-
Zonegran Capsules (Eisai)
DESCRIPTION
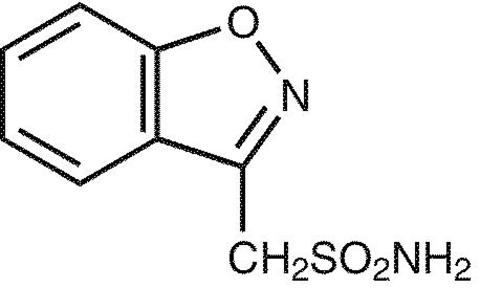
ZONEGRAN® (zonisamide) is an antiseizure drug chemically classified as a sulfonamide and unrelated to other antiseizure agents. The active ingredient is zonisamide, 1,2-benzisoxazole-3-methanesulfonamide. The empirical formula is C 8 H 8 N 2 O 3 S with a molecular weight of 212.23. Zonisamide is a white powder, pKa = 10.2, and is moderately soluble in water (0.80 mg/mL) and 0.1 N HCl (0.50 mg/mL). The chemical structure is:
ZONEGRAN is supplied for oral administration as capsules containing 25 mg, 50 mg or 100 mg zonisamide. Each capsule contains the labeled amount of zonisamide plus the following inactive ingredients: microcrystalline cellulose, hydrogenated vegetable oil, sodium lauryl sulfate, gelatin, and colorants.
CLINICAL PHARMACOLOGY
Mechanism of Action: The precise mechanism(s) by which zonisamide exerts its antiseizure effect is unknown. Zonisamide demonstrated anticonvulsant activity in several experimental models. In animals, zonisamide was effective against tonic extension seizures induced by maximal electroshock but ineffective against clonic seizures induced by subcutaneous pentylenetetrazol. Zonisamide raised the threshold for generalized seizures in the kindled rat model and reduced the duration of cortical focal seizures induced by electrical stimulation of the visual cortex in cats. Furthermore, zonisamide suppressed both interictal spikes and the secondarily generalized seizures produced by cortical application of tungstic acid gel in rats or by cortical freezing in cats. The relevance of these models to human epilepsy is unknown.
Zonisamide may produce these effects through action at sodium and calcium channels. In vitro pharmacological studies suggest that zonisamide blocks sodium channels and reduces voltage-dependent, transient inward currents (T-type Ca 2+ currents), consequently stabilizing neuronal membranes and suppressing neuronal hypersynchronization. In vitro binding studies have demonstrated that zonisamide binds to the GABA/benzodiazepine receptor ionophore complex in an allosteric fashion which does not produce changes in chloride flux. Other in vitro studies have demonstrated that zonisamide (10-30 µg/mL) suppresses synaptically-driven electrical activity without affecting postsynaptic GABA or glutamate responses (cultured mouse spinal cord neurons) or neuronal or glial uptake of [ 3 H]-GABA (rat hippocampal slices). Thus, zonisamide does not appear to potentiate the synaptic activity of GABA. In vivo microdialysis studies demonstrated that zonisamide facilitates both dopaminergic and serotonergic neurotransmission. Zonisamide also has weak carbonic anhydrase inhibiting activity, but this pharmacologic effect is not thought to be a major contributing factor in the antiseizure activity of zonisamide.
Pharmacokinetics: Following a 200-400 mg oral zonisamide dose, peak plasma concentrations (range: 2-5 µg/mL) in normal volunteers occur within 2-6 hours. In the presence of food, the time to maximum concentration is delayed, occurring at 4-6 hours, but food has no effect on the bioavailability of zonisamide. Zonisamide extensively binds to erythrocytes, resulting in an eight-fold higher concentration of zonisamide in red blood cells (RBC) than in plasma. The pharmacokinetics of zonisamide are dose proportional in the range of 200-400 mg, but the C max and AUC increase disproportionately at 800 mg, perhaps due to saturable binding of zonisamide to RBC. Once a stable dose is reached, steady state is achieved within 14 days. The elimination half-life of zonisamide in plasma is about 63 hours. The elimination half-life of zonisamide in RBC is approximately 105 hours.
The apparent volume of distribution (V/F) of zonisamide is about 1.45 L/kg following a 400 mg oral dose. Zonisamide, at concentrations of 1.0-7.0 µg/mL, is approximately 40% bound to human plasma proteins. Protein binding of zonisamide is unaffected in the presence of therapeutic concentrations of phenytoin, phenobarbital or carbamazepine.
Metabolism and Excretion: Following oral administration of 14 C-zonisamide to healthy volunteers, only zonisamide was detected in plasma. Zonisamide is excreted primarily in urine as parent drug and as the glucuronide of a metabolite. Following multiple dosing, 62% of the 14 C dose was recovered in the urine, with 3% in the feces by day 10. Zonisamide undergoes acetylation to form N-acetyl zonisamide and reduction to form the open ring metabolite, 2-sulfamoylacetyl phenol (SMAP). Of the excreted dose, 35% was recovered as zonisamide, 15% as N-acetyl zonisamide, and 50% as the glucuronide of SMAP. Reduction of zonisamide to SMAP is mediated by cytochrome P450 isozyme 3A4 (CYP3A4). Zonisamide does not induce its own metabolism. Plasma clearance of zonisamide is approximately 0.30-0.35 mL/min/kg in patients not receiving enzyme-inducing antiepilepsy drugs (AEDs). The clearance of zonisamide is increased to 0.5 mL/min/kg in patients concurrently on enzyme-inducing AEDs.
Renal clearance is about 3.5 mL/min. The clearance of an oral dose of zonisamide from RBC is 2 mL/min.
Special Populations:
Renal Insufficiency: Single 300 mg zonisamide doses were administered to three groups of volunteers. Group 1 was a healthy group with a creatinine clearance ranging from 70-152 mL/min. Group 2 and Group 3 had creatinine clearances ranging from 14.5-59 mL/min and 10-20 mL/min, respectively. Zonisamide renal clearance decreased with decreasing renal function (3.42, 2.50, 2.23 mL/min, respectively). Marked renal impairment (creatinine clearance < 20 mL/min) was associated with an increase in zonisamide AUC of 35% (see DOSAGE AND ADMINISTRATION section).
Hepatic Disease: The pharmacokinetics of zonisamide in patients with impaired liver function have not been studied (see DOSAGE AND ADMINISTRATION section).
Age: The pharmacokinetics of a 300 mg single dose of zonisamide was similar in young (mean age 28 years) and elderly subjects (mean age 69 years).
Gender and Race: Information on the effect of gender and race on the pharmacokinetics of zonisamide is not available.
Interactions of Zonisamide with Other Antiepilepsy Drugs (AEDs): Concurrent medication with drugs that either induce or inhibit CYP3A4 may alter serum concentrations of zonisamide. Concomitant administration of phenytoin and carbamazepine increases zonisamide plasma clearance from 0.30-0.35 mL/min/kg to 0.35-0.5 mL/min/kg. The half-life of zonisamide is decreased to 27 hours by phenytoin, to 38 hours by phenobarbital and carbamazepine, and to 46 hours by valproate. Plasma protein binding of phenytoin and carbamazepine was not affected by zonisamide administration (see PRECAUTIONS , Drug Interactions subsection).
Clinical Studies: The effectiveness of ZONEGRAN as adjunctive therapy (added to other antiepilepsy drugs) has been established in three multicenter, placebo-controlled, double blind, 3-month clinical trials (two domestic, one European) in 499 patients with refractory partial onset seizures with or without secondary generalization. Each patient had a history of at least four partial onset seizures per month in spite of receiving one or two antiepilepsy drugs at therapeutic concentrations. The 499 patients (209 women, 290 men) ranged in age from 13-68 years with a mean age of about 35 years. In the two US studies, over 80% of patients were Caucasian; 100% of patients in the European study were Caucasian. ZONEGRAN or placebo was added to the existing therapy. The primary measure of effectiveness was median percent reduction from baseline in partial seizure frequency. The secondary measure was proportion of patients achieving a 50% or greater seizure reduction from baseline (responders). The results described below are for all partial seizures in the intent-to-treat populations.
In the first study (n = 203), all patients had a 1-month baseline observation period, then received placebo or ZONEGRAN in one of two dose escalation regimens; either 1) 100 mg/day for five weeks, 200 mg/day for one week, 300 mg/day for one week, and then 400 mg/day for five weeks; or 2) 100 mg/day for one week, followed by 200 mg/day for five weeks, then 300 mg/day for one week, then 400 mg/day for five weeks. This design allowed a 100 mg vs. placebo comparison over weeks 1-5, and a 200 mg vs. placebo comparison over weeks 2-6; the primary comparison was 400 mg (both escalation groups combined) vs. placebo over weeks 8-12. The total daily dose was given as twice a day dosing. Statistically significant treatment differences favoring ZONEGRAN were seen for doses of 100, 200, and 400 mg/day.
In the second (n = 152) and third (n = 138) studies, patients had a 2-3 month baseline, then were randomly assigned to placebo or ZONEGRAN for three months. ZONEGRAN was introduced by administering 100 mg/day for the first week, 200 mg/day the second week, then 400 mg/day for two weeks, after which the dose (ZONEGRAN or placebo) could be adjusted as necessary to a maximum dose of 20 mg/kg/day or a maximum plasma level of 40 µg/mL. In the second study, the total daily dose was given as twice a day dosing; in the third study, it was given as a single daily dose. The average final maintenance doses received in the studies were 530 and 430 mg/day in the second and third studies, respectively. Both studies demonstrated statistically significant differences favoring ZONEGRAN for doses of 400-600 mg/day, and there was no apparent difference between once daily and twice daily dosing (in different studies). Analysis of the data (first 4 weeks) during titration demonstrated statistically significant differences favoring ZONEGRAN at doses between 100 and 400 mg/day. The primary comparison in both trials was for any dose over Weeks 5-12.
Table 1. Median % Reduction in All Partial Seizures and % Responders in
Primary Efficacy Analyses: Intent-To-Treat AnalysisStudy Median % reduction in partial seizures % Responders ZONEGRAN Placebo ZONEGRAN Placebo Study 1:n=98 n=72 n=98 n=72 Weeks 8-12:40.5% * 9.0% 41.8% * 22.2% Study 2:n=69 n=72 n=69 n=72 Weeks 5-12:29.6% * -3.2% 29.0% 15.0% Study 3:n=67 n=66 n=67 n=66 Weeks 5-12:27.2% * -1.1% 28.0% * 12.0% *p<0.05 compared to placebo Table 2. Median % Reduction in All Partial Seizures and % Responders for Dose Analyses in Study 1: Intent-To-Treat Analysis Dose Group Median % reduction in partial seizures % Responders ZONEGRAN Placebo ZONEGRAN Placebo 100-400 mg/day:n=112 n=83 n=112 n=83 Weeks 1-12:32.3% * 5.6% 32.1% * 9.6% 100 mg/day:n=56 n=80 n=56 n=80 Weeks 1-5:24.7% * 8.3% 25.0% * 11.3% 200 mg/day:n=55 n=82 n=55 n=82 Weeks 2-6:20.4% * 4.0% 25.5% * 9.8% *p<0.05 compared to placebo
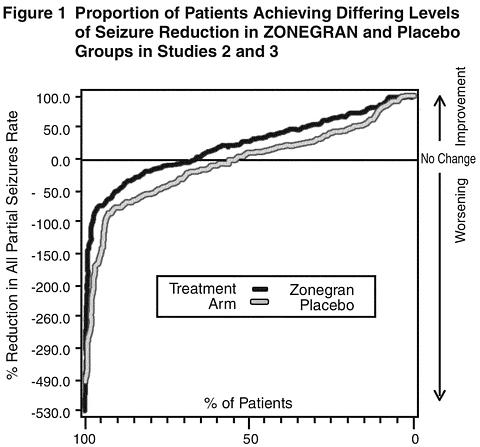
Figure 1 presents the proportion of patients (X-axis) whose percentage reduction from baseline in the all partial seizure rate was at least as great as that indicated on the Y-axis in the second and third placebo-controlled trials. A positive value on the Y-axis indicates an improvement from baseline (i.e., a decrease in seizure rate), while a negative value indicates a worsening from baseline (i.e., an increase in seizure rate). Thus, in a display of this type, the curve for an effective treatment is shifted to the left of the curve for placebo. The proportion of patients achieving any particular level of reduction in seizure rate was consistently higher for the ZONEGRAN groups compared to the placebo groups. For example, Figure 1 indicates that approximately 27% of patients treated with ZONEGRAN experienced a 75% or greater reduction, compared to approximately 12% in the placebo groups.
No differences in efficacy based on age, sex or race, as measured by a change in seizure frequency from baseline, were detected.
INDICATIONS AND USAGE
ZONEGRAN is indicated as adjunctive therapy in the treatment of partial seizures in adults with epilepsy.
CONTRAINDICATIONS
ZONEGRAN is contraindicated in patients who have demonstrated hypersensitivity to sulfonamides or zonisamide.
WARNINGS
Potentially Fatal Reactions to Sulfonamides: Fatalities have occurred, although rarely, as a result of severe reactions to sulfonamides (zonisamide is a sulfonamide) including Stevens-Johnson syndrome, toxic epidermal necrolysis, fulminant hepatic necrosis, agranulocytosis, aplastic anemia, and other blood dyscrasias. Such reactions may occur when a sulfonamide is readministered irrespective of the route of administration. If signs of hypersensitivity or other serious reactions occur, discontinue zonisamide immediately. Specific experience with sulfonamide-type adverse reaction to zonisamide is described below.
Serious Skin Reactions: Consideration should be given to discontinuing ZONEGRAN in patients who develop an otherwise unexplained rash. If the drug is not discontinued, patients should be observed frequently. Seven deaths from severe rash [i.e. Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN)] were reported in the first 11 years of marketing in Japan. All of the patients were receiving other drugs in addition to zonisamide. In post-marketing experience from Japan, a total of 49 cases of SJS or TEN have been reported, a reporting rate of 46 per million patient-years of exposure. Although this rate is greater than background, it is probably an underestimate of the true incidence because of under-reporting. There were no confirmed cases of SJS or TEN in the US, European, or Japanese development programs.
In the US and European randomized controlled trials, 6 of 269 (2.2%) zonisamide patients discontinued treatment because of rash compared to none on placebo. Across all trials during the US and European development, rash that led to discontinuation of zonisamide was reported in 1.4% of patients (12.0 events per 1000 patient-years of exposure). During Japanese development, serious rash or rash that led to study drug discontinuation was reported in 2.0% of patients (27.8 events per 1000 patient years). Rash usually occurred early in treatment, with 85% reported within 16 weeks in the US and European studies and 90% reported within two weeks in the Japanese studies. There was no apparent relationship of dose to the occurrence of rash.
Serious Hematologic Events: Two confirmed cases of aplastic anemia and one confirmed case of agranulocytosis were reported in the first 11 years of marketing in Japan, rates greater than generally accepted background rates. There were no cases of aplastic anemia and two confirmed cases of agranulocytosis in the US, European, or Japanese development programs. There is inadequate information to assess the relationship, if any, between dose and duration of treatment and these events.
Oligohidrosis and Hyperthermia in Pediatric Patients: Oligohidrosis, sometimes resulting in heat stroke and hospitalization, is seen in association with zonisamide in pediatric patients.
During the pre-approval development program in Japan, one case of oligohidrosis was reported in 403 pediatric patients, an incidence of 1 case per 285 patient-years of exposure. While there were no cases reported in the US or European development programs, fewer than 100 pediatric patients participated in these trials.
In the first 11 years of marketing in Japan, 38 cases were reported, an estimated reporting rate of about 1 case per 10,000 patient-years of exposure. In the first year of marketing in the US, 2 cases were reported, an estimated reporting rate of about 12 cases per 10,000 patient-years of exposure. These rates are underestimates of the true incidence because of under-reporting. There has also been one report of heat stroke in an 18-year-old patient in the US.
Decreased sweating and an elevation in body temperature above normal characterized these cases. Many cases were reported after exposure to elevated environmental temperatures. Heat stroke, requiring hospitalization, was diagnosed in some cases. There have been no reported deaths.
Pediatric patients appear to be at an increased risk for zonisamide-associated oligohidrosis and hyperthermia. Patients, especially pediatric patients, treated with Zonegran should be monitored closely for evidence of decreased sweating and increased body temperature, especially in warm or hot weather. Caution should be used when zonisamide is prescribed with other drugs that predispose patients to heat-related disorders; these drugs include, but are not limited to, carbonic anhydrase inhibitors and drugs with anticholinergic activity.
The practitioner should be aware that the safety and effectiveness of zonisamide in pediatric patients have not been established, and that zonisamide is not approved for use in pediatric patients.
Seizures on Withdrawal: As with other AEDs, abrupt withdrawal of ZONEGRAN in patients with epilepsy may precipitate increased seizure frequency or status epilepticus. Dose reduction or discontinuation of zonisamide should be done gradually.
Teratogenicity: Women of child bearing potential who are given zonisamide should be advised to use effective contraception. Zonisamide was teratogenic in mice, rats, and dogs and embryolethal in monkeys when administered during the period of organogenesis. A variety of fetal abnormalities, including cardiovascular defects, and embryo-fetal deaths occurred at maternal plasma levels similar to or lower than therapeutic levels in humans. These findings suggest that the use of ZONEGRAN during pregnancy in humans may present a significant risk to the fetus (see PRECAUTIONS , Pregnancy subsection). It cannot be said with any confidence, however, that even mild seizures do not pose some hazards to the developing fetus. Zonisamide should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Cognitive/Neuropsychiatric Adverse Events: Use of ZONEGRAN was frequently associated with central nervous system-related adverse events. The most significant of these can be classified into three general categories: 1) psychiatric symptoms, including depression and psychosis, 2) psychomotor slowing, difficulty with concentration, and speech or language problems, in particular, word-finding difficulties, and 3) somnolence or fatigue.
In placebo-controlled trials, 2.2% of patients discontinued ZONEGRAN or were hospitalized for depression compared to 0.4% of placebo patients, while 1.1% of ZONEGRAN and 0.4% of placebo patients attempted suicide. Among all epilepsy patients treated with ZONEGRAN, 1.4% were discontinued and 1.0% were hospitalized because of reported depression or suicide attempts. In placebo-controlled trials, 2.2% of patients discontinued ZONEGRAN or were hospitalized due to psychosis or psychosis-related symptoms compared to none of the placebo patients. Among all epilepsy patients treated with ZONEGRAN, 0.9% were discontinued and 1.4% were hospitalized because of reported psychosis or related symptoms.
Psychomotor slowing and difficulty with concentration occurred in the first month of treatment and were associated with doses above 300 mg/day. Speech and language problems tended to occur after 6-10 weeks of treatment and at doses above 300 mg/day. Although in most cases these events were of mild to moderate severity, they at times led to withdrawal from treatment.
Somnolence and fatigue were frequently reported CNS adverse events during clinical trials with ZONEGRAN. Although in most cases these events were of mild to moderate severity, they led to withdrawal from treatment in 0.2% of the patients enrolled in controlled trials. Somnolence and fatigue tended to occur within the first month of treatment. Somnolence and fatigue occurred most frequently at doses of 300-500 mg/day. Patients should be cautioned about this possibility and special care should be taken by patients if they drive, operate machinery, or perform any hazardous task.
PRECAUTIONS
General: Somnolence is commonly reported, especially at higher doses of ZONEGRAN (see WARNINGS: Cognitive/Neuropsychiatric Adverse Events subsection). Zonisamide is metabolized by the liver and eliminated by the kidneys; caution should therefore be exercised when administering ZONEGRAN to patients with hepatic and renal dysfunction (see CLINICAL PHARMACOLOGY , Special Populations subsection).
Kidney Stones: Among 991 patients treated during the development of ZONEGRAN, 40 patients (4.0%) with epilepsy receiving ZONEGRAN developed clinically possible or confirmed kidney stones (e.g. clinical symptomatology, sonography, etc.), a rate of 34 per 1000 patient-years of exposure (40 patients with 1168 years of exposure). Of these, 12 were symptomatic, and 28 were described as possible kidney stones based on sonographic detection. In nine patients, the diagnosis was confirmed by a passage of a stone or by a definitive sonographic finding. The rate of occurrence of kidney stones was 28.7 per 1000 patient-years of exposure in the first six months, 62.6 per 1000 patient-years of exposure between 6 and 12 months, and 24.3 per 1000 patient-years of exposure after 12 months of use. There are no normative sonographic data available for either the general population or patients with epilepsy. The clinical significance of the sonographic finding is unknown. The analyzed stones were composed of calcium or urate salts. In general, increasing fluid intake and urine output can help reduce the risk of stone formation, particularly in those with predisposing risk factors. It is unknown, however, whether these mea-sures will reduce the risk of stone formation in patients treated with ZONEGRAN.
Effect on Renal Function: In several clinical studies, zonisamide was associated with a statistically significant 8% mean increase from baseline of serum creatinine and blood urea nitrogen (BUN) compared to essentially no change in the placebo patients. The increase appeared to persist over time but was not progressive; this has been interpreted as an effect on glomerular filtration rate (GFR). There were no episodes of unexplained acute renal failure in clinical development in the US, Europe, or Japan. The decrease in GFR appeared within the first 4 weeks of treatment. In a 30-day study, the GFR returned to baseline within 2-3 weeks of drug discontinuation. There is no information about reversibility, after drug discontinuation, of the effects on GFR after long-term use. ZONEGRAN should be discontinued in patients who develop acute renal failure or a clinically significant sustained increase in the creatinine/BUN concentration. ZONEGRAN should not be used in patients with renal failure (estimated GFR <50 mL/min) as there has been insufficient experience concerning drug dosing and toxicity.
Sudden Unexplained Death in Epilepsy: During the development of ZONEGRAN, nine sudden unexplained deaths occurred among 991 patients with epilepsy receiving ZONEGRAN for whom accurate exposure data are available. This represents an incidence of 7.7 deaths per 1000 patient years. Although this rate exceeds that expected in a healthy population, it is within the range of estimates for the incidence of sudden unexplained deaths in patients with refractory epilepsy not receiving ZONEGRAN (ranging from 0.5 per 1000 patient-years for the general population of patients with epilepsy, to 2-5 per 1000 patient-years for patients with refractory epilepsy; higher incidences range from 9-15 per 1000 patient-years among surgical candidates and surgical failures). Some of the deaths could represent seizure-related deaths in which the seizure was not observed.
Status Epilepticus: Estimates of the incidence of treatment emergent status epilepticus in ZONEGRAN-treated patients are difficult because a standard definition was not employed. Nonetheless, in controlled trials, 1.1% of patients treated with ZONEGRAN had an event labeled as status epilepticus compared to none of the patients treated with placebo. Among patients treated with ZONEGRAN across all epilepsy studies (controlled and uncontrolled), 1.0% of patients had an event reported as status epilepticus.
Creatine Phosphokinase (CPK) Elevation and Pancreatitis: In the post-market setting, the following rare adverse events have been observed (<1:1000):
If patients taking zonisamide develop severe muscle pain and/or weakness, either in the presence or absence of a fever, markers of muscle damage should be assessed, including serum CPK and aldolase levels. If elevated, in the absence of another obvious cause such as trauma, grand mal seizures, etc., tapering and/or discontinuance of zonisamide should be considered and appropriate treatment initiated.
Patients taking zonisamide that manifest clinical signs and symptoms of pancreatitis should have pancreatic lipase and amylase levels monitored. If pancreatitis is evident, in the absence of another obvious cause, tapering and/or discontinuation of zonisamide should be considered and appropriate treatment initiated.
Information for Patients: Patients should be advised as follows:
- ZONEGRAN may produce drowsiness, especially at higher doses. Patients should be advised not to drive a car or operate other complex machinery until they have gained experience on ZONEGRAN sufficient to determine whether it affects their performance.
- Patients should contact their physician immediately if a skin rash develops or seizures worsen.
- Patients should contact their physician immediately if they develop signs or symptoms, such as sudden back pain, abdominal pain, and/or blood in the urine, that could indicate a kidney stone. Increasing fluid intake and urine output may reduce the risk of stone formation, particularly in those with predisposing risk factors for stones.
- Patients should contact their physician immediately if a child has been taking ZONEGRAN and is not sweating as usual with or without a fever.
- Because zonisamide can cause hematological complications, patients should contact their physician immediately if they develop a fever, sore throat, oral ulcers, or easy bruising.
- As with other AEDs, patients should contact their physician if they intend to become pregnant or are pregnant during ZONEGRAN therapy. Patients should notify their physician if they intend to breast-feed or are breast-feeding an infant.
- Patients should contact their physician immediately if they develop severe muscle pain and/or weakness.
Laboratory Tests: In several clinical studies, zonisamide was associated with a mean increase in the concentration of serum creatinine and blood urea nitrogen (BUN) of approximately 8% over the baseline measurement. Consideration should be given to monitoring renal function periodically (see PRECAUTIONS , Effect on Renal Function subsection).
Zonisamide was associated with an increase in serum alkaline phosphatase. In the randomized, controlled trials, a mean increase of approximately 7% over baseline was associated with zonisamide compared to a 3% mean increase in placebo-treated patients. These changes were not statistically significant. The clinical relevance of these changes is unknown.
Drug Interactions: Effects of ZONEGRAN on the pharmacokinetics of other antiepilepsy drugs (AEDs): Zonisamide had no appreciable effect on the steady state plasma concentrations of phenytoin, carbamazepine, or valproate during clinical trials. Zonisamide did not inhibit mixed-function liver oxidase enzymes (cytochrome P450), as measured in human liver microsomal preparations, in vitro . Zonisamide is not expected to interfere with the metabolism of other drugs that are metabolized by cytochrome P450 isozymes.
Effects of other drugs on ZONEGRAN pharmacokinetics: Drugs that induce liver enzymes increase the metabolism and clearance of zonisamide and decrease its half-life. The half-life of zonisamide following a 400 mg dose in patients concurrently on enzyme-inducing AEDs such as phenytoin, carbamazepine, or phenobarbital was between 27-38 hours; the half-life of zonisamide in patients concurrently on the non-enzyme inducing AED, valproate, was 46 hours. Concurrent medication with drugs that either induce or inhibit CYP3A4 would be expected to alter serum concentrations of zonisamide.
Interaction with cimetidine: Zonisamide single dose pharmacokinetic parameters were not affected by cimetidine (300 mg four times a day for 12 days).
Carcinogenicity, Mutagenesis, Impairment of Fertility: No evidence of carcinogenicity was found in mice or rats following dietary administration of zonisamide for two years at doses of up to 80 mg/kg/day. In mice, this dose is approximately equivalent to the maximum recommended human dose (MRHD) of 400 mg/day on a mg/m 2 basis. In rats, this dose is 1-2 times the MRHD on a mg/m 2 basis.
Zonisamide increased mutation frequency in Chinese hamster lung cells in the absence of metabolic activation. Zonisamide was not mutagenic or clastogenic in the Ames test, mouse lymphoma assay, sister chromatid exchange test, and human lymphocyte cytogenetics assay in vitro , and the rat bone marrow cytogenetics assay in vivo .
Rats treated with zonisamide (20, 60, or 200 mg/kg) before mating and during the initial gestation phase showed signs of reproductive toxicity (decreased corpora lutea, implantations, and live fetuses) at all doses. The low dose in this study is approximately 0.5 times the maximum recommended human dose (MRHD) on a mg/m 2 basis. The effect of zonisamide on human fertility is unknown.
Pregnancy: Pregnancy Category C (see WARNINGS, Teratogenicity subsection): Zonisamide was teratogenic in mice, rats, and dogs and embryolethal in monkeys when administered during the period of organogenesis. Fetal abnormalities or embryo-fetal deaths occurred in these species at zonisamide dosage and maternal plasma levels similar to or lower than therapeutic levels in humans, indicating that use of this drug in pregnancy entails a significant risk to the fetus. A variety of external, visceral, and skeletal malformations was produced in animals by prenatal exposure to zonisamide. Cardiovascular defects were prominent in both rats and dogs.
Following administration of zonisamide (10, 30, or 60 mg/kg/day) to pregnant dogs during organogenesis, increased incidences of fetal cardiovascular malformations (ventricular septal defects, cardiomegaly, various valvular and arterial anomalies) were found at doses of 30 mg/kg/day or greater. The low effect dose for malformations produced peak maternal plasma zonisamide levels (25 µg/mL) about 0.5 times the highest plasma levels measured in patients receiving the maximum recommended human dose (MRHD) of 400 mg/day. In dogs, cardiovascular malformations were found in approximately 50% of all fetuses exposed to the high dose, which was associated with maternal plasma levels (44 µg/mL) approximately equal to the highest levels measured in humans receiving the MRHD. Incidences of skeletal malformations were also increased at the high dose, and fetal growth retardation and increased frequencies of skeletal variations were seen at all doses in this study. The low dose produced maternal plasma levels (12 µg/mL) about 0.25 times the highest human levels.
In cynomolgus monkeys, administration of zonisamide (10 or 20 mg/kg/day) to pregnant animals during organogenesis resulted in embryo-fetal deaths at both doses. The possibility that these deaths were due to malformations cannot be ruled out. The lowest embryolethal dose in monkeys was associated with peak maternal plasma zonisamide levels (5 µg/mL) approximately 0.1 times the highest levels measured in patients at the MRHD.
In a mouse embryo-fetal development study, treatment of pregnant animals with zonisamide (125, 250, or 500 mg/kg/day) during the period of organogenesis resulted in increased incidences of fetal malformations (skeletal and/or craniofacial defects) at all doses tested. The low dose in this study is approximately 1.5 times the MRHD on a mg/m 2 basis. In rats, increased frequencies of malformations (cardiovascular defects) and variations (persistent cords of thymic tissue, decreased skeletal ossification) were observed among the offspring of dams treated with zonisamide (20, 60, or 200 mg/kg/day) throughout organogenesis at all doses. The low effect dose is approximately 0.5 times the MRHD on a mg/m 2 basis.
Perinatal death was increased among the offspring of rats treated with zonisamide (10, 30, or 60 mg/kg/day) from the latter part of gestation up to weaning at the high dose, or approximately 1.4 times the MRHD on a mg/m 2 basis. The no effect level of 30 mg/kg/day is approximately 0.7 times the MRHD on a mg/m 2 basis.
There are no adequate and well-controlled studies in pregnant women. ZONEGRAN should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Labor and Delivery: The effect of ZONEGRAN on labor and delivery in humans is not known.
Use in Nursing Mothers: It is not known whether zonisamide is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from zonisamide, a decision should be made whether to discontinue nursing or to discontinue drug, taking into account the importance of the drug to the mother. ZONEGRAN should be used in nursing mothers only if the benefits outweigh the risks.
Pediatric Use: The safety and effectiveness of ZONEGRAN in children under age 16 have not been established. Cases of oligohidrosis and hyperpyrexia have been reported (see WARNINGS , Oligohidrosis and Hyperthermia in Pediatric Patients subsection).
Geriatric Use: Single dose pharmacokinetic parameters are similar in elderly and young healthy volunteers (see CLINICAL PHARMACOLOGY , Special Populations subsection). Clinical studies of zonisamide did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
ADVERSE REACTIONS
The most commonly observed adverse events associated with the use of ZONEGRAN in controlled clinical trials that were not seen at an equivalent frequency among placebo-treated patients were somnolence, anorexia, dizziness, headache, nausea, and agitation/irritability.
In controlled clinical trials, 12% of patients receiving ZONEGRAN as adjunctive therapy discontinued due to an adverse event compared to 6% receiving placebo. Approximately 21% of the 1,336 patients with epilepsy who received ZONEGRAN in clinical studies discontinued treatment because of an adverse event. The adverse events most commonly associated with discontinuation were somnolence, fatigue and/or ataxia (6%), anorexia (3%), difficulty concentrating (2%), difficulty with memory, mental slowing, nausea/vomiting (2%), and weight loss (1%). Many of these adverse events were dose-related (see WARNINGS and PRECAUTIONS ).
Adverse Event Incidence in Controlled Clinical Trials: Table 3 lists treatment-emergent adverse events that occurred in at least 2% of patients treated with ZONEGRAN in controlled clinical trials that were numerically more common in the ZONEGRAN group. In these studies, either ZONEGRAN or placebo was added to the patient's current AED therapy. Adverse events were usually mild or moderate in intensity.
The prescriber should be aware that these figures, obtained when ZONEGRAN was added to concurrent AED therapy, cannot be used to predict the frequency of adverse events in the course of usual medical practice when patient characteristics and other factors may differ from those prevailing during clinical studies. Similarly, the cited frequencies cannot be directly compared with figures obtained from other clinical investigations involving different treatments, uses, or investigators. An inspection of these frequencies, however, does provide the prescriber with one basis by which to estimate the relative contribution of drug and non-drug factors to the adverse event incidences in the population studied.
TABLE 3: Incidence (%) of Treatment-Emergent Adverse Events in Placebo-Controlled, Add-On Trials (Events that occurred in at least 2% of ZONEGRAN-treated patients and occurred more frequently in ZONEGRAN-treated than placebo-treated patients) BODY SYSTEM/
PREFERRED
TERMZONEGRAN
(n=269)
%PLACEBO
(n=230)
%BODY AS A WHOLEHeadache10 8 Abdominal Pain6 3 Flu Syndrome4 3 DIGESTIVEAnorexia13 6 Nausea9 6 Diarrhea5 2 Dyspepsia3 1 Constipation2 1 Dry Mouth2 1 HEMATOLOGIC AND LYMPHATICEcchymosis2 1 METABOLIC AND NUTRITIONALWeight Loss3 2 NERVOUS SYSTEMDizziness13 7 Ataxia6 1 Nystagmus4 2 Paresthesia4 1 NEUROPSYCHIATRIC AND COGNITIVE DYSFUNCTION-
ALTERED COGNITIVE FUNCTIONConfusion6 3 Difficulty Concentrating6 2 Difficulty with Memory6 2 Mental Slowing4 2 NEUROPSYCHIATRIC AND COGNITIVE DYSFUNCTION-
BEHAVIORAL ABNORMALITIES (NON-PSYCHOSIS-RELATED)Agitation/Irritability9 4 Depression6 3 Insomnia6 3 Anxiety3 2 Nervousness2 1 NEUROPSYCHIATRIC AND COGNITIVE DYSFUNCTION-
BEHAVIORAL ABNORMALITIES (PSYCHOSIS-RELATED)Schizophrenic/
Schizophreniform
Behavior2 0 NEUROPSYCHIATRIC AND COGNITIVE DYSFUNCTION-
CNS DEPRESSIONSomnolence17 7 Fatigue8 6 Tiredness7 5 NEUROPSYCHIATRIC AND COGNITIVE DYSFUNCTION-
SPEECH AND LANGUAGE ABNORMALITIESSpeech Abnormalities5 2 Difficulties in Verbal
Expression2 <1 RESPIRATORYRhinitis2 1 SKIN AND APPENDAGESRash3 2 SPECIAL SENSESDiplopia6 3 Taste Perversion2 0 Other Adverse Events Observed During Clinical Trials: ZONEGRAN has been administered to 1,598 individuals during all clinical trials, only some of which were placebo-controlled. During these trials, all events were recorded by the investigators using their own terms. To provide a useful estimate of the proportion of individuals having adverse events, similar events have been grouped into a smaller number of standardized categories using a modified COSTART dictionary. The frequencies represent the proportion of the 1,598 individuals exposed to ZONEGRAN who experienced an event on at least one occasion. All events are included except those already listed in the previous table or discussed in WARNINGS or PRECAUTIONS , trivial events, those too general to be informative, and those not reasonably associated with ZONEGRAN.
Events are further classified within each category and listed in order of decreasing frequency as follows: frequent occurring in at least 1:100 patient; infrequent occurring in 1:100 to 1:1000 patients; rare occurring in fewer than 1:1000 patients.
Body as a Whole: Frequent: Accidental injury, asthenia. Infrequent: Chest pain, flank pain, malaise, allergic reaction, face edema, neck rigidity. Rare: Lupus erythematosus.
Cardiovascular: Infrequent: Palpitation, tachycardia, vascular insufficiency, hypotension, hypertension, thrombophlebitis, syncope, bradycardia. Rare: Atrial fibrillation, heart failure, pulmonary embolus, ventricular extrasystoles.
Digestive: Frequent: Vomiting. Infrequent: Flatulence, gingivitis, gum hyperplasia, gastritis, gastroenteritis, stomatitis, cholelithiasis, glossitis, melena, rectal hemorrhage, ulcerative stomatitis, gastro-duodenal ulcer, dysphagia, gum hemorrhage. Rare: Cholangitis, hematemesis, cholecystitis, cholestatic jaundice, colitis, duodenitis, esophagitis, fecal incontinence, mouth ulceration.
Hematologic and Lymphatic: Infrequent: Leukopenia, anemia, immunodeficiency, lymphadenopathy. Rare: Thrombocytopenia, microcytic anemia, petechia.
Metabolic and Nutritional: Infrequent: Peripheral edema, weight gain, edema, thirst, dehydration. Rare: Hypoglycemia, hyponatremia, lactic dehydrogenase increased, SGOT increased, SGPT increased.
Musculoskeletal: Infrequent: Leg cramps, myalgia, myasthenia, arthralgia, arthritis.
Nervous System: Frequent: Tremor, convulsion, abnormal gait, hyperesthesia, incoordination. Infrequent: Hypertonia, twitching, abnormal dreams, vertigo, libido decreased, neuropathy, hyperkinesia, movement disorder, dysarthria, cerebrovascular accident, hypotonia, peripheral neuritis, parathesia, reflexes increased. Rare: Circumoral paresthesia, dyskinesia, dystonia, encephalopathy, facial paralysis, hypokinesia, hyperesthesia, myoclonus, oculogyric crisis.
Behavioral Abnormalities--Non-Psychosis-Related: Infrequent: Euphoria.
Respiratory: Frequent: Pharyngitis, cough increased. Infrequent: Dyspnea. Rare: Apnea, hemoptysis.
Skin and Appendages: Frequent: Pruritus. Infrequent: Maculopapular rash, acne, alopecia, dry skin, sweating, eczema, urticaria, hirsutism, pustular rash, vesiculobullous rash.
Special Senses: Frequent: Ambylopia, tinnitus. Infrequent: Conjunctivitis, parosmia, deafness, visual field defect, glaucoma. Rare: Photophobia, iritis.
Urogenital: Infrequent: Urinary frequency, dysuria, urinary incontinence, hematuria, impotence, urinary retention, urinary urgency, amenorrhea, polyuria, nocturia. Rare: Albuminuria, enuresis, bladder pain, bladder calculus, gynecomastia, mastitis, menorrhagia.
DRUG ABUSE AND DEPENDENCE
The abuse and dependence potential of ZONEGRAN has not been evaluated in human studies (see WARNINGS, Cognitive/Neuropsychiatric Adverse Events subsection). In a series of animal studies, zonisamide did not demonstrate abuse liability and dependence potential. Monkeys did not self-administer zonisamide in a standard reinforcing paradigm. Rats exposed to zonisamide did not exhibit signs of physical dependence of the CNS-depressant type. Rats did not generalize the effects of diazepam to zonisamide in a standard discrimination paradigm after training, suggesting that zonisamide does not have abuse potential of the benzodiazepine-CNS depressant type.
OVERDOSAGE
Human Experience: Experience with ZONEGRAN daily doses over 800 mg/day is limited. During ZONEGRAN clinical development, three patients ingested unknown amounts of ZONEGRAN as suicide attempts, and all three were hospitalized with CNS symptoms. One patient became comatose and developed bradycardia, hypotension, and respiratory depression; the zonisamide plasma level was 100.1 µg/mL measured 31 hours post-ingestion. Zonisamide plasma levels fell with a half-life of 57 hours, and the patient became alert five days later.
Management: No specific antidotes for ZONEGRAN overdosage are available. Following a suspected recent overdose, emesis should be induced or gastric lavage performed with the usual precautions to protect the airway. General supportive care is indicated, including frequent monitoring of vital signs and close observation.
Zonisamide has a long half-life (see CLINICAL PHARMACOLOGY section). Due to the low protein binding of zonisamide (40%), renal dialysis may not be effective. A poison control center should be contacted for information on the management of ZONEGRAN overdosage.
DOSAGE AND ADMINISTRATION
ZONEGRAN (zonisamide) is recommended as adjunctive therapy for the treatment of partial seizures in adults. Safety and efficacy in pediatric patients below the age of 16 have not been established. ZONEGRAN should be administered once or twice daily, using 25 mg, 50 mg or 100 mg capsules. ZONEGRAN is given orally and can be taken with or without food. Capsules should be swallowed whole.
Adults over Age 16: The prescriber should be aware that, because of the long half-life of zonisamide, up to two weeks may be required to achieve steady state levels upon reaching a stable dose or following dosage adjustment. Although the regimen described below is one that has been shown to be tolerated, the prescriber may wish to prolong the duration of treatment at the lower doses in order to fully assess the effects of zonisamide at steady state, noting that many of the side effects of zonisamide are more frequent at doses of 300 mg per day and above. Although there is some evidence of greater response at doses above 100-200 mg/day, the increase appears small and formal dose-response studies have not been conducted.
The initial dose of ZONEGRAN should be 100 mg daily. After two weeks, the dose may be increased to 200 mg/day for at least two weeks. It can be increased to 300 mg/day and 400 mg/day, with the dose stable for at least two weeks to achieve steady state at each level. Evidence from controlled trials suggests that ZONEGRAN doses of 100-600 mg/day are effective, but there is no suggestion of increasing response above 400 mg/day (see CLINICAL PHARMACOLOGY, Clinical Studies subsection). There is little experience with doses greater than 600 mg/day.
Patients with Renal or Hepatic Disease: Because zonisamide is metabolized in the liver and excreted by the kidneys, patients with renal or hepatic disease should be treated with caution, and might require slower titration and more frequent monitoring (see CLINICAL PHARMACOLOGY and PRECAUTIONS ).
HOW SUPPLIED
ZONEGRAN is available as 25 mg, 50 mg and 100 mg two-piece hard gelatin capsules. The capsules are printed in black with "Eisai" and "ZONEGRAN 25," "ZONEGRAN 50," or "ZONEGRAN 100," respectively. ZONEGRAN is available in bottles of 100 with strengths and colors as follows:
Dosage StrengthCapsule ColorsNDC #25 mgWhite opaque body with white opaque cap.62856-681-1050 mgWhite opaque body with gray opaque cap.62856-682-10100 mgWhite opaque body with red opaque cap.62856-680-10
Store at 25°C (77°F), excursions permitted to 15-30° C (59-86°F) [see USP Controlled Room Temperature], in a dry place and protected from light.
US Patent #6,342,515
ANIMAL TOXICOLOGY
In dogs treated with zonisamide (10, 30, or 75 mg/kg/day) for 1 year, dark brown discoloration of the liver and concentric lamellar bodies in the cytoplasm of hepatocytes were observed in association with clinical chemistry changes indicative of liver damage (elevated alkaline phosphatase, gamma glutamyl transferase, and alanine amino transferase; decreased albumin) and altered drug metabolism at the highest dose, which is approximately 6 times the maximum recommended human dose (MRHD) of 400 mg/day on a mg/m 2 basis. Gross liver changes not clearly accompanied by biochemical evidence of hepatotoxicity were noted at 30 mg/kg/day, or approximately 2.4 times the MRHD on mg/m 2 basis. The no effect dose of 10 mg/kg/day is slightly less than the MRHD on mg/m 2 basis. The significance of these findings for humans is not known.
Manufactured by:
Elan Pharma International Ltd.
Distributed by:
Eisai Inc., Teaneck, NJ 07666
ZONEGRAN ® is a registered trademark of Dainippon Pharmaceutical Co. Ltd. and licensed exclusively to Eisai Inc.
© 2004 Eisai Inc.
200412
Revised December 2004
PATIENT INFORMATION LEAFLET
Questions and Answers about ZONEGRAN ® (zonisamide) capsules
What is the most important information I should know about ZONEGRAN?
Some people taking ZONEGRAN (ZO-nuh-gran) can get serious reactions. If you get any of the following symptoms, call your doctor right away:
- Rash (may be a sign of a dangerous condition)
- Fever, sore throat, sores in your mouth, or bruising easily (may be signs of a blood problem)
- Sudden back pain, abdominal (stomach area) pain, pain when urinating, bloody or dark urine (may be signs of a kidney stone)
- Decreased sweating or a rise in body temperature (especially in patients under 17 years old)
- Depression
- Thoughts that are unusual for you
- Speech or language problems
- Severe muscle pain and/or weakness
ZONEGRAN can cause drowsiness and coordination problems. Do not drive or operate dangerous machinery until you know how ZONEGRAN affects you.
What is ZONEGRAN?
ZONEGRAN is a medicine to treat partial seizures in adults. It is taken with other seizure medicines to help control your seizures.
Who should not take ZONEGRAN?
Talk to your doctor first before stopping ZONEGRAN.
Tell your doctor if you are allergic to sulfa drugs. Do not take ZONEGRAN if you are allergic to any sulfa drugs (for example, Bactrim™ or Septra®) or ZONEGRAN.
How should I take ZONEGRAN?
Be sure to follow your doctor's directions. Starting a new medicine can be confusing. If you have any questions, call your doctor.
ZONEGRAN is available as 25 mg, 50 mg, and 100 mg capsules. The usual recommended starting dose of ZONEGRAN is 100 mg each day. After a week or so, your doctor may increase your dose of ZONEGRAN. This may occur more than once. It is done to get the best control for your seizures. Take only the number of ZONEGRAN capsules you were told to take.
It is important to swallow ZONEGRAN capsules whole. Do not bite into or break the capsules. You may take ZONEGRAN with or without food.
Talk to your doctor about what to do if you miss a dose.
If you think you have overdosed on your medicine, call your local poison control center or emergency room right away.
Drink 6-8 glasses of water a day. This may help prevent kidney stones.
Talk to your doctor before stopping ZONEGRAN or any other seizure medicine. Stopping a seizure medicine all at once can cause status epilepticus, a serious problem.
What should I avoid while taking ZONEGRAN?
ZONEGRAN may make you drowsy. Do not drive a car or operate complex machinery until you know how ZONEGRAN may affect you.
Tell your doctor about any other medicines you may be taking, including non-prescription medicines.
Tell your doctor right away if you are pregnant or plan to become pregnant. You and your doctor can decide if the benefits of taking ZONEGRAN outweigh the risks. ZONEGRAN may cause birth defects.
It is not known whether ZONEGRAN is passed through breast milk to the baby. Before taking ZONEGRAN, tell your doctor if you are nursing or planning to nurse your baby.
What are the possible or reasonably likely side effects of ZONEGRAN?
The most common side effects are drowsiness, loss of appetite, dizziness, headache, nausea, agitation, and irritability. These side effects could occur at any time, but most often occur in the first 4 weeks.
Contact your doctor right away if:
- you develop skin rash
- your seizures worsen
- you develop signs of kidney stones (sudden back pain, abdominal pain, blood in your urine)
- you develop signs of a blood problem (fever, sore throat, sores in your mouth, or bruising easily)
- you get depressed
- you start having thoughts that are unusual for you
- you are very drowsy, have difficulty concentrating, or have coordination problems
- you develop speech or language problems
Other information about ZONEGRAN:
Medicines are sometimes prescribed for purposes other than those listed in a patient leaflet. Use ZONEGRAN only for the reason your doctor told you. Do not use it for another reason. Do not share your ZONEGRAN with others.
This is a summary of information about ZONEGRAN. Call your healthcare professional with any questions. Your doctor or pharmacist can give you the complete information about ZONEGRAN that is written for health professionals. You can also get information about ZONEGRAN at www.Eisai.com. You can get information and help from the Epilepsy Foundation at 800-EFA-1000 or www.efa.org.
Manufactured by:
Elan Pharma International Ltd.
Distributed by:
Eisai Inc., Teaneck, NJ 07666
ZONEGRAN ® is a registered trademark of Dainippon Pharmaceutical Co. Ltd. and licensed exclusively to Eisai Inc.
All other product names may be trademarks of the respective companies with which they are associated.
© 2004 Eisai Inc.
Subscribe to the "News" RSS Feed 
TOP ۞
