-
Inderal LA Long-Acting Capsules (Wyeth)
This product's label may have been revised after this insert was used in production. For further product information and current package insert, please visit www.wyeth.com or call our medical communications department toll-free at 1-800-934-5556.
DESCRIPTION
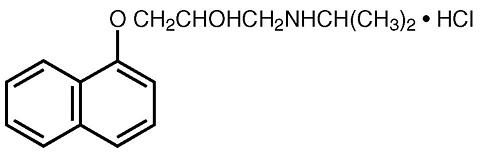
Inderal (propranolol hydrochloride) is a synthetic beta-adrenergic receptor-blocking agent chemically described as 2-Propanol, 1-[(1-methylethyl)amino]-3-(1-naphthalenyloxy)-, hydrochloride. Its structural formula is:
Propranolol hydrochloride is a stable, white, crystalline solid which is readily soluble in water and ethanol. Its molecular weight is 295.80.
Inderal LA is formulated to provide a sustained release of propranolol hydrochloride. Inderal LA is available as 60 mg, 80 mg, 120 mg, and 160 mg capsules.
Inderal LA capsules contain the following inactive ingredients: cellulose, ethylcellulose, gelatin capsules, hypromellose, and titanium dioxide. In addition, Inderal LA 60 mg, 80 mg, and 120 mg capsules contain D&C Red No. 28 and FD&C Blue No. 1; Inderal LA 160 mg capsules contain FD&C Blue No. 1.
These capsules comply with USP Drug Release Test 1.
CLINICAL PHARMACOLOGY
Inderal is a nonselective, beta-adrenergic receptor-blocking agent possessing no other autonomic nervous system activity. It specifically competes with beta-adrenergic receptor-stimulating agents for available receptor sites. When access to beta-receptor sites is blocked by Inderal, the chronotropic, inotropic, and vasodilator responses to beta-adrenergic stimulation are decreased proportionately.
Inderal LA Capsules (60, 80, 120, and 160 mg) release propranolol HCl at a controlled and predictable rate. Peak blood levels following dosing with Inderal LA occur at about 6 hours, and the apparent plasma half-life is about 10 hours. When measured at steady state over a 24-hour period the areas under the propranolol plasma concentration-time curve (AUCs) for the capsules are approximately 60% to 65% of the AUCs for a comparable divided daily dose of Inderal Tablets. The lower AUCs for the capsules are due to greater hepatic metabolism of propranolol, resulting from the slower rate of absorption of propranolol. Over a twenty-four (24) hour period, blood levels are fairly constant for about twelve (12) hours, then decline exponentially.
Inderal LA should not be considered a simple mg-for-mg substitute for conventional propranolol and the blood levels achieved do not match (are lower than) those of two to four times daily dosing with the same dose. When changing to Inderal LA from conventional propranolol, a possible need for retitration upwards should be considered, especially to maintain effectiveness at the end of the dosing interval. In most clinical settings, however, such as hypertension or angina where there is little correlation between plasma levels and clinical effect, Inderal LA has been therapeutically equivalent to the same mg dose of conventional Inderal as assessed by 24-hour effects on blood pressure and on 24-hour exercise responses of heart rate, systolic pressure, and rate pressure product. Inderal LA can provide effective beta blockade for a 24-hour period.
The mechanism of the antihypertensive effect of Inderal has not been established. Among the factors that may be involved in contributing to the antihypertensive action are: (1) decreased cardiac output, (2) inhibition of renin release by the kidneys, and (3) diminution of tonic sympathetic nerve outflow from vasomotor centers in the brain. Although total peripheral resistance may increase initially, it readjusts to or below the pretreatment level with chronic use. Effects on plasma volume appear to be minor and somewhat variable. Inderal has been shown to cause a small increase in serum potassium concentration when used in the treatment of hypertensive patients.
In angina pectoris, propranolol generally reduces the oxygen requirement of the heart at any given level of effort by blocking the catecholamine-induced increases in the heart rate, systolic blood pressure, and the velocity and extent of myocardial contraction. Propranolol may increase oxygen requirements by increasing left ventricular fiber length, end diastolic pressure, and systolic ejection period. The net physiologic effect of beta-adrenergic blockade is usually advantageous and is manifested during exercise by delayed onset of pain and increased work capacity.
In dosages greater than required for beta blockade, Inderal also exerts a quinidine-like or anesthetic-like membrane action which affects the cardiac action potential. The significance of the membrane action in the treatment of arrhythmias is uncertain.
The mechanism of the antimigraine effect of propranolol has not been established. Beta-adrenergic receptors have been demonstrated in the pial vessels of the brain.
Beta-receptor blockade can be useful in conditions in which, because of pathologic or functional changes, sympathetic activity is detrimental to the patient. But there are also situations in which sympathetic stimulation is vital. For example, in patients with severely damaged hearts, adequate ventricular function is maintained by virtue of sympathetic drive, which should be preserved. In the presence of AV block, greater than first degree, beta blockade may prevent the necessary facilitating effect of sympathetic activity on conduction. Beta blockade results in bronchial constriction by interfering with adrenergic bronchodilator activity, which should be preserved in patients subject to bronchospasm.
Propranolol is not significantly dialyzable.
INDICATIONS AND USAGE
Hypertension
Inderal LA is indicated in the management of hypertension; it may be used alone or used in combination with other antihypertensive agents, particularly a thiazide diuretic. Inderal LA is not indicated in the management of hypertensive emergencies.
Angina Pectoris Due to Coronary Atherosclerosis
Inderal LA is indicated for the long-term management of patients with angina pectoris.
Migraine
Inderal LA is indicated for the prophylaxis of common migraine headache. The efficacy of propranolol in the treatment of a migraine attack that has started has not been established, and propranolol is not indicated for such use.
Hypertrophic Subaortic Stenosis
Inderal LA is useful in the management of hypertrophic subaortic stenosis, especially for treatment of exertional or other stress-induced angina, palpitations, and syncope. Inderal LA also improves exercise performance. The effectiveness of propranolol hydrochloride in this disease appears to be due to a reduction of the elevated outflow pressure gradient, which is exacerbated by beta-receptor stimulation. Clinical improvement may be temporary.
CONTRAINDICATIONS
Inderal is contraindicated in 1) cardiogenic shock; 2) sinus bradycardia and greater than first-degree block; 3) bronchial asthma; 4) congestive heart failure (see " WARNINGS "), unless the failure is secondary to a tachyarrhythmia treatable with Inderal.
WARNINGS
Hypersensitivity reactions, including anaphylactic/anaphylactoid reactions, have been associated with the administration of propranolol (see " ADVERSE REACTIONS ").
Cardiac Failure: Sympathetic stimulation may be a vital component supporting circulatory function in patients with congestive heart failure, and its inhibition by beta blockade may precipitate more severe failure. Although beta blockers should be avoided in overt congestive heart failure, if necessary, they can be used with close follow-up in patients with a history of failure who are well compensated and are receiving digitalis and diuretics. Beta-adrenergic blocking agents do not abolish the inotropic action of digitalis on heart muscle.
In Patients without a History of Heart Failure, continued use of beta blockers can, in some cases, lead to cardiac failure. Therefore, at the first sign or symptom of heart failure, the patient should be digitalized and/or treated with diuretics, and the response observed closely, or Inderal should be discontinued (gradually, if possible).
In Patients with Angina Pectoris, there have been reports of exacerbation of angina and, in some cases, myocardial infarction, following abrupt discontinuance of Inderal therapy. Therefore, when discontinuance of Inderal is planned, the dosage should be gradually reduced over at least a few weeks, and the patient should be cautioned against interruption or cessation of therapy without the physician's advice. If Inderal therapy is interrupted and exacerbation of angina occurs, it usually is advisable to reinstitute Inderal therapy and take other measures appropriate for the management of unstable angina pectoris. Since coronary artery disease may be unrecognized, it may be prudent to follow the above advice in patients considered at risk of having occult atherosclerotic heart disease who are given propranolol for other indications. Nonallergic Bronchospasm (e.g., Chronic Bronchitis, Emphysema) --PATIENTS WITH BRONCHOSPASTIC DISEASES SHOULD IN GENERAL NOT RECEIVE BETA BLOCKERS. Inderal should be administered with caution since it may block bronchodilation produced by endogenous and exogenous catecholamine stimulation of beta receptors.
Major Surgery: The necessity or desirability of withdrawal of beta-blocking therapy prior to major surgery is controversial. It should be noted, however, that the impaired ability of the heart to respond to reflex adrenergic stimuli may augment the risks of general anesthesia and surgical procedures.
Inderal, like other beta blockers, is a competitive inhibitor of beta-receptor agonists and its effects can be reversed by administration of such agents, e.g., dobutamine or isoproterenol. However, such patients may be subject to protracted severe hypotension. Difficulty in starting and maintaining the heartbeat has also been reported with beta blockers.
Diabetes and Hypoglycemia: Beta-adrenergic blockade may prevent the appearance of certain premonitory signs and symptoms (pulse rate and pressure changes) of acute hypoglycemia in labile insulin-dependent diabetes. In these patients, it may be more difficult to adjust the dosage of insulin. Hypoglycemic attacks may be accompanied by a precipitous elevation of blood pressure in patients on propranolol.
Propranolol therapy, particularly in infants and children, diabetic or not, has been associated with hypoglycemia especially during fasting as in preparation for surgery. Hypoglycemia also has been found after this type of drug therapy and prolonged physical exertion and has occurred in renal insufficiency, both during dialysis and sporadically, in patients on propranolol.
Acute increases in blood pressure have occurred after insulin-induced hypoglycemia in patients on propranolol.
Thyrotoxicosis: Beta blockade may mask certain clinical signs of hyperthyroidism. Therefore, abrupt withdrawal of propranolol may be followed by an exacerbation of symptoms of hyperthyroidism, including thyroid storm. Propranolol may change thyroid-function tests, increasing T 4 and reverse T 3 , and decreasing T 3 .
In Patients with Wolff-Parkinson-White Syndrome, several cases have been reported in which, after propranolol, the tachycardia was replaced by a severe bradycardia requiring a demand pacemaker. In one case this resulted after an initial dose of 5 mg propranolol.
Skin Reactions: Cutaneous reactions, including Stevens-Johnson Syndrome, toxic epidermal necrolysis, exfoliative dermatitis, erythema multiforme, and urticaria, have been reported with use of propranolol (see " ADVERSE REACTIONS ").
PRECAUTIONS
General
Propranolol should be used with caution in patients with impaired hepatic or renal function. Inderal is not indicated for the treatment of hypertensive emergencies.
Beta-adrenoreceptor blockade can cause reduction of intraocular pressure. Patients should be told that Inderal may interfere with the glaucoma screening test. Withdrawal may lead to a return of increased intraocular pressure.
Risk of anaphylactic reaction. While taking beta blockers, patients with a history of severe anaphylactic reaction to a variety of allergens may be more reactive to repeated challenge, either accidental, diagnostic, or therapeutic. Such patients may be unresponsive to the usual doses of epinephrine used to treat allergic reaction.
Clinical Laboratory Tests
Elevated blood urea levels in patients with severe heart disease, elevated serum transaminase, alkaline phosphatase, lactate dehydrogenase.
Drug Interactions
Patients receiving catecholamine-depleting drugs such as reserpine should be closely observed if Inderal is administered. The added catecholamine-blocking action may produce an excessive reduction of resting sympathetic nervous activity which may result in hypotension, marked bradycardia, vertigo, syncopal attacks, or orthostatic hypotension.
Caution should be exercised when patients receiving a beta blocker are administered a calcium-channel-blocking drug, especially intravenous verapamil, for both agents may depress myocardial contractility or atrioventricular conduction. On rare occasions, the concomitant intravenous use of a beta blocker and verapamil has resulted in serious adverse reactions, especially in patients with severe cardiomyopathy, congestive heart failure or recent myocardial infarction.
Blunting of the antihypertensive effect of beta-adrenoceptor blocking agents by nonsteroidal anti-inflammatory drugs has been reported.
Hypotension and cardiac arrest have been reported with the concomitant use of propranolol and haloperidol.
Aluminum hydroxide gel greatly reduces intestinal absorption of propranolol.
Ethanol slows the rate of absorption of propranolol.
Phenytoin, phenobarbitone, and rifampin accelerate propranolol clearance.
Chlorpromazine, when used concomitantly with propranolol, results in increased plasma levels of both drugs.
Antipyrine and lidocaine have reduced clearance when used concomitantly with propranolol.
Thyroxine may result in a lower than expected T 3 concentration when used concomitantly with propranolol.
Cimetidine decreases the hepatic metabolism of propranolol, delaying elimination and increasing blood levels.
Theophylline clearance is reduced when used concomitantly with propranolol.
Carcinogenesis, Mutagenesis, Impairment of Fertility
In dietary administration studies in which mice and rats were treated with propranolol for up to 18 months at doses of up to 150 mg/kg/day, there was no evidence of drug-related tumorigenesis. In a study in which both male and female rats were exposed to propranolol in their diets at concentrations of up to 0.05%, from 60 days prior to mating and throughout pregnancy and lactation for two generations, there were no effects on fertility. Based on differing results from Ames Tests performed by different laboratories, there is equivocal evidence for a genotoxic effect of propranolol in bacteria ( S. typhimurium strain TA 1538).
Pregnancy: Pregnancy Category C
In a series of reproductive and developmental toxicology studies, propranolol was given to rats by gavage or in the diet throughout pregnancy and lactation. At doses of 150 mg/kg/day (> 10 times the maximum recommended human daily dose of propranolol on a body weight basis), but not at doses of 80 mg/kg/day, treatment was associated with embryotoxicity (reduced litter size and increased resorption sites) as well as neonatal toxicity (deaths). Propranolol also was administered (in the feed) to rabbits (throughout pregnancy and lactation) at doses as high as 150 mg/kg/day (> 15 times the maximum recommended daily human dose). No evidence of embryo or neonatal toxicity was noted.
There are no adequate and well-controlled studies in pregnant women. Intrauterine growth retardation has been reported in neonates whose mothers received propranolol during pregnancy. Neonates whose mothers are receiving propranolol at parturition have exhibited bradycardia, hypoglycemia and respiratory depression. Adequate facilities for monitoring these infants at birth should be available. Inderal should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Nursing Mothers
Inderal is excreted in human milk. Caution should be exercised when Inderal is administered to a nursing woman.
Pediatric Use
Safety and effectiveness in pediatric patients have not been established.
Geriatric Use
Clinical studies of propranolol did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of the decreased hepatic, renal or cardiac function, and of concomitant disease or other drug therapy.
ADVERSE REACTIONS
Most adverse effects have been mild and transient and have rarely required the withdrawal of therapy.
Cardiovascular: Bradycardia; congestive heart failure; intensification of AV block; hypotension; paresthesia of hands; thrombocytopenic purpura; arterial insufficiency, usually of the Raynaud type.
Central Nervous System: Light-headedness; mental depression manifested by insomnia, lassitude, weakness, fatigue; reversible mental depression progressing to catatonia; visual disturbances; hallucinations; vivid dreams; an acute reversible syndrome characterized by disorientation for time and place, short-term memory loss, emotional lability, slightly clouded sensorium, and decreased performance on neuropsychometrics. For immediate formulations, fatigue, lethargy, and vivid dreams appear dose related.
Gastrointestinal: Nausea, vomiting, epigastric distress, abdominal cramping, diarrhea, constipation, mesenteric arterial thrombosis, and ischemic colitis.
Allergic: Hypersensitivity reactions, including anaphylactic/anaphylactoid reactions, pharyngitis and agranulocytosis, erythematous rash, fever combined with aching and sore throat, laryngospasm, and respiratory distress.
Respiratory: Bronchospasm.
Hematologic: Agranulocytosis, nonthrombocytopenic purpura, and thrombocytopenic purpura.
Autoimmune: In extremely rare instances, systemic lupus erythematosus has been reported.
Miscellaneous: Alopecia, LE-like reactions, psoriasiform rashes, dry eyes, male impotence, and Peyronie's disease have been reported rarely. Oculomucocutaneous reactions involving the skin, serous membranes, and conjunctivae reported for a beta blocker (practolol) have not been associated with propranolol.
Skin: Stevens-Johnson Syndrome, toxic epidermal necrolysis, exfoliative dermatitis, erythema multiforme, and urticaria.
DOSAGE AND ADMINISTRATION
Inderal ® LA provides propranolol hydrochloride in a sustained-release capsule for administration once daily. If patients are switched from Inderal Tablets to Inderal LA Capsules, care should be taken to assure that the desired therapeutic effect is maintained. Inderal LA should not be considered a simple mg-for-mg substitute for Inderal. Inderal LA has different kinetics and produces lower blood levels. Retitration may be necessary, especially to maintain effectiveness at the end of the 24-hour dosing interval.
Hypertension
Dosage must be individualized. The usual initial dosage is 80 mg Inderal LA once daily, whether used alone or added to a diuretic. The dosage may be increased to 120 mg once daily or higher until adequate blood pressure control is achieved. The usual maintenance dosage is 120 to 160 mg once daily. In some instances a dosage of 640 mg may be required. The time needed for full hypertensive response to a given dosage is variable and may range from a few days to several weeks.
Angina Pectoris
Dosage must be individualized. Starting with 80 mg Inderal LA once daily, dosage should be gradually increased at three- to seven-day intervals until optimal response is obtained. Although individual patients may respond at any dosage level, the average optimal dosage appears to be 160 mg once daily. In angina pectoris, the value and safety of dosage exceeding 320 mg per day have not been established.
If treatment is to be discontinued, reduce dosage gradually over a period of a few weeks (see " WARNINGS ").
Migraine
Dosage must be individualized. The initial oral dose is 80 mg Inderal LA once daily. The usual effective dose range is 160 to 240 mg once daily. The dosage may be increased gradually to achieve optimal migraine prophylaxis. If a satisfactory response is not obtained within four to six weeks after reaching the maximal dose, Inderal LA therapy should be discontinued. It may be advisable to withdraw the drug gradually over a period of several weeks.
Hypertrophic Subaortic Stenosis
80 to 160 mg Inderal LA once daily.
Pediatric Dosage
At this time the data on the use of the drug in this age group are too limited to permit adequate directions for use.
OVERDOSAGE
Inderal is not significantly dialyzable. In the event of overdosage or exaggerated response, the following measures should be employed:
General
If ingestion is, or may have been, recent, evacuate gastric contents, taking care to prevent pulmonary aspiration.
Bradycardia
ADMINISTER ATROPINE (0.25 to 1.0 mg); IF THERE IS NO RESPONSE TO VAGAL BLOCKADE, ADMINISTER ISOPROTERENOL CAUTIOUSLY.
Cardiac Failure
DIGITALIZATION AND DIURETICS.
Hypotension
VASOPRESSORS, e.g., LEVARTERENOL OR EPINEPHRINE (THERE IS EVIDENCE THAT EPINEPHRINE IS THE DRUG OF CHOICE).
Bronchospasm
ADMINISTER ISOPROTERENOL AND AMINOPHYLLINE.
HOW SUPPLIED
Inderal ® LA Capsules (propranolol hydrochloride)
Each white/light-blue capsule, identified by 3 narrow bands, 1 wide band, and "INDERAL LA 60," contains 60 mg of propranolol hydrochloride in bottles of 100 (NDC 0046-0470-81).
Each light-blue capsule, identified by 3 narrow bands, 1 wide band, and "INDERAL LA 80," contains 80 mg of propranolol hydrochloride in bottles of 100 (NDC 0046-0471-81).
Each light-blue/dark-blue capsule, identified by 3 narrow bands, 1 wide band, and "INDERAL LA 120," contains 120 mg of propranolol hydrochloride in bottles of 100 (NDC 0046-0473-81).
Each dark-blue capsule, identified by 3 narrow bands, 1 wide band, and "INDERAL LA 160," contains 160 mg of propranolol hydrochloride in bottles of 100 (NDC 0046-0479-81).
The appearance of these capsules is a registered trademark of Wyeth Pharmaceuticals.
Store at 20° to 25°C (68° to 77°F); excursions permitted to 15° to 30°C (59° to 86°F). [See USP Controlled Room Temperature]
Protect from light, moisture, freezing, and excessive heat.
Dispense in a tight, light-resistant container as defined in the USP.
Wyeth ®
Wyeth Pharmaceuticals Inc.W10478C003
Philadelphia, PA 19101ET01
Rev 07/04
Subscribe to the "News" RSS Feed 
TOP ۞
