-
Zemaira (Zlb Behring)
Rx only
DESCRIPTION
Alpha 1 -Proteinase Inhibitor (Human), Zemaira®, is a sterile, stable, lyophilized preparation of highly purified human alpha 1 -proteinase inhibitor (A 1 -PI), also known as alpha 1 -antitrypsin, derived from human plasma. Zemaira® is manufactured from large pools of human plasma by cold ethanol fractionation according to a modified Cohn process followed by additional purification steps.
Zemaira® is supplied as a sterile, white, lyophilized powder to be administered by the intravenous route. The specific activity of Zemaira® is >/=0.7 mg of functional A 1 -PI per milligram of total protein. The purity is >/=90% A 1 -PI. Following reconstitution with 20 mL of Sterile Water for Injection, USP, each vial contains approximately 1000 mg of functionally active A 1 -PI, 81 mM sodium, 38 mM chloride, 17 mM phosphate, and 144 mM mannitol. Hydrochloric acid and/or sodium hydroxide may have been added to adjust the pH. Zemaira® contains no preservatives.
Each vial of Zemaira® contains the labeled amount of functionally active A 1 -PI in milligrams as stated on the vial label as determined by its capacity to neutralize human neutrophil elastase.
The plasma used in the manufacture of this product has been tested and found to be nonreactive to HBsAg, nonreactive for antibody to Hepatitis C Virus (Anti-HCV), and negative for antibody to Human Immunodeficiency Virus (Anti-HIV-1/HIV-2).
Two viral reduction steps are employed in the manufacture of Zemaira®: pasteurization at 60°C for 10 hours in an aqueous solution with stabilizers and two sequential ultrafiltration steps. These viral reduction steps have been validated in a series of in vitro experiments for their capacity to inactivate/remove Human Immunodeficiency Virus (HIV), Hepatitis A Virus (HAV), and the following model viruses: Bovine Viral Diarrhea Virus (BVDV) as a model virus for HCV, Canine Parvovirus (CPV) as a model virus for Parvovirus B19, and Pseudorabies Virus (PRV) as a non-specific model virus to cover a wide range of physiochemical properties of the viruses studied. Total mean log 10 reductions range from 6.8 to>12.2 log 10 as shown in Table 1.
Table 1: Mean (cumulative) virus reduction factors Mean Reduction Factor
Pasteurization
[log 10 ]Mean Reduction Factor
Two Ultrafiltration
Steps [log 10 ]Cumulative Reduction
Factor [log 10 ]HIV-1>/=6.7 >/=5.5 >/=12.2 BVDV>/=5.9 5.1 >/=11.0 PRV4.3 >/=6.9 >/=11.2 HAV>/=5.4 >/=6.3 >/=11.7 CPV(0.9) 6.8 6.8 CLINICAL PHARMACOLOGY
Alpha 1 -proteinase inhibitor (A 1 -PI) deficiency is a chronic, hereditary, autosomal, co-dominant disorder that is usually fatal in its severe form. Low blood levels of A 1 -PI are most commonly associated with progressive, severe emphysema that becomes clinically apparent by the third to fourth decade of life. However, an unknown percentage of individuals with severe A 1 -PI deficiency apparently never develop clinically evident emphysema during their lifetimes. A recent registry study showed 54% of A 1 -PI deficient subjects had emphysema. 1 Another registry study showed 72% of A 1 -PI deficient subjects had pulmonary symptoms. 2 Smoking is an important risk factor for the development of emphysema in patients with A 1 -PI deficiency. Less commonly, low blood levels of A 1 -PI are associated with liver disease and liver cirrhosis. 3 , 4 , 5
Approximately 100 genetic variants of A 1 -PI deficiency can be identified electrophoretically, only some of which are associated with the clinical disease. 6 , 7 Ninety-five percent of A 1 -PI deficient individuals are of the severe PiZZ phenotype. Up to 39% of A 1 -PI deficient patients may have an asthmatic component to their lung disease, as evidenced by symptoms and/or bronchial hyperreactivity. 1 Pulmonary infections, including pneumonia and acute bronchitis, are common in A 1 -PI deficient patients and contribute significantly to the morbidity of the disease.
The most direct approach to therapy for A 1 -PI deficiency in patients with emphysema has been to partially replace the missing protease inhibitor by intravenous infusion and, thus, attempt to ameliorate the imbalance in the anti-neutrophil elastase protection of the lower respiratory tract. Individuals with endogenous levels of A 1 -PI below 11 µM, in general, manifest a significantly increased risk for development of emphysema above the general population background risk. 3 , 4 , 7 , 8 Therefore, the maintenance of blood serum levels of A 1 -PI (antigenically measured) above 11 µM is historically thought to provide therapeutically relevant anti-neutrophil elastase protection. 9 However, the hypothesis that maintaining a serum level of antigenic A 1 -PI will restore protease-antiprotease balance and prevent further lung damage has never been tested in an adequately-powered controlled clinical trial.
Mechanism of Action
Pulmonary disease, particularly emphysema, is the most frequent manifestation of A 1 -PI deficiency. 7 The pathogenesis of emphysema is understood to evolve as described in the "protease-antiprotease imbalance" model. A 1 -PI is now understood to be the primary antiprotease in the lower respiratory tract, where it inhibits neutrophil elastase (NE). 10 Normal healthy individuals produce sufficient A 1 -PI to control the NE produced by activated neutrophils and are thus able to prevent inappropriate proteolysis of lung tissue by NE. Conditions that increase neutrophil accumulation and activation in the lung, such as respiratory infection and smoking, will in turn increase levels of NE. However, individuals who are severely deficient in endogenous A 1 -PI are unable to maintain an appropriate antiprotease defense and are thereby subject to more rapid proteolysis of the alveolar walls leading to chronic lung disease. Zemaira® serves as A 1 -PI augmentation therapy in this patient population, acting to increase and maintain serum levels and lung epithelial lining fluid (ELF) levels of A 1 -PI.
In 18 subjects treated with a single dose (60 mg/kg) of Zemaira®, the mean area under the curve (AUC) and standard deviation (SD) were 144 µM × day (SD 27), maximum serum concentration was 44.1 µM (SD 10.8), clearance was 603 mL per day (SD 129), and terminal half-life was 5.1 days (SD 2.4).
Weekly repeated infusions of A 1 -PI at a dose of 60 mg/kg lead to serum A 1 -PI levels above the historical target threshold of 11 µM.
CLINICAL STUDIES
Clinical studies were conducted with Zemaira® in 89 subjects (59 males and 30 females). The subjects ranged in age from 29 to 68 years (median age 49 years). Ninety-seven percent of the treated subjects had the PiZZ phenotype of A 1 -PI deficiency, and 3% had the M MALTON phenotype. At screening, serum A 1 -PI levels were between 3.2 and 10.1 µM (mean of 5.6 µM). The objectives of the clinical studies were to demonstrate that Alpha 1 -Proteinase Inhibitor (Human), Zemaira® augments and maintains serum levels of A 1 -PI above 11 µM and increases A 1 -PI levels in ELF of the lower lung.
In a double-blind, controlled clinical study to evaluate the safety and efficacy of Zemaira®, 44 subjects were randomized to receive 60 mg/kg of either Zemaira® or Prolastin® (a commercially available Alpha 1 -Proteinase Inhibitor [Human] product) once weekly for 10 weeks. After 10 weeks, all subjects received Zemaira® for an additional 14 weeks. All subjects were followed for a total of 24 weeks to complete the safety evaluation. The mean trough serum A 1 -PI levels at steady state (Weeks 7-11) in the Zemaira®-treated subjects were statistically equivalent to those in the Prolastin®-treated subjects. Both groups were maintained above 11 µM (80 mg/dL). The mean (range and standard deviation) of the steady state trough serum antigenic A 1 -PI level for Zemaira®-treated subjects was 17.7 µM (range 13.9 to 23.2, SD 2.5) and for Prolastin®-treated subjects was 19.1 µM (range 14.7 to 23.1, SD 2.2). The difference between the Zemaira® and the Prolastin® groups was not considered clinically significant and may be related to the higher specific activity of Zemaira®.
In a subgroup of subjects enrolled in the study (10 Zemaira®-treated subjects and 5 Prolastin®-treated subjects), bronchoalveolar lavage was performed at baseline and at Week 11. Four A 1 -PI related analytes in ELF were measured: antigenic A 1 -PI, A 1 -PI:NE complexes, free NE, and functional A 1 -PI (anti-neutrophil elastase capacity, ANEC). A blinded retrospective analysis, which revised the prospectively established acceptance criteria showed that within each treatment group, ELF levels of antigenic A 1 -PI and A 1 -PI:NE complexes increased from baseline to Week 11. Free elastase was immeasurably low in all samples. The post-treatment ANEC values in ELF were not significantly different between the Zemaira®-treated and Prolastin®-treated subjects (mean 1725 nM vs. 1418 nM). No conclusions can be drawn about changes of ANEC values in ELF during the study period as baseline values in the Zemaira®-treated subjects were unexpectedly high. No A 1 -PI analytes showed any clinically significant differences between the Zemaira® and Prolastin® treatment groups.
Table 2: ELF Analytes -- change from baseline AnalyteTreatment Mean change
from baseline90% Cl A 1 -PI (nM)Zemaira® 1358.3 822.6 to 1894.0 Prolastin® 949.9 460.0 to 1439.7 ANEC (nM)Zemaira® -588.1 -2032.3 to 856.1 Prolastin® 497.5 -392.3 to 1387.2 A 1 -PI:NE Complexes (nM)Zemaira® 118.0 39.9 to 196.1 Prolastin® 287.1 49.8 to 524.5
Subjects were also monitored for the presence of antibodies to HIV and markers for viral hepatitis (HAV, HBV, and HCV). Subjects who were negative for Hepatitis B surface antigen (HBsAg) at screening were vaccinated against Hepatitis B. Zemaira®-treated subjects were tested six months after the end of treatment for HAV, HBV, HCV, HIV, and Parvovirus B19, and no evidence of viral transmission was observed. No subjects developed detectable antibodies to Zemaira®.
INDICATIONS AND USAGE
Zemaira® is indicated for chronic augmentation and maintenance therapy in individuals with alpha 1 -proteinase inhibitor (A 1 -PI) deficiency and clinical evidence of emphysema.
Zemaira® increases antigenic and functional (ANEC) serum levels and lung epithelial lining fluid levels of A 1 -PI.
Clinical data demonstrating the long-term effects of chronic augmentation therapy of individuals with Zemaira® are not available.
Safety and effectiveness in pediatric patients have not been established.
Zemaira® is not indicated as therapy for lung disease patients in whom severe congenital A 1 -PI deficiency has not been established.
CONTRAINDICATIONS
Zemaira® is contraindicated in individuals with a known hypersensitivity to any of its components. Zemaira® is also contraindicated in individuals with a history of anaphylaxis or severe systemic response to A 1 -PI products.
Individuals with selective IgA deficiencies who have known antibodies against IgA (anti-IgA antibodies) should not receive Zemaira®, since these patients may experience severe reactions, including anaphylaxis, to IgA that may be present in Zemaira®.
WARNINGS
Zemaira® is made from human plasma. Products made from human plasma may contain infectious agents, such as viruses, that can cause disease. Because Zemaira® is made from human blood, it may carry a risk of transmitting infectious agents, e.g., viruses, and theoretically the Creutzfeldt-Jakob disease (CJD) agent. The risk that such products will transmit an infectious agent has been reduced by screening plasma donors for prior exposure to certain viruses, by testing for the presence of certain current virus infections, and by inactivating and/or removing certain viruses during manufacture. (See DESCRIPTION section for viral reduction measures). The manufacturing procedure for Zemaira® includes processing steps designed to reduce further the risk of viral transmission. Stringent procedures utilized at plasma collection centers, plasma testing laboratories, and fractionation facilities are designed to reduce the risk of viral transmission. The primary viral reduction steps of the Zemaira® manufacturing process are pasteurization (60°C for 10 hours) and two sequential ultrafiltration steps. Additional purification procedures used in the manufacture of Zemaira® also potentially provide viral reduction. Despite these measures, such products may still potentially contain human pathogenic agents, including those not yet known or identified. Thus, the risk of transmission of infectious agents can not be totally eliminated. Any infections thought by a physician possibly to have been transmitted by this product should be reported by the physician or other healthcare provider to Zlb Behring at 800-504-5434. The physician should discuss the risks and benefits of this product with the patient.
Individuals who receive infusions of blood or plasma products may develop signs and/or symptoms of some viral infections (see Information For Patients ).
During clinical studies, no cases of hepatitis A, B, C, or HIV viral infections were reported with the use of Zemaira®.
PRECAUTIONS
General -- Infusion rates and the patient's clinical state should be monitored closely during infusion. The patient should be observed for signs of infusion-related reactions.
As with any colloid solution, there may be an increase in plasma volume following intravenous administration of Zemaira®. Caution should therefore be used in patients at risk for circulatory overload.
Information For Patients -- Patients should be informed of the early signs of hypersensitivity reactions including hives, generalized urticaria, tightness of the chest, dyspnea, wheezing, faintness, hypotension, and anaphylaxis. Patients should be advised to discontinue use of the product and contact their physician and/or seek immediate emergency care, depending on the severity of the reaction, if these symptoms occur.
As with all plasma-derived products, some viruses, such as parvovirus B19, are particularly difficult to remove or inactivate at this time. Parvovirus B19 may most seriously affect pregnant women and immune-compromised individuals. Symptoms of parvovirus B19 include fever, drowsiness, chills, and runny nose followed two weeks later by a rash and joint pain. Patients should be encouraged to consult their physician if such symptoms occur.
Pregnancy Category C -- Animal reproduction studies have not been conducted with Zemaira®. It is also not known whether Zemaira® can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. Zemaira® should be given to a pregnant woman only if clearly needed.
Nursing Mothers -- It is not known whether Zemaira® is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when Zemaira® is administered to a nursing woman.
Pediatric Use -- Safety and effectiveness in the pediatric population have not been established.
Geriatric Use -- Clinical studies of Alpha 1 -Proteinase Inhibitor (Human), Zemaira® did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. As for all patients, dosing for geriatric patients should be appropriate to their overall situation.
ADVERSE REACTIONS
Intravenous administration of Zemaira®, 60 mg/kg weekly, has been shown to be generally well tolerated. In clinical studies, the following treatment-related adverse reactions were reported: asthenia, injection site pain, dizziness, headache, paresthesia, and pruritus. Each of these related adverse events was observed in 1 of 89 subjects (1%). The adverse reactions were mild.
Should evidence of an acute hypersensitivity reaction be observed, the infusion should be stopped promptly and appropriate countermeasures and supportive therapy should be administered.
Table 3 summarizes the adverse event data obtained with single and multiple doses during clinical trials with Zemaira® and Prolastin®. No clinically significant differences were detected between the two treatment groups.
Table 3: Summary of Adverse Events Zemaira® Prolastin® No. of subjects treated89 32 No. of subjects with adverse events regardless of causality (%)69 (78%) 20 (63%) No. of subjects with related adverse events (%)5 (6%) 4 (13%) No. of subjects with related serious adverse events0 0 No. of infusions1296 160 No. of adverse events regardless of causality (rates per infusion)298 (0.230) 83 (0.519) No. of related adverse events (rates per infusion)6 (0.005) 5 (0.031)
The frequencies of adverse events per infusion that were >/=0.4% in Zemaira®-treated subjects, regardless of causality, were: headache (33 events per 1296 infusions, 2.5%), upper respiratory infection (1.6%), sinusitis (1.5%), injection site hemorrhage (0.9%), sore throat (0.9%), bronchitis (0.8%), asthenia (0.6%), fever (0.6%), pain (0.5%), rhinitis (0.5%), bronchospasm (0.5%), chest pain (0.5%), increased cough (0.4%), rash (0.4%), and infection (0.4%).
The following adverse events, regardless of causality, occurred at a rate of 0.2% to <0.4% per infusion: abdominal pain, diarrhea, dizziness, ecchymosis, myalgia, pruritus, vasodilation, accidental injury, back pain, dyspepsia, dyspnea, hemorrhage, injection site reaction, lung disorder, migraine, nausea, and paresthesia.
Diffuse interstitial lung disease was noted on a routine chest x-ray of one subject at Week 24. Causality could not be determined.
In a retrospective analysis, during the 10-week blinded portion of the 24-week clinical study, 6 subjects (20%) of the 30 treated with Zemaira® had a total of 7 exacerbations of their chronic obstructive pulmonary disease (COPD). Nine subjects (64%) of the 14 treated with Prolastin® had a total of 11 exacerbations of their COPD. The observed difference between groups was 44% (95% confidence interval from 8% to 70%). Over the entire 24-week treatment period, of the 30 subjects in the Zemaira® treatment group, 7 subjects (23%) had a total of 11 exacerbations of their COPD.
DOSAGE AND ADMINISTRATION
Each vial of Zemaira® contains the labeled amount of functionally active A 1 -PI in milligrams as stated on the vial label as determined by capacity to neutralize human neutrophil elastase. The recommended dose of Zemaira® is 60 mg/kg body weight administered once weekly.
When reconstituted as directed, Zemaira® may be administered intravenously at a rate of approximately 0.08 mL/kg/min as determined by the response and comfort of the patient. The recommended dosage of 60 mg/kg body weight will take approximately 15 minutes to infuse.
Preparation
Each product package contains one Zemaira® single use vial, one 20 mL vial of Sterile Water for Injection, USP (diluent), one color-coded vented transfer device with air inlet filter, and one large volume 5 micron conical filter. Administer within three hours after reconstitution.
Reconstitution
- Bring both product (green cap) vial and diluent (white cap) vial to room temperature prior to reconstitution.
-
Remove the plastic flip-top caps from the vials. Aseptically cleanse the rubber stoppers with antiseptic solution and allow them to dry.
NOTE: The transfer device (Fig. 1) provided in the package is comprised of a white (diluent) end, which has a double orifice, and a green (product) end, which has a single orifice. Incorrect use of the transfer device will result in loss of vacuum and prevent transfer of the diluent, thereby preventing reconstitution of the product.
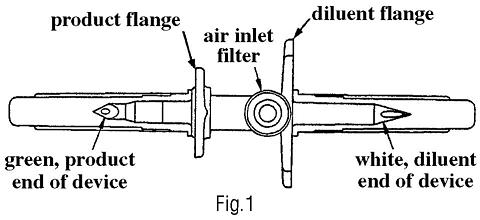
The transfer device is sterile. Do not touch
the exposed ends of the spike
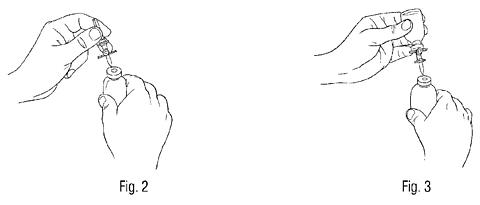
after removing the protective covers. - Remove the protective cover from the white (diluent) end of the transfer device. Insert the white end of the transfer device into the center of the stopper of the upright diluent vial first. (Fig. 2)
- Remove the protective cover from the green (product) end of the transfer device. Invert the diluent vial with the attached transfer device and, using minimum force, insert the green end of the transfer device into the center of the rubber stopper of the upright Zemaira® vial (green top). (Fig. 3) The flange of the transfer device should rest on the surface of the stopper so that the diluent flows into the Zemaira® vial.
- Allow the vacuum in the Zemaira® vial to pull the diluent into the Zemaira® vial.
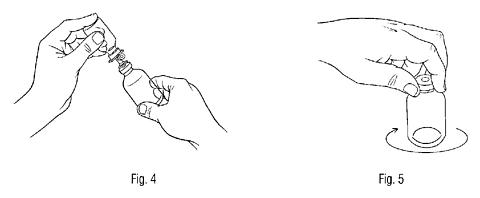
- During diluent transfer, wet the lyophilized cake completely by gently tilting the Zemaira® vial. (Fig. 4) Do not allow the air inlet filter to face downward. Care should be taken not to lose the vacuum, as this will prolong reconstitution of the product.
- After diluent transfer is complete, the transfer device will allow filtered air into the Zemaira® vial through the air filter. Additional venting of the product vial after diluent transfer is complete is not required. When diluent transfer is complete, withdraw the transfer device and diluent vial and properly discard in accordance with biohazard procedures.
- Gently swirl the Zemaira® vial until the powder is completely dissolved. (Fig. 5) DO NOT SHAKE.
-
Parenteral drug preparations should be inspected visually for particulate matter and discoloration prior to administration. Administer at room temperature within three hours after reconstitution.
Pooling Reconstituted Vials
If more than one vial of Alpha 1 -Proteinase Inhibitor (Human), Zemaira® is needed to achieve the required dose, use an aseptic technique to transfer the reconstituted solution from the vials into the administration container (e.g., empty I.V. bag or glass bottle).
Administration
Parenteral drug preparations should be inspected visually for particulate matter and discoloration prior to administration. Administer at room temperature within three hours after reconstitution.
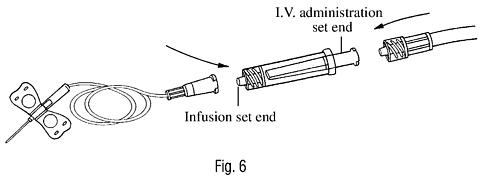
The reconstituted solution should be filtered during administration. To ensure proper filtration of Zemaira®, place the large volume 5 micron conical filter (provided) between the distal end of the I.V. administration set and the infusion set. (Fig. 6) Follow the appropriate procedure for I.V. administration.
After administration, any unused solution and administration equipment should be discarded in accordance with biohazard procedures.
HOW SUPPLIED
Zemaira® is supplied in a single use vial containing the labeled amount of functionally active A 1 -PI, as stated on the label. Each product package (NDC 0053-7201-02) contains one single use vial of Zemaira®, one 20 mL vial of Sterile Water for Injection, USP (diluent), one vented transfer device, and one large volume 5 micron conical filter.
STORAGE
When stored up to 25°C (77°F), Zemaira® is stable for the period indicated by the expiration date on its label. Avoid freezing which may damage container for the diluent.
REFERENCES
-
Stoller JK, Brantly M,
et al.
Formation and current results of a patient-organized registry for (alpha)
1
-antitrypsin deficiency.
Chest
118(3):843-848, 2000.
-
McElvaney NG, Stoller JK,
et al.
Baseline Characteristics of Enrollees in the National Heart, Lung, and Blood Institute Registry of (alpha)
1
-Antitrypsin Deficiency.
Chest
111:394-403, 1997.
-
Eriksson S. Pulmonary Emphysema and Alpha
1
-Antitrypsin Deficiency.
ACTA Med Scand
175(2):197-205, 1964.
-
Eriksson S. Studies in (alpha)
1
-antitrypsin deficiency.
ACTA Med Scand
Suppl. 432:1-85, 1965.
-
Morse JO. Alpha
1
-Antitrypsin Deficiency.
N Engl J Med
299:1045-1048; 1099-1105, 1978.
-
Crystal RG. (alpha)
1
-Antitrypsin Deficiency, Emphysema, and Liver Disease; Genetic Basis and Strategies for Therapy.
J Clin Invest
85:1343-1352, 1990.
-
World Health Organization. Alpha-1-Antitrypsin Deficiency; Report of a WHO Meeting. Geneva. 18-20 March 1996.
-
Gadek JE, Crystal RG. (alpha)
1
-Antitrypsin Deficiency. In: The Metabolic Basis of Inherited Disease 5th ed. Stanbury JB, Wyngaarden JB, Frederickson DS,
et al
., eds: New York, McGraw-Hill. 1983; pp. 1450-1467.
-
American Thoracic Society. Guidelines for the Approach to the Patient with Severe Hereditary Alpha-1-Antitrypsin Deficiency.
Am Rev Respir Dis
140:1494-1497, 1989.
-
Gadek JE, Fells GA, Zimmerman RL, Rennard SI, Crystal RG. Antielastases of the Human Alveolar Structures; Implications for the Protease-Antiprotease Theory of Emphysema.
J Clin Invest
68:889-898, 1981.
Prolastin® is a registered trademark of Bayer Corporation.
Manufactured by:
Zlb Behring LLC
Kankakee, IL 60901 USA
US License No. 1709
Revised: August, 2004 19131-03
Subscribe to the "News" RSS Feed 
TOP ۞
