at least a trend toward improvement in NYHA class in all studies. Exercise tolerance was the primary end point in 3 studies; in none was a statistically significant effect found.
Subjective Measures: Quality of life, as measured with a standard questionnaire (a primary end point in 1 study), was unaffected by carvedilol. However, patients' and investigators' global assessments showed significant improvement in most studies.
Mortality: Death was not a pre-specified end-point in any study, but was analyzed in all studies. Overall, in these 4 US trials, mortality was reduced, nominally significantly so in 2 studies.
The COMET Trial: In this double-blind trial, 3,029 patients with NYHA class II-IV heart failure (left ventricular ejection fraction </=35%) were randomized to receive either carvedilol (target dose: 25 mg twice daily) or immediate-release metoprolol tartrate (target dose: 50 mg twice daily). The mean age of the patients was approximately 62 years, 80% were males, and the mean left ventricular ejection fraction at baseline was 26%. Approximately 96% of the patients had NYHA class II or III heart failure. Concomitant treatment included diuretics (99%), ACE inhibitors (91%), digitalis (59%), aldosterone antagonists (11%), and "statin" lipid-lowering agents (21%). The mean duration of follow-up was 4.8 years. The mean dose of carvedilol was 42 mg per day.
The study had 2 primary endpoints: all-cause mortality and the composite of death plus hospitalization for any reason. All-cause mortality carried most of the statistical weight and was the primary determinant of the study size. All-cause mortality was 34% in the patients treated with carvedilol and was 40% in the immediate-release metoprolol group (p=0.0017; hazard ratio=0.83, 95% CI 0.74-0.93). The difference between the 2 groups with respect to the composite endpoint was not significant (p=0.122). The estimated mean survival was 8.0 years with carvedilol and 6.6 years with immediate-release metoprolol.
It is not known whether this formulation of metoprolol at any dose or this low dose of metoprolol in any formulation has any effect on survival or hospitalization in patients with heart failure. Thus, this trial extends the time over which carvedilol manifests benefits on survival in heart failure, but it is not evidence that carvedilol improves outcome over the formulation of metoprolol (Toprol XL) with benefits in heart failure.
Trials in Severe Heart Failure: In a double-blind study (COPERNICUS), 2,289 patients with heart failure at rest or with minimal exertion and left ventricular ejection fraction <25% (mean 20%), despite digitalis (66%), diuretics (99%), and ACE inhibitors (89%) were randomized to placebo or carvedilol. Carvedilol was titrated from a starting dose of 3.125 mg twice daily to the maximum tolerated dose or up to 25 mg twice daily over a minimum of 6 weeks. Most subjects achieved the target dose of 25 mg. The study was conducted in Eastern and Western Europe, the United States, Israel, and Canada. Similar numbers of subjects per group (about 100) withdrew during the titration period.
The primary end point of the trial was all-cause mortality, but cause-specific mortality and the risk of death or hospitalization (total, cardiovascular CV, or congestive heart failure [CHF]) were also examined. The developing trial data were followed by a data monitoring committee, and mortality analyses were adjusted for these multiple looks. The trial was stopped after a median follow-up of 10 months because of an observed 35% reduction in mortality (from 19.7% per patient year on placebo to 12.8% on carvedilol, hazard ratio 0.65, 95% CI 0.52 - 0.81, p = 0.0014, adjusted) (see Figure 1). The results of COPERNICUS are shown in Table 1.
Table 1. Results of COPERNICUS End point Placebo
N = 1,133Carvedilol
N = 1,156Hazard ratio
(95% CI)%
ReductionNominal
p valueMortality 190 130 0.65
(0.52 - 0.81)35 0.00013 Mortality + all
hospitalization507 425 0.76
(0.67 - 0.87)24 0.00004 Mortality + CV
hospitalization395 314 0.73
(0.63 - 0.84)27 0.00002 Mortality + CHF
hospitalization357 271 0.69
(0.59 - 0.81)31 0.000004 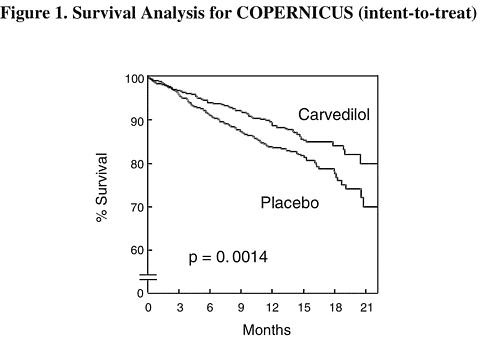
The effect on mortality was principally the result of a reduction in the rate of sudden death among patients without worsening heart failure.
Patients' global assessments, in which carvedilol-treated patients were compared to placebo, were based on pre-specified, periodic patient self-assessments regarding whether clinical status post-treatment showed improvement, worsening or no change compared to baseline. Patients treated with carvedilol showed significant improvements in global assessments compared with those treated with placebo in COPERNICUS.
The protocol also specified that hospitalizations would be assessed. Fewer patients on COREG than on placebo were hospitalized for any reason (372 vs. 432, p = 0.0029), for cardiovascular reasons (246 vs. 314, p = 0.0003), or for worsening heart failure (198 vs. 268, p = 0.0001).
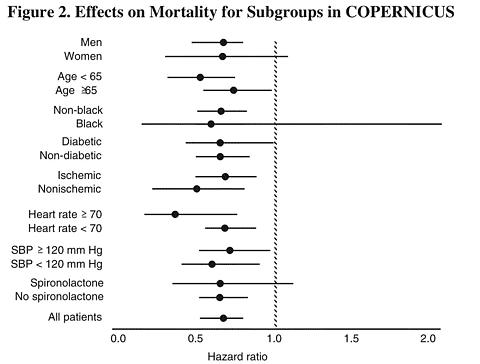
COREG had a consistent and beneficial effect on all-cause mortality as well as the combined end points of all-cause mortality plus hospitalization (total, CV, or for heart failure) in the overall study population and in all subgroups examined, including men and women, elderly and non-elderly, blacks and non-blacks, and diabetics and non-diabetics (see Figure 2).
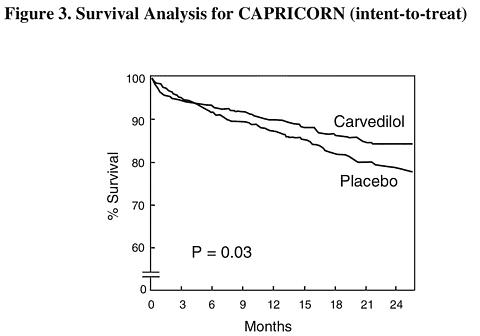
Left Ventricular Dysfunction Following Myocardial Infarction: CAPRICORN was a double-blind study comparing carvedilol and placebo in 1,959 patients with a recent myocardial infarction (within 21 days) and left ventricular ejection fraction of </=40%, with (47%) or without symptoms of heart failure. Patients given carvedilol received 6.25 mg twice daily, titrated as tolerated to 25 mg twice daily. Patients had to have a systolic blood pressure >90 mm Hg, a sitting heart rate >60 beats/minute, and no contraindication to (beta)-blocker use. Treatment of the index infarction included aspirin (85%), IV or oral (beta)-blockers (37%), nitrates (73%), heparin (64%), thrombolytics (40%), and acute angioplasty (12%). Background treatment included ACE inhibitors or angiotensin receptor blockers (97%), anticoagulants (20%), lipid-lowering agents (23%), and diuretics (34%). Baseline population characteristics included an average age of 63 years, 74% male, 95% Caucasian, mean blood pressure 121/74 mm Hg, 22% with diabetes, and 54% with a history of hypertension. Mean dosage achieved of carvedilol was 20 mg twice daily; mean duration of follow-up was 15 months.
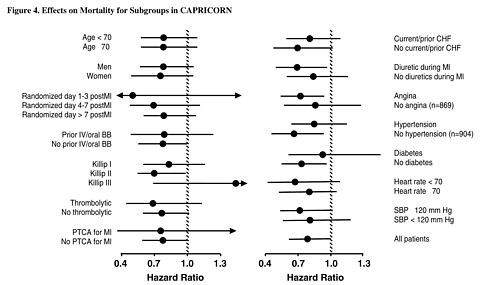
All-cause mortality was 15% in the placebo group and 12% in the carvedilol group, indicating a 23% risk reduction in patients treated with carvedilol (95% CI 2-40%, p = 0.03), as shown in Figure 3. The effects on mortality in various subgroups are shown in Figure 4. Nearly all deaths were cardiovascular (which were reduced by 25% by carvedilol), and most of these deaths were sudden or related to pump failure (both types of death were reduced by carvedilol). Another study endpoint, total mortality and all-cause hospitalization, did not show a significant improvement.
There was also a significant 40% reduction in fatal or non-fatal myocardial infarction observed in the group treated with carvedilol (95% CI 11% to 60%, p = 0.01). A similar reduction in the risk of myocardial infarction was also observed in a meta-analysis of placebo-controlled trials of carvedilol in heart failure.
Hypertension: COREG was studied in 2 placebo-controlled trials that utilized twice-daily dosing, at total daily doses of 12.5 to 50 mg. In these and other studies, the starting dose did not exceed 12.5 mg. At 50 mg/day, COREG reduced sitting trough (12-hour) blood pressure by about 9/5.5 mm Hg; at 25 mg/day the effect was about 7.5/3.5 mm Hg. Comparisons of trough to peak blood pressure showed a trough to peak ratio for blood pressure response of about 65%. Heart rate fell by about 7.5 beats/minute at 50 mg/day. In general, as is true for other (beta)-blockers, responses were smaller in black than non-black patients. There were no age- or gender-related differences in response.
The peak antihypertensive effect occurred 1 to 2 hours after a dose. The dose-related blood pressure response was accompanied by a dose-related increase in adverse effects (see ADVERSE REACTIONS ).
INDICATIONS AND USAGE
Congestive Heart Failure: COREG is indicated for the treatment of mild-to-severe heart failure of ischemic or cardiomyopathic origin, usually in addition to diuretics, ACE inhibitor, and digitalis, to increase survival and, also, to reduce the risk of hospitalization (see CLINICAL TRIALS ).
Left Ventricular Dysfunction Following Myocardial Infarction: COREG is indicated to reduce cardiovascular mortality in clinically stable patients who have survived the acute phase of a myocardial infarction and have a left ventricular ejection fraction of </=40% (with or without symptomatic heart failure) (see CLINICAL TRIALS ).
Hypertension: COREG is also indicated for the management of essential hypertension. It can be used alone or in combination with other antihypertensive agents, especially thiazide-type diuretics (see PRECAUTIONS , Drug Interactions ).
CONTRAINDICATIONS
COREG is contraindicated in patients with bronchial asthma (2 cases of death from status asthmaticus have been reported in patients receiving single doses of COREG) or related bronchospastic conditions, second- or third-degree AV block, sick sinus syndrome or severe bradycardia (unless a permanent pacemaker is in place), or in patients with cardiogenic shock or who have decompensated heart failure requiring the use of intravenous inotropic therapy. Such patients should first be weaned from intravenous therapy before initiating COREG.
Use of COREG in patients with clinically manifest hepatic impairment is not recommended.
COREG is contraindicated in patients with hypersensitivity to any component of the product.
WARNINGS
Cessation of Therapy with COREG: Patients with coronary artery disease, who are being treated with COREG, should be advised against abrupt discontinuation of therapy. Severe exacerbation of angina and the occurrence of myocardial infarction and ventricular arrhythmias have been reported in angina patients following the abrupt discontinuation of therapy with (beta)-blockers. The last 2 complications may occur with or without preceding exacerbation of the angina pectoris. As with other (beta)-blockers, when discontinuation of COREG is planned, the patients should be carefully observed and advised to limit physical activity to a minimum. COREG should be discontinued over 1 to 2 weeks whenever possible. If the angina worsens or acute coronary insufficiency develops, it is recommended that COREG be promptly reinstituted, at least temporarily. Because coronary artery disease is common and may be unrecognized, it may be prudent not to discontinue COREG therapy abruptly even in patients treated only for hypertension or heart failure (See DOSAGE AND ADMINISTRATION .)
Peripheral Vascular Disease: (beta)-blockers can precipitate or aggravate symptoms of arterial insufficiency in patients with peripheral vascular disease. Caution should be exercised in such individuals.
Anesthesia and Major Surgery: If treatment with COREG is to be continued perioperatively, particular care should be taken when anesthetic agents which depress myocardial function, such as ether, cyclopropane, and trichloroethylene, are used. See OVERDOSAGE for information on treatment of bradycardia and hypertension.
Diabetes and Hypoglycemia: In general, (beta)-blockers may mask some of the manifestations of hypoglycemia, particularly tachycardia. Nonselective (beta)-blockers may potentiate insulin-induced hypoglycemia and delay recovery of serum glucose levels. Patients subject to spontaneous hypoglycemia, or diabetic patients receiving insulin or oral hypoglycemic agents, should be cautioned about these possibilities. In congestive heart failure patients, there is a risk of worsening hyperglycemia (see PRECAUTIONS ).
Thyrotoxicosis: (beta)-adrenergic blockade may mask clinical signs of hyperthyroidism, such as tachycardia. Abrupt withdrawal of (beta)-blockade may be followed by an exacerbation of the symptoms of hyperthyroidism or may precipitate thyroid storm.
PRECAUTIONS
General: In clinical trials, COREG caused bradycardia in about 2% of hypertensive patients, 9% of congestive heart failure patients, and 6.5% of myocardial infarction patients with left ventricular dysfunction. If pulse rate drops below 55 beats/minute, the dosage should be reduced.
In clinical trials of primarily mild-to-moderate heart failure, hypotension and postural hypotension occurred in 9.7% and syncope in 3.4% of patients receiving COREG compared to 3.6% and 2.5% of placebo patients, respectively. The risk for these events was highest during the first 30 days of dosing, corresponding to the up-titration period and was a cause for discontinuation of therapy in 0.7% of COREG patients, compared to 0.4% of placebo patients. In a long-term, placebo-controlled trial in severe heart failure (COPERNICUS), hypotension and postural hypotension occurred in 15.1% and syncope in 2.9% of heart failure patients receiving COREG compared to 8.7% and 2.3% of placebo patients, respectively. These events were a cause for discontinuation of therapy in 1.1% of COREG patients, compared to 0.8% of placebo patients.
Postural hypotension occurred in 1.8% and syncope in 0.1% of hypertensive patients, primarily following the initial dose or at the time of dose increase and was a cause for discontinuation of therapy in 1% of patients.
In the CAPRICORN study of survivors of an acute myocardial infarction, hypotension or postural hypotension occurred in 20.2% of patients receiving COREG compared to 12.6% of placebo patients. Syncope was reported in 3.9% and 1.9% of patients, respectively. These events were a cause for discontinuation of therapy in 2.5% of patients receiving COREG, compared to 0.2% of placebo patients.
To decrease the likelihood of syncope or excessive hypotension, treatment should be initiated with 3.125 mg twice daily for congestive heart failure patients, and at 6.25 mg twice daily for hypertensive patients and survivors of an acute myocardial infarction with left ventricular dysfunction. Dosage should then be increased slowly, according to recommendations in the DOSAGE AND ADMINISTRATION section, and the drug should be taken with food. During initiation of therapy, the patient should be cautioned to avoid situations such as driving or hazardous tasks, where injury could result should syncope occur.
Rarely, use of carvedilol in patients with congestive heart failure has resulted in deterioration of renal function. Patients at risk appear to be those with low blood pressure (systolic blood pressure <100 mm Hg), ischemic heart disease and diffuse vascular disease, and/or underlying renal insufficiency. Renal function has returned to baseline when carvedilol was stopped. In patients with these risk factors it is recommended that renal function be monitored during up-titration of carvedilol and the drug discontinued or dosage reduced if worsening of renal function occurs.
Worsening heart failure or fluid retention may occur during up-titration of carvedilol. If such symptoms occur, diuretics should be increased and the carvedilol dose should not be advanced until clinical stability resumes (see DOSAGE AND ADMINISTRATION ). Occasionally it is necessary to lower the carvedilol dose or temporarily discontinue it. Such episodes do not preclude subsequent successful titration of, or a favorable response to, carvedilol. In a placebo-controlled trial of patients with severe heart failure, worsening heart failure during the first 3 months was reported to a similar degree with carvedilol and with placebo. When treatment was maintained beyond 3 months, worsening heart failure was reported less frequently in patients treated with carvedilol than with placebo. Worsening heart failure observed during long-term therapy is more likely to be related to the patients' underlying disease than to treatment with carvedilol.
In patients with pheochromocytoma, an (alpha)-blocking agent should be initiated prior to the use of any (beta)-blocking agent. Although carvedilol has both (alpha)- and (beta)-blocking pharmacologic activities, there has been no experience with its use in this condition. Therefore, caution should be taken in the administration of carvedilol to patients suspected of having pheochromocytoma.
Agents with non-selective (beta)-blocking activity may provoke chest pain in patients with Prinzmetal's variant angina. There has been no clinical experience with carvedilol in these patients although the (alpha)-blocking activity may prevent such symptoms. However, caution should be taken in the administration of carvedilol to patients suspected of having Prinzmetal's variant angina.
In congestive heart failure patients with diabetes, carvedilol therapy may lead to worsening hyperglycemia, which responds to intensification of hypoglycemic therapy. It is recommended that blood glucose be monitored when carvedilol dosing is initiated, adjusted, or discontinued.
Risk of Anaphylactic Reaction: While taking (beta)-blockers, patients with a history of severe anaphylactic reaction to a variety of allergens may be more reactive to repeated challenge, either accidental, diagnostic, or therapeutic. Such patients may be unresponsive to the usual doses of epinephrine used to treat allergic reaction.
Nonallergic Bronchospasm (e.g., chronic bronchitis and emphysema): Patients with bronchospastic disease should, in general, not receive (beta)-blockers. COREG may be used with caution, however, in patients who do not respond to, or cannot tolerate, other antihypertensive agents. It is prudent, if COREG is used, to use the smallest effective dose, so that inhibition of endogenous or exogenous (beta)-agonists is minimized.
In clinical trials of patients with congestive heart failure, patients with bronchospastic disease were enrolled if they did not require oral or inhaled medication to treat their bronchospastic disease. In such patients, it is recommended that carvedilol be used with caution. The dosing recommendations should be followed closely and the dose should be lowered if any evidence of bronchospasm is observed during up-titration.
Information for Patients: Patients taking COREG should be advised of the following:
- they should not interrupt or discontinue using COREG without a physician's advice.
- congestive heart failure patients should consult their physician if they experience signs or symptoms of worsening heart failure such as weight gain or increasing shortness of breath.
- they may experience a drop in blood pressure when standing, resulting in dizziness and, rarely, fainting. Patients should sit or lie down when these symptoms of lowered blood pressure occur.
- if patients experience dizziness or fatigue, they should avoid driving or hazardous tasks.
- they should consult a physician if they experience dizziness or faintness, in case the dosage should be adjusted.
- they should take COREG with food.
- diabetic patients should report any changes in blood sugar levels to their physician.
- contact lens wearers may experience decreased lacrimation.
Drug Interactions: (Also see CLINICAL PHARMACOLOGY , Pharmacokinetic Drug-Drug Interactions .)
Inhibitors of CYP2D6; poor metabolizers of debrisoquin: Interactions of carvedilol with strong inhibitors of CYP2D6 (such as quinidine, fluoxetine, paroxetine, and propafenone) have not been studied, but these drugs would be expected to increase blood levels of the R(+) enantiomer of carvedilol (see CLINICAL PHARMACOLOGY ). Retrospective analysis of side effects in clinical trials showed that poor 2D6 metabolizers had a higher rate of dizziness during up-titration, presumably resulting from vasodilating effects of the higher concentrations of the (alpha)-blocking R(+) enantiomer.
Catecholamine-depleting agents: Patients taking both agents with (beta)-blocking properties and a drug that can deplete catecholamines (e.g., reserpine and monoamine oxidase inhibitors) should be observed closely for signs of hypotension and/or severe bradycardia.
Clonidine: Concomitant administration of clonidine with agents with (beta)-blocking properties may potentiate blood-pressure- and heart-rate-lowering effects. When concomitant treatment with agents with (beta)-blocking properties and clonidine is to be terminated, the (beta)-blocking agent should be discontinued first. Clonidine therapy can then be discontinued several days later by gradually decreasing the dosage.
Cyclosporine: Modest increases in mean trough cyclosporine concentrations were observed following initiation of carvedilol treatment in 21 renal transplant patients suffering from chronic vascular rejection. In about 30% of patients, the dose of cyclosporine had to be reduced in order to maintain cyclosporine concentrations within the therapeutic range, while in the remainder no adjustment was needed. On the average for the group, the dose of cyclosporine was reduced about 20% in these patients. Due to wide interindividual variability in the dose adjustment required, it is recommended that cyclosporine concentrations be monitored closely after initiation of carvedilol therapy and that the dose of cyclosporine be adjusted as appropriate.
Digoxin: Digoxin concentrations are increased by about 15% when digoxin and carvedilol are administered concomitantly. Both digoxin and COREG slow AV conduction. Therefore, increased monitoring of digoxin is recommended when initiating, adjusting, or discontinuing COREG.
Inducers and inhibitors of hepatic metabolism: Rifampin reduced plasma concentrations of carvedilol by about 70%. Cimetidine increased AUC by about 30% but caused no change in C max .
Calcium channel blockers: Isolated cases of conduction disturbance (rarely with hemodynamic compromise) have been observed when COREG is co-administered with diltiazem. As with other agents with (beta)-blocking properties, if COREG is to be administered orally with calcium channel blockers of the verapamil or diltiazem type, it is recommended that ECG and blood pressure be monitored.
Insulin or oral hypoglycemics: Agents with (beta)-blocking properties may enhance the blood-sugar-reducing effect of insulin and oral hypoglycemics. Therefore, in patients taking insulin or oral hypoglycemics, regular monitoring of blood glucose is recommended.
Carcinogenesis, Mutagenesis, Impairment of Fertility: In 2-year studies conducted in rats given carvedilol at doses up to 75 mg/kg/day (12 times the maximum recommended human dose [MRHD] when compared on a mg/m 2 basis) or in mice given up to 200 mg/kg/day (16 times the MRHD on a mg/m 2 basis), carvedilol had no carcinogenic effect.
Carvedilol was negative when tested in a battery of genotoxicity assays, including the Ames and the CHO/HGPRT assays for mutagenicity and the in vitro hamster micro-nucleus and in vivo human lymphocyte cell tests for clastogenicity.
At doses >/=200 mg/kg/day (>/=32 times the MRHD as mg/m 2 ) carvedilol was toxic to adult rats (sedation, reduced weight gain) and was associated with a reduced number of successful matings, prolonged mating time, significantly fewer corpora lutea and implants per dam, and complete resorption of 18% of the litters. The no-observed-effect dose level for overt toxicity and impairment of fertility was 60 mg/kg/day (10 times the MRHD as mg/m 2 ).
Pregnancy: Teratogenic Effects: Pregnancy Category C. Studies performed in pregnant rats and rabbits given carvedilol revealed increased post-implantation loss in rats at doses of 300 mg/kg/day (50 times the MRHD as mg/m 2 ) and in rabbits at doses of 75 mg/kg/day (25 times the MRHD as mg/m 2 ). In the rats, there was also a decrease in fetal body weight at the maternally toxic dose of 300 mg/kg/day (50 times the MRHD as mg/m 2 ), which was accompanied by an elevation in the frequency of fetuses with delayed skeletal development (missing or stunted 13th rib). In rats the no-observed-effect level for developmental toxicity was 60 mg/kg/day (10 times the MRHD as mg/m 2 ); in rabbits it was 15 mg/kg/day (5 times the MRHD as mg/m 2 ). There are no adequate and well-controlled studies in pregnant women. COREG should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Nursing Mothers: It is not known whether this drug is excreted in human milk. Studies in rats have shown that carvedilol and/or its metabolites (as well as other (beta)-blockers) cross the placental barrier and are excreted in breast milk. There was increased mortality at one week post-partum in neonates from rats treated with 60 mg/kg/day (10 times the MRHD as mg/m 2 ) and above during the last trimester through day 22 of lactation. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from (beta)-blockers, especially bradycardia, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother. The effects of other (alpha)- and (beta)-blocking agents have included perinatal and neonatal distress.
Pediatric Use: Safety and efficacy in patients younger than 18 years of age have not been established.
Geriatric Use: Of the 765 patients with congestive heart failure randomized to COREG in US clinical trials, 31% (235) were 65 years of age or older, and 7.3% (56) were 75 years of age or older. Of the 1,156 patients randomized to COREG in a long-term, placebo-controlled trial in severe heart failure, 47% (547) were 65 years of age or older, and 15% (174) were 75 years of age or older. Of 3,025 patients receiving COREG in congestive heart failure trials worldwide, 42% were 65 years of age or older.
Of the 975 myocardial infarction patients randomized to COREG in the CAPRICORN trial, 48% (468) were 65 years of age or older, and 11% (111) were 75 years of age or older.
Of the 2,065 hypertensive patients in US clinical trials of efficacy or safety who were treated with COREG, 21% (436) were 65 years of age or older. Of 3,722 patients receiving COREG in hypertension clinical trials conducted worldwide, 24% were 65 years of age or older.
With the exception of dizziness in hypertensive patients (incidence 8.8% in the elderly vs. 6% in younger patients), no overall differences in the safety or effectiveness (See Figures 2 and 4.) were observed between the older subjects and younger subjects in each of these populations. Similarly, other reported clinical experience has not identified differences in responses between the elderly and younger subjects, but greater sensitivity of some older individuals cannot be ruled out.
ADVERSE REACTIONS
COREG has been evaluated for safety in patients with congestive heart failure (mild, moderate, and severe heart failure), in patients with left ventricular dysfunction following myocardial infarction and in hypertensive patients. The observed adverse event profile was consistent with the pharmacology of the drug and the health status of the patients in the clinical trials. Adverse events reported for each of these patient populations are provided below. Excluded are adverse events considered too general to be informative, and those not reasonably associated with the use of the drug because they were associated with the condition being treated or are very common in the treated population. Rates of adverse events were generally similar across demographic subsets (men and women, elderly and non-elderly, blacks and non-blacks).
Congestive Heart Failure: COREG has been evaluated for safety in congestive heart failure in more than 4,500 patients worldwide of whom more than 2,100 participated in placebo-controlled clinical trials. Approximately 60% of the total treated population in placebo-controlled clinical trials received COREG for at least 6 months and 30% received COREG for at least 12 months. In the COMET trial, 1,511 patients with mild-to-moderate heart failure were treated with COREG for up to 5.9 years (mean 4.8 years). Both in US clinical trials in mild-to-moderate heart failure that compared COREG in daily doses up to 100 mg (n = 765) to placebo (n = 437), and in a multinational clinical trial in severe heart failure (COPERNICUS) that compared COREG in daily doses up to 50 mg (n = 1,156) with placebo (n = 1,133), discontinuation rates for adverse experiences were similar in carvedilol and placebo patients. In placebo-controlled clinical trials, the only cause of discontinuation >1%, and occurring more often on carvedilol was dizziness (1.3% on carvedilol, 0.6% on placebo in the COPERNICUS trial).
Table 2 shows adverse events reported in patients with mild-to-moderate heart failure enrolled in US placebo-controlled clinical trials, and with severe heart failure enrolled in the COPERNICUS trial. Shown are adverse events that occurred more frequently in drug-treated patients than placebo-treated patients with an incidence of >3% in patients treated with carvedilol regardless of causality. Median study medication exposure was 6.3 months for both carvedilol and placebo patients in the trials of mild-to-moderate heart failure, and 10.4 months in the trial of severe heart failure patients. The adverse event profile of COREG observed in the long-term COMET study was generally similar to that observed in the US Heart Failure Trials.
Table 2. Adverse Events (% Occurrence) Occurring More Frequently With COREG Than With Placebo in Patients With Mild-to-Moderate Heart Failure Enrolled in US Heart Failure Trials or in Patients With Severe Heart Failure in the COPERNICUS Trial (Incidence >3% in Patients Treated with Carvedilol, Regardless of Causality) Mild-to-Moderate HF Severe Heart Failure COREG Placebo COREG Placebo (n = 765) (n = 437) (n = 1,156) (n = 1,133) Body as a Whole Asthenia 7 7 11 9 Fatigue 24 22 -- -- Digoxin level increased 5 4 2 1 Edema generalized 5 3 6 5 Edema dependent 4 2 -- -- Cardiovascular Bradycardia 9 1 10 3 Hypotension 9 3 14 8 Syncope 3 3 8 5 Angina Pectoris 2 3 6 4 Central Nervous System Dizziness 32 19 24 17 Headache 8 7 5 3 Gastrointestinal Diarrhea 12 6 5 3 Nausea 9 5 4 3 Vomiting 6 4 1 2 Metabolic Hyperglycemia 12 8 5 3 Weight increase 10 7 12 11 BUN increased 6 5 -- -- NPN increased 6 5 -- -- Hypercholesterolemia 4 3 1 1 Edema peripheral 2 1 7 6 Musculoskeletal Arthralgia 6 5 1 1 Respiratory Cough Increased 8 9 5 4 Rales 4 4 4 2 Vision Vision abnormal 5 2 -- -- Cardiac failure and dyspnea were also reported in these studies, but the rates were equal or greater in patients who received placebo.
The following adverse events were reported with a frequency of >1% but </=3% and more frequently with COREG in either the US placebo-controlled trials in patients with mild-to-moderate heart failure, or in patients with severe heart failure in the COPERNICUS trial.
Incidence >1% to </=3%
Body as a Whole: Allergy, malaise, hypovolemia, fever, leg edema.
Cardiovascular: Fluid overload, postural hypotension, aggravated angina pectoris, AV block, palpitation, hypertension.
Central and Peripheral Nervous System: Hypesthesia, vertigo, paresthesia.
Gastrointestinal: Melena, periodontitis.
Liver and Biliary System: SGPT increased, SGOT increased.
Metabolic and Nutritional: Hyperuricemia, hypoglycemia, hyponatremia, increased alkaline phosphatase, glycosuria, hypervolemia, diabetes mellitus, GGT increased, weight loss, hyperkalemia, creatinine increased.
Musculoskeletal: Muscle cramps.
Platelet, Bleeding and Clotting: Prothrombin decreased, purpura, thrombocytopenia.
Psychiatric: Somnolence.
Reproductive, male: Impotence.
Special Senses: Blurred vision.
Urinary System: Renal insufficiency, albuminuria, hematuria.
Left Ventricular Dysfunction Following Myocardial Infarction: COREG has been evaluated for safety in survivors of an acute myocardial infarction with left ventricular dysfunction in the CAPRICORN trial which involved 969 patients who received COREG and 980 who received placebo. Approximately 75% of the patients received COREG for at least 6 months and 53% received COREG for at least 12 months. Patients were treated for an average of 12.9 months and 12.8 months with COREG and placebo, respectively.
The most common adverse events reported with COREG in the CAPRICORN trial were consistent with the profile of the drug in the US heart failure trials and the COPERNICUS trial. The only additional adverse events reported in CAPRICORN in >3% of the patients and more commonly on carvedilol were dyspnea, anemia, and lung edema. The following adverse events were reported with a frequency of >1% but </=3% and more frequently with COREG: flu syndrome, cerebrovascular accident, peripheral vascular disorder, hypotonia, depression, gastrointestinal pain, arthritis and gout. The overall rates of discontinuations due to adverse events were similar in both groups of patients. In this database, the only cause of discontinuation >1%, and occurring more often on carvedilol was hypotension (1.5% on carvedilol, 0.2% on placebo).
Hypertension: COREG has been evaluated for safety in hypertension in more than 2,193 patients in US clinical trials and in 2,976 patients in international clinical trials. Approximately 36% of the total treated population received COREG for at least 6 months. In general, COREG was well tolerated at doses up to 50 mg daily. Most adverse events reported during COREG therapy were of mild to moderate severity. In US controlled clinical trials directly comparing COREG monotherapy in doses up to 50 mg (n = 1,142) to placebo (n = 462), 4.9% of COREG patients discontinued for adverse events vs. 5.2% of placebo patients. Although there was no overall difference in discontinuation rates, discontinuations were more common in the carvedilol group for postural hypotension (1% vs. 0). The overall incidence of adverse events in US placebo-controlled trials was found to increase with increasing dose of COREG. For individual adverse events this could only be distinguished for dizziness, which increased in frequency from 2% to 5% as total daily dose increased from 6.25 mg to 50 mg.
Table 3 shows adverse events in US placebo-controlled clinical trials for hypertension that occurred with an incidence of >1% regardless of causality, and that were more frequent in drug-treated patients than placebo-treated patients.
Table 3. Adverse Events in US Placebo-Controlled Hypertension Trials Incidence >/=1%, Regardless of Causality * Adverse Reactions COREG
(n = 1,142)
% occurrencePlacebo
(n = 462)
% occurrenceCardiovascular Bradycardia 2 -- Postural hypotension 2 -- Peripheral Edema 1 -- Central Nervous System Dizziness 6 5 Insomnia 2 1 Gastrointestinal Diarrhea 2 1 Hematologic Thrombocytopenia 1 -- Metabolic Hypertriglyceridemia 1 -- *Shown are events with rate >1% rounded to nearest integer. Dyspnea and fatigue were also reported in these studies, but the rates were equal or greater in patients who received placebo.
The following adverse events not described above were reported as possibly or probably related to COREG in worldwide open or controlled trials with COREG in patients with hypertension or congestive heart failure.
Incidence >0.1% to </=1%
Cardiovascular: Peripheral ischemia, tachycardia.
Central and Peripheral Nervous System: Hypokinesia.
Gastrointestinal: Bilirubinemia, increased hepatic enzymes (0.2% of hypertension patients and 0.4% of congestive heart failure patients were discontinued from therapy because of increases in hepatic enzymes; see Laboratory Abnormalities .
Psychiatric: Nervousness, sleep disorder, aggravated depression, impaired concentration, abnormal thinking, paroniria, emotional lability.
Respiratory System: Asthma (see CONTRAINDICATIONS).
Reproductive: Male: decreased libido.
Skin and Appendages: Pruritus, rash erythematous, rash maculopapular, rash psoriaform, photosensitivity reaction.
Special Senses: Tinnitus.
Urinary System: Micturition frequency increased.
Autonomic Nervous System: Dry mouth, sweating increased.
Metabolic and Nutritional: Hypokalemia, hypertriglyceridemia.
Hematologic: Anemia, leukopenia.
The following events were reported in </=0.1% of patients and are potentially important: complete AV block, bundle branch block, myocardial ischemia, cerebrovascular disorder, convulsions, migraine, neuralgia, paresis, anaphylactoid reaction, alopecia, exfoliative dermatitis, amnesia, GI hemorrhage, bronchospasm, pulmonary edema, decreased hearing, respiratory alkalosis, increased BUN, decreased HDL, pancytopenia, and atypical lymphocytes.
Laboratory Abnormalities: Reversible elevations in serum transaminases (ALT or AST) have been observed during treatment with COREG. Rates of transaminase elevations (2- to 3-times the upper limit of normal) observed during controlled clinical trials have generally been similar between patients treated with COREG and those treated with placebo. However, transaminase elevations, confirmed by rechallenge, have been observed with COREG. In a long-term, placebo-controlled trial in severe heart failure, patients treated with COREG had lower values for hepatic transaminases than patients treated with placebo, possibly because COREG-induced improvements in cardiac function led to less hepatic congestion and/or improved hepatic blood flow.
COREG therapy has not been associated with clinically significant changes in serum potassium, total triglycerides, total cholesterol, HDL cholesterol, uric acid, blood urea nitrogen, or creatinine. No clinically relevant changes were noted in fasting serum glucose in hypertensive patients; fasting serum glucose was not evaluated in the congestive heart failure clinical trials.
Postmarketing Experience: Reports of aplastic anemia and severe skin reactions (Stevens-Johnson syndrome, toxic epidermal necrolysis, and erythema multiforme) have been rare and received only when carvedilol was administered concomitantly with other medications associated with such reactions. Urinary incontinence in women (which resolved upon discontinuation of the medication) and interstitial pneumonitis have been reported rarely.
OVERDOSAGE
The acute oral LD50 doses in male and female mice and male and female rats are over 8000 mg/kg. Overdosage may cause severe hypotension, bradycardia, cardiac insufficiency, cardiogenic shock, and cardiac arrest. Respiratory problems, bronchospasms, vomiting, lapses of consciousness, and generalized seizures may also occur.
The patient should be placed in a supine position and, where necessary, kept under observation and treated under intensive-care conditions. Gastric lavage or pharmacologically induced emesis may be used shortly after ingestion. The following agents may be administered:
for excessive bradycardia: atropine, 2 mg IV.
to support cardiovascular function: glucagon, 5 to 10 mg IV rapidly over 30 seconds, followed by a continuous infusion of 5 mg/hour; sympathomimetics (dobutamine, isoprenaline, adrenaline) at doses according to body weight and effect.
If peripheral vasodilation dominates, it may be necessary to administer adrenaline or noradrenaline with continuous monitoring of circulatory conditions. For therapy-resistant bradycardia, pacemaker therapy should be performed. For bronchospasm, (beta)-sympathomimetics (as aerosol or IV) or aminophylline IV should be given. In the event of seizures, slow IV injection of diazepam or clonazepam is recommended.
NOTE: In the event of severe intoxication where there are symptoms of shock, treatment with antidotes must be continued for a sufficiently long period of time consistent with the 7- to 10-hour half-life of carvedilol.
Cases of overdosage with COREG alone or in combination with other drugs have been reported. Quantities ingested in some cases exceeded 1,000 milligrams. Symptoms experienced included low blood pressure and heart rate. Standard supportive treatment was provided and individuals recovered.
DOSAGE AND ADMINISTRATION
Congestive Heart Failure: DOSAGE MUST BE INDIVIDUALIZED AND CLOSELY MONITORED BY A PHYSICIAN DURING UP-TITRATION. Prior to initiation of COREG, it is recommended that fluid retention be minimized. The recommended starting dose of COREG is 3.125 mg, twice daily for 2 weeks. Patients who tolerate a dose of 3.125 mg twice daily may have their dose increased to 6.25, 12.5, and 25 mg twice daily over successive intervals of at least 2 weeks. Patients should be maintained on lower doses if higher doses are not tolerated. A maximum dose of 50 mg twice daily has been administered to patients with mild-to-moderate heart failure weighing over 85 kg (187 lbs).
Patients should be advised that initiation of treatment and (to a lesser extent) dosage increases may be associated with transient symptoms of dizziness or lightheadedness (and rarely syncope) within the first hour after dosing. Thus during these periods they should avoid situations such as driving or hazardous tasks, where symptoms could result in injury. In addition, COREG should be taken with food to slow the rate of absorption. Vasodilatory symptoms often do not require treatment, but it may be useful to separate the time of dosing of COREG from that of the ACE inhibitor or to reduce temporarily the dose of the ACE inhibitor. The dose of COREG should not be increased until symptoms of worsening heart failure or vasodilation have been stabilized.
Fluid retention (with or without transient worsening heart failure symptoms) should be treated by an increase in the dose of diuretics.
The dose of COREG should be reduced if patients experience bradycardia (heart rate <55 beats/minute).
Episodes of dizziness or fluid retention during initiation of COREG can generally be managed without discontinuation of treatment and do not preclude subsequent successful titration of, or a favorable response to, carvedilol.
Left Ventricular Dysfunction Following Myocardial Infarction: DOSAGE MUST BE INDIVIDUALIZED AND MONITORED DURING UP-TITRATION. Treatment with COREG may be started as an inpatient or outpatient and should be started after the patient is hemodynamically stable and fluid retention has been minimized. It is recommended that COREG be started at 6.25 mg twice daily and increased after 3 to 10 days, based on tolerability to 12.5 mg twice daily, then again to the target dose of 25 mg twice daily. A lower starting dose may be used (3.125 mg twice daily) and/or, the rate of up-titration may be slowed if clinically indicated (e.g., due to low blood pressure or heart rate, or fluid retention). Patients should be maintained on lower doses if higher doses are not tolerated. The recommended dosing regimen need not be altered in patients who received treatment with an IV or oral (beta)-blocker during the acute phase of the myocardial infarction.
Hypertension: DOSAGE MUST BE INDIVIDUALIZED. The recommended starting dose of COREG is 6.25 mg twice daily. If this dose is tolerated, using standing systolic pressure measured about 1 hour after dosing as a guide, the dose should be maintained for 7 to 14 days, and then increased to 12.5 mg twice daily if needed, based on trough blood pressure, again using standing systolic pressure one hour after dosing as a guide for tolerance. This dose should also be maintained for 7 to 14 days and can then be adjusted upward to 25 mg twice daily if tolerated and needed. The full antihypertensive effect of COREG is seen within 7 to 14 days. Total daily dose should not exceed 50 mg. COREG should be taken with food to slow the rate of absorption and reduce the incidence of orthostatic effects.
Addition of a diuretic to COREG, or COREG to a diuretic can be expected to produce additive effects and exaggerate the orthostatic component of COREG action.
Use in Patients with Hepatic Impairment: COREG should not be given to patients with severe hepatic impairment (see CONTRAINDICATIONS ).
HOW SUPPLIED
Tablets: White, oval, film-coated tablets: 3.125 mg-engraved with 39 and SB, in bottles of 100; 6.25 mg-engraved with 4140 and SB, in bottles of 100; 12.5 mg-engraved with 4141 and SB, in bottles of 100; 25 mg-engraved with 4142 and SB, in bottles of 100. The 6.25 mg, 12.5 mg, and 25 mg tablets are TILTAB tablets.
Store below 30°C (86°F). Protect from moisture. Dispense in a tight, light-resistant container.
3.125 mg 100's: 0007-4139-20
6.25 mg 100's: NDC 0007-4140-20
12.5 mg 100's: NDC 0007-4141-20
25 mg 100's: NDC 0007-4142-20
COREG and TILTAB are registered trademarks of Glaxosmithkline.
Research Triangle Park, NC 27709
©2005 Glaxosmithkline. All rights reserved.
June 2005 CO:L10
Subscribe to the "News" RSS Feed 
TOP ۞
