-
Avodart Soft Gelatin Capsules (Glaxosmithkline)
DESCRIPTION
AVODART (dutasteride) is a synthetic 4-azasteroid compound that is a selective inhibitor of both the type 1 and type 2 isoforms of steroid 5(alpha)-reductase (5AR), an intracellular enzyme that converts testosterone to 5(alpha)-dihydrotestosterone (DHT).
Dutasteride is chemically designated as (5(alpha),17(beta))-N-{2,5 bis(trifluoromethyl)phenyl}-3-oxo-4-azaandrost-1-ene-17-carboxamide. The empirical formula of dutasteride is C 27 H 30 F 6 N 2 O 2 , representing a molecular weight of 528.5.
Dutasteride is a white to pale yellow powder with a melting point of 242° to 250°C. It is soluble in ethanol (44 mg/mL), methanol (64 mg/mL), and polyethylene glycol 400 (3 mg/mL), but it is insoluble in water.
AVODART Soft Gelatin Capsules for oral administration contain 0.5 mg of the active ingredient dutasteride in yellow capsules with red print. Each capsule contains 0.5 mg of dutasteride dissolved in a mixture of mono-di-glycerides of caprylic/capric acid and butylated hydroxytoluene. The inactive excipients in the capsule shell are gelatin (from certified BSE-free bovine sources), glycerin, and ferric oxide (yellow). The soft gelatin capsules are printed with edible red ink.
CLINICAL PHARMACOLOGY
Pharmacodynamics: Mechanism of Action: Dutasteride inhibits the conversion of testosterone to 5(alpha)-dihydrotestosterone (DHT). DHT is the androgen primarily responsible for the initial development and subsequent enlargement of the prostate gland. Testosterone is converted to DHT by the enzyme 5(alpha)-reductase, which exists as 2 isoforms, type 1 and type 2. The type 2 isoenzyme is primarily active in the reproductive tissues, while the type 1 isoenzyme is also responsible for testosterone conversion in the skin and liver.
Dutasteride is a competitive and specific inhibitor of both type 1 and type 2 5(alpha)-reductase isoenzymes, with which it forms a stable enzyme complex. Dissociation from this complex has been evaluated under in vitro and in vivo conditions and is extremely slow. Dutasteride does not bind to the human androgen receptor.
Effect on 5(alpha)-Dihydrotestosterone and Testosterone: The maximum effect of daily doses of dutasteride on the reduction of DHT is dose dependent and is observed within 1 to 2 weeks. After 1 and 2 weeks of daily dosing with dutasteride 0.5 mg, median serum DHT concentrations were reduced by 85% and 90%, respectively. In patients with benign prostatic hyperplasia (BPH) treated with dutasteride 0.5 mg/day for 4 years, the median decrease in serum DHT was 94% at 1 year, 93% at 2 years, and 95% at both 3 and 4 years. The median increase in serum testosterone was 19% at both 1 and 2 years, 26% at 3 years, and 22% at 4 years, but the mean and median levels remained within the physiologic range.
In patients with BPH treated with 5 mg/day of dutasteride or placebo for up to 12 weeks prior to transurethral resection of the prostate, mean DHT concentrations in prostatic tissue were significantly lower in the dutasteride group compared with placebo (784 and 5,793 pg/g, respectively, p<0.001). Mean prostatic tissue concentrations of testosterone were significantly higher in the dutasteride group compared with placebo (2,073 and 93 pg/g, respectively, p<0.001).
Adult males with genetically inherited type 2 5(alpha)-reductase deficiency also have decreased DHT levels. These 5(alpha)-reductase deficient males have a small prostate gland throughout life and do not develop BPH. Except for the associated urogenital defects present at birth, no other clinical abnormalities related to 5(alpha)-reductase deficiency have been observed in these individuals.
Other Effects: Plasma lipid panel and bone mineral density were evaluated following 52 weeks of dutasteride 0.5 mg once daily in healthy volunteers. There was no change in bone mineral density as measured by dual energy x-ray absorptiometry (DEXA) compared with either placebo or baseline. In addition, the plasma lipid profile (i.e., total cholesterol, low density lipoproteins, high density lipoproteins, and triglycerides) was unaffected by dutasteride. No clinically significant changes in adrenal hormone responses to ACTH stimulation were observed in a subset population (n = 13) of the 1-year healthy volunteer study.
Pharmacokinetics: Absorption: Following administration of a single 0.5-mg dose of a soft gelatin capsule, time to peak serum concentrations (T max ) of dutasteride occurs within 2 to 3 hours. Absolute bioavailability in 5 healthy subjects is approximately 60% (range, 40% to 94%). When the drug is administered with food, the maximum serum concentrations were reduced by 10% to 15%. This reduction is of no clinical significance.
Distribution: Pharmacokinetic data following single and repeat oral doses show that dutasteride has a large volume of distribution (300 to 500 L). Dutasteride is highly bound to plasma albumin (99.0%) and alpha-1 acid glycoprotein (96.6%).
In a study of healthy subjects (n = 26) receiving dutasteride 0.5 mg/day for 12 months, semen dutasteride concentrations averaged 3.4 ng/mL (range, 0.4 to 14 ng/mL) at 12 months and, similar to serum, achieved steady-state concentrations at 6 months. On average, at 12 months 11.5% of serum dutasteride concentrations partitioned into semen.
Metabolism and Elimination: Dutasteride is extensively metabolized in humans. In vitro studies showed that dutasteride is metabolized by the CYP3A4 and CYP3A5 isoenzymes. Both of these isoenzymes produced the 4'-hydroxydutasteride, 6-hydroxydutasteride, and the 6,4'-dihydroxydutasteride metabolites. In addition, the 15-hydroxydutasteride metabolite was formed by CYP3A4. Dutasteride is not metabolized in vitro by human cytochrome P450 isoenzymes CYP1A2, CYP2A6, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, and CYP2E1. In human serum following dosing to steady state, unchanged dutasteride, 3 major metabolites (4'-hydroxydutasteride, 1,2-dihydrodutasteride, and 6-hydroxydutasteride), and 2 minor metabolites (6,4'-dihydroxydutasteride and 15-hydroxydutasteride), as assessed by mass spectrometric response, have been detected. The absolute stereochemistry of the hydroxyl additions in the 6 and 15 positions is not known. In vitro, the 4'-hydroxydutasteride and 1,2-dihydrodutasteride metabolites are much less potent than dutasteride against both isoforms of human 5AR. The activity of 6(beta)-hydroxydutasteride is comparable to that of dutasteride.
Dutasteride and its metabolites were excreted mainly in feces. As a percent of dose, there was approximately 5% unchanged dutasteride (~1% to ~15%) and 40% as dutasteride-related metabolites (~2% to ~90%). Only trace amounts of unchanged dutasteride were found in urine (<1%). Therefore, on average, the dose unaccounted for approximated 55% (range, 5% to 97%).
The terminal elimination half-life of dutasteride is approximately 5 weeks at steady state. The average steady-state serum dutasteride concentration was 40 ng/mL following 0.5 mg/day for 1 year. Following daily dosing, dutasteride serum concentrations achieve 65% of steady-state concentration after 1 month and approximately 90% after 3 months. Due to the long half-life of dutasteride, serum concentrations remain detectable (greater than 0.1 ng/mL) for up to 4 to 6 months after discontinuation of treatment.
Special Populations: Pediatric: Dutasteride pharmacokinetics have not been investigated in subjects younger than 18 years.
Geriatric: No dose adjustment is necessary in the elderly. The pharmacokinetics and pharmacodynamics of dutasteride were evaluated in 36 healthy male subjects aged between 24 and 87 years following administration of a single 5-mg dose of dutasteride. In this single-dose study, dutasteride half-life increased with age (approximately 170 hours in men aged 20 to 49 years, approximately 260 hours in men aged 50 to 69 years, and approximately 300 hours in men older than 70 years). Of 2,167 men treated with dutasteride in the 3 pivotal studies, 60% were age 65 and over and 15% were age 75 and over. No overall differences in safety or efficacy were observed between these patients and younger patients.
Gender: AVODART is not indicated for use in women (see WARNINGS and PRECAUTIONS ). The pharmacokinetics of dutasteride in women have not been studied.
Race: The effect of race on dutasteride pharmacokinetics has not been studied.
Renal Impairment: The effect of renal impairment on dutasteride pharmacokinetics has not been studied. However, less than 0.1% of a steady-state 0.5-mg dose of dutasteride is recovered in human urine, so no adjustment in dosage is anticipated for patients with renal impairment.
Hepatic Impairment: The effect of hepatic impairment on dutasteride pharmacokinetics has not been studied. Because dutasteride is extensively metabolized, exposure could be higher in hepatically impaired patients (see PRECAUTIONS : Use in Hepatic Impairment ).
Drug Interactions: In vitro drug metabolism studies reveal that dutasteride is metabolized by the human cytochrome P450 isoenzymes CYP3A4 and CYP3A5. In a human mass balance analysis (n = 8), dutasteride was extensively metabolized. Less than 20% of the dose was excreted unchanged in the feces. No clinical drug interaction studies have been performed to evaluate the impact of CYP3A enzyme inhibitors on dutasteride pharmacokinetics. However, based on the in vitro data, blood concentrations of dutasteride may increase in the presence of inhibitors of CYP3A4/5 such as ritonavir, ketoconazole, verapamil, diltiazem, cimetidine, troleandomycin, and ciprofloxacin. Dutasteride is not metabolized in vitro by human cytochrome P450 isoenzymes CYP1A2, CYP2A6, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, and CYP2E1.
Clinical drug interaction studies have shown no pharmacokinetic or pharmacodynamic interactions between dutasteride and tamsulosin, terazosin, warfarin, di-goxin, and cholestyramine (see PRECAUTIONS : Drug Interactions ).
Dutasteride does not inhibit the in vitro metabolism of model substrates for the major human cytochrome P450 isoenzymes (CYP1A2, CYP2C9, CYP2C19, CYP2D6, and CYP3A4) at a concentration of 1,000 ng/mL, 25 times greater than steady-state serum concentrations in humans.
CLINICAL STUDIES
Dutasteride 0.5 mg/day (n = 2,167) or placebo (n = 2,158) was evaluated in male subjects with BPH in three 2-year multicenter, placebo-controlled, double-blind studies, each with 2-year open-label extensions (n = 2,340). More than 90% of the study population was Caucasian. Subjects were at least 50 years of age with a serum prostate-specific antigen (PSA) >/=1.5 ng/mL and <10 ng/mL and BPH diagnosed by medical history and physical examination, including enlarged prostate (>/=30 cc) and BPH symptoms that were moderate to severe according to the American Urological Association Symptom Index (AUA-SI). Most of the 4,325 subjects randomly assigned to receive either dutasteride or placebo completed 2 years of double-blind treatment (70% and 67%, respectively). Most of the 2,340 subjects in the study extensions completed 2 additional years of open-label treatment (71%).
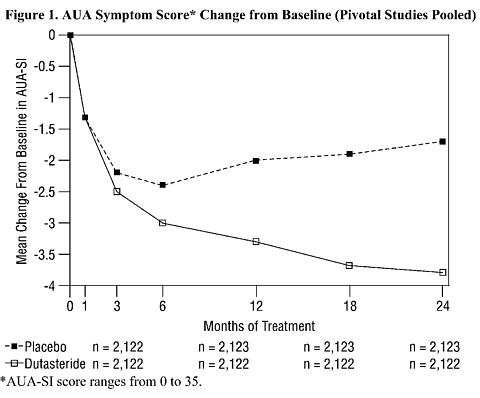
Effect on Symptom Scores: Symptoms were quantified using the AUA-SI, a questionnaire that evaluates urinary symptoms (incomplete emptying, frequency, intermittency, urgency, weak stream, straining, and nocturia) by rating on a 0 to 5 scale for a total possible score of 35. The baseline AUA-SI score across the 3 studies was approximately 17 units in both treatment groups.
Subjects receiving dutasteride achieved statistically significant improvement in symptoms versus placebo by Month 3 in one study and by Month 12 in the other 2 pivotal studies. At Month 12, the mean decrease from baseline in AUA-SI symptom scores across the 3 studies pooled was -3.3 units for dutasteride and -2.0 units for placebo with a mean difference between the 2 treatment groups of -1.3 (range, -1.1 to -1.5 units in each of the 3 studies, p<0.001) and was consistent across the 3 studies. At Month 24, the mean decrease from baseline was -3.8 units for dutasteride and -1.7 units for placebo with a mean difference of -2.1 (range, -1.9 to -2.2 units in each of the 3 studies, p<0.001). See Figure 1. The improvement in BPH symptoms seen during the first 2 years of double-blind treatment was maintained throughout an additional 2 years of open-label extension studies.
These studies were prospectively designed to evaluate effects on symptoms based on prostate size at baseline. In men with prostate volumes >/=40 cc, the mean decrease was -3.8 units for dutasteride and -1.6 units for placebo, with a mean difference between the 2 treatment groups of -2.2 at Month 24. In men with prostate volumes <40 cc, the mean decrease was -3.7 units for dutasteride and -2.2 units for placebo, with a mean difference between the 2 treatment groups of -1.5 at Month 24.
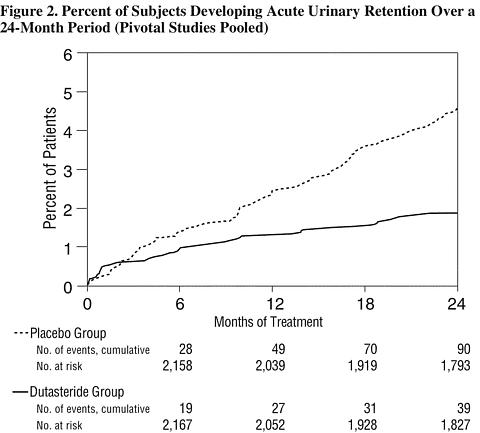
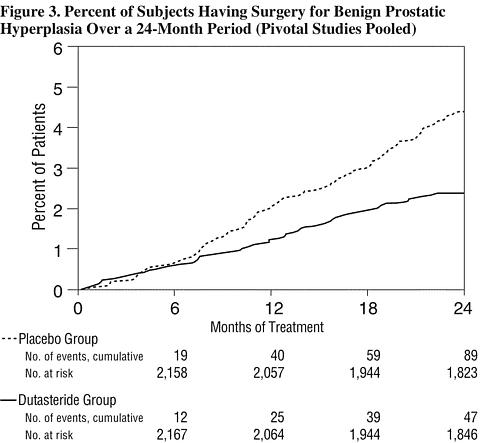
Effect on Acute Urinary Retention and the Need for Surgery: Efficacy was also assessed after 2 years of treatment by the incidence of acute urinary retention (AUR) requiring catheterization and BPH-related urological surgical intervention. Compared with placebo, AVODART was associated with a statistically significantly lower incidence of AUR (1.8% for AVODART vs. 4.2% for placebo, p<0.001; 57% reduction in risk, 95% CI: [38-71%]) and with a statistically significantly lower incidence of surgery (2.2% for AVODART vs. 4.1% for placebo, p<0.001; 48% reduction in risk, 95% CI: [26-63%]). See Figures 2 and 3.
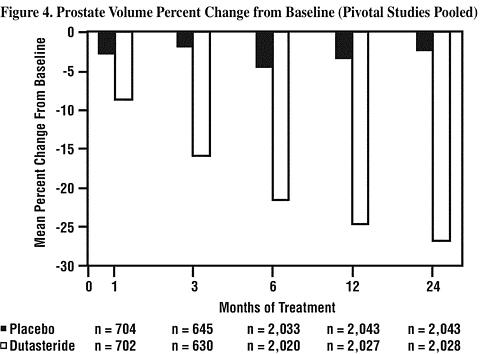
Effect on Prostate Volume: A prostate volume of at least 30 cc measured by transrectal ultrasound was required for study entry. The mean prostate volume at study entry was approximately 54 cc.
Statistically significant differences (dutasteride vs. placebo) were noted at the earliest post-treatment prostate volume measurement in each study (Month 1, Month 3, or Month 6) and continued through Month 24. At Month 12, the mean percent change in prostate volume across the 3 studies pooled was -24.7% for dutasteride and -3.4% for placebo; the mean difference (dutasteride minus placebo) was -21.3% (range, -21.0% to -21.6% in each of the 3 studies, p<0.001). At Month 24, the mean percent change in prostate volume across the 3 studies pooled was -26.7% for dutasteride and -2.2% for placebo with a mean difference of -24.5% (range, -24.0% to -25.1% in each of the 3 studies, p<0.001). See Figure 4. The reduction in prostate volume seen during the first 2 years of double-blind treatment was maintained throughout an additional 2 years of open-label extension studies.
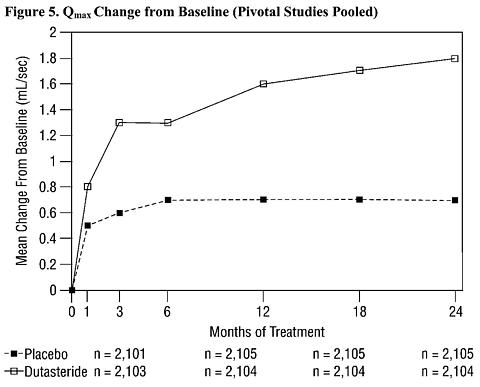
Effect on Maximum Urine Flow Rate: A mean peak urine flow rate (Q max ) of </=15 mL/sec was required for study entry. Q max was approximately 10 mL/sec at baseline across the 3 pivotal studies.
Differences between the 2 groups were statistically significant from baseline at Month 3 in all 3 studies and were maintained through Month 12. At Month 12, the mean increase in Q max across the 3 studies pooled was 1.6 mL/sec for dutasteride and 0.7 mL/sec for placebo; the mean difference (dutasteride minus placebo) was 0.8 mL/sec (range, 0.7 to 1.0 mL/sec in each of the 3 studies, p<0.001). At Month 24, the mean increase in Q max was 1.8 mL/sec for dutasteride and 0.7 mL/sec for placebo, with a mean difference of 1.1 mL/sec (range, 1.0 to 1.2 mL/sec in each of the 3 studies, p<0.001). See Figure 5. The increase in maximum urine flow rate seen during the first 2 years of double-blind treatment was maintained throughout an additional 2 years of open-label extension studies.
Summary of Clinical Studies: Data from 3 large, well-controlled efficacy studies demonstrate that treatment with AVODART (0.5 mg once daily) reduces the risk of both AUR and BPH-related surgical intervention relative to placebo, improves BPH-related symptoms, decreases prostate volume, and increases maximum urinary flow rates. These data suggest that AVODART arrests the disease process of BPH in men with an enlarged prostate.
INDICATIONS AND USAGE
AVODART is indicated for the treatment of symptomatic benign prostatic hyperplasia (BPH) in men with an enlarged prostate to:
- Improve symptoms
- Reduce the risk of acute urinary retention
- Reduce the risk of the need for BPH-related surgery
CONTRAINDICATIONS
AVODART is contraindicated for use in women and children.
AVODART is contraindicated for patients with known hypersensitivity to dutasteride, other 5(alpha)-reductase inhibitors, or any component of the preparation.
WARNINGS
Exposure of Women--Risk to Male Fetus: Dutasteride is absorbed through the skin. Therefore, women who are pregnant or may be pregnant should not handle AVODART Soft Gelatin Capsules because of the possibility of absorption of dutasteride and the potential risk of a fetal anomaly to a male fetus (see CONTRAINDICATIONS ). In addition, women should use caution whenever handling AVODART Soft Gelatin Capsules. If contact is made with leaking capsules, the contact area should be washed immediately with soap and water.
PRECAUTIONS
General: Lower urinary tract symptoms of BPH can be indicative of other urological diseases, including prostate cancer. Patients should be assessed to rule out other urological diseases prior to treatment with AVODART. Patients with a large residual urinary volume and/or severely diminished urinary flow may not be good candidates for 5(alpha)-reductase inhibitor therapy and should be carefully monitored for obstructive uropathy.
Blood Donation: Men being treated with dutasteride should not donate blood until at least 6 months have passed following their last dose. The purpose of this deferred period is to prevent administration of dutasteride to a pregnant female transfusion recipient.
Use in Hepatic Impairment: The effect of hepatic impairment on dutasteride pharmacokinetics has not been studied. Because dutasteride is extensively metabolized and has a half-life of approximately 5 weeks at steady state, caution should be used in the administration of dutasteride to patients with liver disease.
Use with Potent CYP3A4 Inhibitors: Although dutasteride is extensively metabolized, no metabolically based drug interaction studies have been conducted. The effect of potent CYP3A4 inhibitors has not been studied. Because of the potential for drug-drug interactions, care should be taken when administering dutasteride to patients taking potent, chronic CYP3A4 enzyme inhibitors (e.g., ritonavir).
Effects on Prostate-Specific Antigen and Prostate Cancer Detection: Digital rectal examinations, as well as other evaluations for prostate cancer, should be performed on patients with BPH prior to initiating therapy with AVODART and periodically thereafter.
Dutasteride reduces total serum PSA concentration by approximately 40% following 3 months of treatment and approximately 50% following 6, 12, and 24 months of treatment. This decrease is predictable over the entire range of PSA values, although it may vary in individual patients. Therefore, for interpretation of serial PSAs in a man taking AVODART, a new baseline PSA concentration should be established after 3 to 6 months of treatment, and this new value should be used to assess potentially cancer-related changes in PSA. To interpret an isolated PSA value in a man treated with AVODART for 6 months or more, the PSA value should be doubled for comparison with normal values in untreated men.
The free-to-total PSA ratio (percent free PSA) remains constant at Month 12, even under the influence of AVODART. If clinicians elect to use percent free PSA as an aid in the detection of prostate cancer in men receiving AVODART, no adjustment to its value appears necessary.
Information for Patients: Physicians should instruct their patients to read the Patient Information leaflet before starting therapy with AVODART and to reread it upon prescription renewal for new information regarding the use of AVODART.
AVODART Soft Gelatin Capsules should not be handled by a woman who is pregnant or who may become pregnant because of the potential for absorption of dutasteride and the subsequent potential risk to a developing male fetus (see CONTRAINDICATIONS and WARNINGS : Exposure of Women--Risk to Male Fetus ).
Physicians should inform patients that ejaculate volume might be decreased in some patients during treatment with AVODART. This decrease does not appear to interfere with normal sexual function. In clinical trials, impotence and decreased libido, considered by the investigator to be drug-related, occurred in a small number of patients treated with AVODART or placebo (see ADVERSE REACTIONS : Table 1).
Men treated with dutasteride should not donate blood until at least 6 months have passed following their last dose to prevent pregnant women from receiving dutasteride through blood transfusion (see PRECAUTIONS : Blood Donation ).
Drug Interactions: Care should be taken when administering dutasteride to patients taking potent, chronic CYP3A4 inhibitors (see PRECAUTIONS : Use with Potent CYP3A4 Inhibitors ).
Dutasteride does not inhibit the in vitro metabolism of model substrates for the major human cytochrome P450 isoenzymes (CYP1A2, CYP2C9, CYP2C19, CYP2D6, and CYP3A4) at a concentration of 1,000 ng/mL, 25 times greater than steady-state serum concentrations in humans. In vitro studies demonstrate that dutasteride does not displace warfarin, diazepam, or phenytoin from plasma protein binding sites, nor do these model compounds displace dutasteride.
Digoxin: In a study of 20 healthy volunteers, AVODART did not alter the steady-state pharmacokinetics of digoxin when administered concomitantly at a dose of 0.5 mg/day for 3 weeks.
Warfarin: In a study of 23 healthy volunteers, 3 weeks of treatment with AVODART 0.5 mg/day did not alter the steady-state pharmacokinetics of the S- or R-warfarin isomers or alter the effect of warfarin on prothrombin time when administered with warfarin.
Alpha-Adrenergic Blocking Agents: In a single sequence, crossover study in healthy volunteers, the administration of tamsulosin or terazosin in combination with AVODART had no effect on the steady-state pharmacokinetics of either alpha-adrenergic blocker. The percent change in DHT concentrations was similar for AVODART alone compared with the combination treatment.
A clinical trial was conducted in which dutasteride and tamsulosin were administered concomitantly for 24 weeks followed by 12 weeks of treatment with either the dutasteride and tamsulosin combination or dutasteride monotherapy. Results from the second phase of the trial revealed no excess of serious adverse events or discontinuations due to adverse events in the combination group compared to the dutasteride monotherapy group.
Calcium Channel Antagonists: In a population pharmacokinetics analysis, a decrease in clearance of dutasteride was noted when co-administered with the CYP3A4 inhibitors verapamil (-37%, n = 6) and diltiazem (-44%, n = 5). In contrast, no decrease in clearance was seen when amlodipine, another calcium channel antagonist that is not a CYP3A4 inhibitor, was co-administered with dutasteride (+7%, n = 4).
The decrease in clearance and subsequent increase in exposure to dutasteride in the presence of verapamil and diltiazem is not considered to be clinically significant. No dose adjustment is recommended.
Cholestyramine: Administration of a single 5-mg dose of AVODART followed 1 hour later by 12 g cholestyramine did not affect the relative bioavailability of dutasteride in 12 normal volunteers.
Other Concomitant Therapy: Although specific interaction studies were not performed with other compounds, approximately 90% of the subjects in the 3 Phase III pivotal efficacy studies receiving AVODART were taking other medications concomitantly. No clinically significant adverse interactions could be attributed to the combination of AVODART and concurrent therapy when AVODART was co-administered with anti-hyperlipidemics, angiotensin-converting enzyme (ACE) inhibitors, beta-adrenergic blocking agents, calcium channel blockers, corticosteroids, diuretics, nonsteroidal anti-inflammatory drugs (NSAIDs), phosphodiesterase Type V inhibitors, and quinolone antibiotics.
Drug/Laboratory Test Interactions: Effects on Prostate-Specific Antigen: PSA levels generally decrease in patients treated with AVODART as the prostate volume decreases. In approximately one-half of the subjects, a 20% decrease in PSA is seen within the first month of therapy. After 6 months of therapy, PSA levels stabilize to a new baseline that is approximately 50% of the pre-treatment value. Results of subjects treated with AVODART for up to 2 years indicate this 50% reduction in PSA is maintained. Therefore, a new baseline PSA concentration should be established after 3 to 6 months of treatment with AVODART (see PRECAUTIONS : Effects on PSA and Prostate Cancer Detection ).
Hormone Levels: In healthy volunteers, 52 weeks of treatment with dutasteride 0.5 mg/day (n = 26) resulted in no clinically significant change compared with placebo (n = 23) in sex hormone binding globulin, estradiol, luteinizing hormone, follicle-stimulating hormone, thyroxine (free T4), and dehydroepiandrosterone. Statistically significant, baseline-adjusted mean increases compared with placebo were observed for total testosterone at 8 weeks (97.1 ng/dL, p<0.003) and thyroid-stimulating hormone (TSH) at 52 weeks (0.4 mcIU/mL, p<0.05). The median percentage changes from baseline within the dutasteride group were 17.9% for testosterone at 8 weeks and 12.4% for TSH at 52 weeks. After stopping dutasteride for 24 weeks, the mean levels of testosterone and TSH had returned to baseline in the group of subjects with available data at the visit. In patients with BPH treated with dutasteride 0.5 mg/day for 4 years, the median decrease in serum DHT was 94% at 1 year, 93% at 2 years, and 95% at both 3 and 4 years. The median increase in serum testosterone was 19% at both 1 and 2 years, 26% at 3 years, and 22% at 4 years, but the mean and median levels remained within the physiologic range. In patients with BPH treated with dutasteride in a large Phase III trial, there was a median percent increase in luteinizing hormone of 12% at 6 months and 19% at both 12 and 24 months.
Reproductive Function: The effects of dutasteride 0.5 mg/day on semen characteristics were evaluated in normal volunteers aged 18 to 52 (n = 27 dutasteride, n = 23 placebo) throughout 52 weeks of treatment and 24 weeks of post-treatment follow-up. At 52 weeks, the mean percent reduction from baseline in total sperm count, semen volume, and sperm motility were 23%, 26%, and 18%, respectively, in the dutasteride group when adjusted for changes from baseline in the placebo group. Sperm concentration and sperm morphology were unaffected. After 24 weeks of follow-up, the mean percent change in total sperm count in the dutasteride group remained 23% lower than baseline. While mean values for all semen parameters at all time points remained within the normal ranges and did not meet predefined criteria for a clinically significant change (30%), two subjects in the dutasteride group had decreases in sperm count of greater than 90% from baseline at 52 weeks, with partial recovery at the 24-week follow-up. The clinical significance of dutasteride's effect on semen characteristics for an individual patient's fertility not known.
Central Nervous System Toxicity: In rats and dogs, repeated oral administration of dutasteride resulted in some animals showing signs of non-specific, reversible, centrally-mediated toxicity without associated histopathological changes at exposure 425- and 315-fold the expected clinical exposure (of parent drug), respectively.
Carcinogenesis, Mutagenesis, Impairment of Fertility: Carcinogenesis: A 2-year carcinogenicity study was conducted in B6C3F1 mice at doses of 3, 35, 250, and 500 mg/kg/day for males and 3, 35, and 250 mg/kg/day for females; an increased incidence of benign hepatocellular adenomas was noted at 250 mg/kg/day (290-fold the expected clinical exposure to a 0.5 mg daily dose) in females only. Two of the 3 major human metabolites have been detected in mice. The exposure to these metabolites in mice is either lower than in humans or is not known.
In a 2-year carcinogenicity study in Han Wistar rats, at doses of 1.5, 7.5, and 53 mg/kg/day for males and 0.8, 6.3, and 15 mg/kg/day for females, there was an increase in Leydig cell adenomas in the testes at 53 mg/kg/day (135-fold the expected clinical exposure). An increased incidence of Leydig cell hyperplasia was present at 7.5 mg/kg/day (52-fold the expected clinical exposure) and 53 mg/kg/day in male rats. A positive correlation between proliferative changes in the Leydig cells and an increase in circulating luteinizing hormone levels has been demonstrated with 5(alpha)-reductase inhibitors and is consistent with an effect on the hypothalamic-pituitary-testicular axis following 5(alpha)-reductase inhibition. At tumorigenic doses in rats, luteinizing hormone levels in rats were increased by 167%. In this study, the major human metabolites were tested for carcinogenicity at approximately 1 to 3 times the expected clinical exposure.
Mutagenesis: Dutasteride was tested for genotoxicity in a bacterial mutagenesis assay (Ames test), a chromosomal aberration assay in CHO cells, and a micronucleus assay in rats. The results did not indicate any genotoxic potential of the parent drug. Two major human metabolites were also negative in either the Ames test or an abbreviated Ames test.
Impairment of Fertility: Treatment of sexually mature male rats with dutasteride at doses of 0.05, 10, 50, and 500 mg/kg/day (0.1- to 110-fold the expected clinical exposure of parent drug) for up to 31 weeks resulted in dose- and time-dependent decreases in fertility; reduced cauda epididymal (absolute) sperm counts but not sperm concentration (at 50 and 500 mg/kg/day); reduced weights of the epididymis, prostate, and seminal vesicles; and microscopic changes in the male reproductive organs. The fertility effects were reversed by recovery week 6 at all doses, and sperm counts were normal at the end of a 14-week recovery period. The 5(alpha)-reductase-related changes consisted of cytoplasmic vacuolation of tubular epithelium in the epididymides and decreased cytoplasmic content of epithelium, consistent with decreased secretory activity in the prostate and seminal vesicles. The microscopic changes were no longer present at recovery week 14 in the low-dose group and were partly recovered in the remaining treatment groups. Low levels of dutasteride (0.6 to 17 ng/mL) were detected in the serum of untreated female rats mated to males dosed at 10, 50, or 500 mg/kg/day for 29 to 30 weeks.
In a fertility study in female rats, oral administration of dutasteride at doses of 0.05, 2.5, 12.5, and 30 mg/kg/day resulted in reduced litter size, increased embryo resorption and feminization of male fetuses (decreased anogenital distance) at doses of >/=2.5 mg/kg/day (2- to 10-fold the clinical exposure of parent drug in men). Fetal body weights were also reduced at >/=0.05 mg/kg/day in rats (<0.02-fold the human exposure).
Pregnancy: Pregnancy Category X (see CONTRAINDICATIONS ). AVODART is contraindicated for use in women. AVODART has not been studied in women because preclinical data suggest that the suppression of circulating levels of dihydrotestosterone may inhibit the development of the external genital organs in a male fetus carried by a woman exposed to dutasteride.
In an intravenous embryo-fetal development study in the rhesus monkey (12/group), administration of dutasteride at 400, 780, 1,325, or 2,010 ng/day on gestation days 20 to 100 did not adversely affect development of male external genitalia. Reduction of fetal adrenal weights, reduction in fetal prostate weights, and increases in fetal ovarian and testis weights were observed in monkeys treated with the highest dose. Based on the highest measured semen concentration of dutasteride in treated men (14 ng/mL), these doses represent 0.8 to 16 times based on blood levels of parent drug (32 to 186 times based on a ng/kg daily dose) the potential maximum exposure of a 50-kg human female to 5 mL semen daily from a dutasteride-treated man, assuming 100% absorption. Dutasteride is highly bound to proteins in human semen (>96%), potentially reducing the amount of dutasteride available for vaginal absorption.
In an embryo-fetal development study in female rats, oral administration of dutasteride at doses of 0.05, 2.5, 12.5, and 30 mg/kg/day resulted in feminization of male fetuses (decreased anogenital distance) and male offspring (nipple development, hypospadias, and distended preputial glands) at all doses (0.07- to 111-fold the expected male clinical exposure). An increase in stillborn pups was observed at 30 mg/kg/day, and reduced fetal body weight was observed at doses >/=2.5 mg/kg/day (15- to 111-fold the expected clinical exposure). Increased incidences of skeletal variations considered to be delays in ossification associated with reduced body weight were observed at doses of 12.5 and 30 mg/kg/day (56- to 111-fold the expected clinical exposure).
In an oral pre- and post-natal development study in rats, dutasteride doses of 0.05, 2.5, 12.5, or 30 mg/kg/day were administered. Unequivocal evidence of feminization of the genitalia (i.e., decreased anogenital distance, increased incidence of hypospadias, nipple development) of F1 generation male offspring occurred at doses >/=2.5 mg/kg/day (14- to 90-fold the expected clinical exposure in men). At a daily dose of 0.05 mg/kg/day (0.05-fold the expected clinical exposure), evidence of feminization was limited to a small, but statistically significant, decrease in anogenital distance. Doses of 2.5 to 30 mg/kg/day resulted in prolonged gestation in the parental females and a decrease in time to vaginal patency for female offspring and decrease prostate and seminal vesicle weights in male offspring. Effects on newborn startle response were noted at doses greater than or equal to 12.5 mg/kg/day. Increased stillbirths were noted at 30 mg/kg/day.
Feminization of male fetuses is an expected physiological consequence of inhibition of the conversion of testosterone to DHT by 5(alpha)-reductase inhibitors. These results are similar to observations in male infants with genetic 5(alpha)-reductase deficiency.
In the rabbit, embryo-fetal study doses of 30, 100, and 200 mg/kg (28- to 93-fold the expected clinical exposure in men) were administered orally on days 7 to 29 of pregnancy to encompass the late period of external genitalia development. Histological evaluation of the genital papilla of fetuses revealed evidence of feminization of the male fetus at all doses. A second embryo-fetal study in rabbits at doses of 0.05, 0.4, 3.0, and 30 mg/kg/day (0.3- to 53-fold the expected clinical exposure) also produced evidence of feminization of the genitalia in male fetuses at all doses. It is not known whether rabbits or rhesus monkeys produce any of the major human metabolites.
Nursing Mothers: AVODART is not indicated for use in women. It is not known whether dutasteride is excreted in human breast milk.
Pediatric Use: AVODART is not indicated for use in the pediatric population. Safety and effectiveness in the pediatric population have not been established.
Geriatric Use: Of 2,167 male subjects treated with AVODART in 3 clinical studies, 60% were 65 and over and 15% were 75 and over. No overall differences in safety or efficacy were observed between these subjects and younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients.
ADVERSE REACTIONS
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trial of another drug and may not reflect the rates observed in practice. The adverse reaction information from clinical trials does, however, provide a basis for identifying the adverse events that appear to be related to drug use and for approximating rates.
Most adverse reactions were mild or moderate and generally resolved while on treatment in both the AVODART and placebo groups. The most common adverse events leading to withdrawal in both treatment groups were associated with the reproductive system.
Over 4,300 male subjects with BPH were randomly assigned to receive placebo or 0.5-mg daily doses of AVODART in 3 identical 2-year, placebo-controlled, double-blind, Phase 3 treatment studies, each with 2-year open-label extensions. During the double-blind treatment period, 2,167 male subjects were exposed to AVODART, including 1,772 exposed for 1 year and 1,510 exposed for 2 years. When including the open-label extensions, 1,009 male subjects were exposed to AVODART for 3 years and 812 were exposed for 4 years. The population was aged 47 to 94 years (mean age, 66 years) and greater than 90% Caucasian. Over the 2-year double-blind treatment period, 376 subjects (9% of each treatment group) were withdrawn from the studies due to adverse experiences, most commonly associated with the reproductive system, with similar findings during the 2-year open-label extensions. Withdrawals due to adverse events considered by the investigator to have a reasonable possibility of being caused by the study medication occurred in 4% of the subjects receiving AVODART and in 3% of the subjects receiving placebo. Table 1 summarizes clinical adverse reactions that were reported by the investigator as drug-related in at least 1% of subjects receiving AVODART and at a higher incidence than subjects receiving placebo.
Table 1. Drug-Related Adverse Events * Reported in >/=1% Subjects Over a 24-Month Period and More Frequently in the Dutasteride Group Than the Placebo Group (Pivotal Studies Pooled)Adverse Events
Dutasteride (n)
Placebo (n)Adverse Event Onset Month 0-6
(n = 2,167)
(n = 2,158)Month 7-12
(n = 1,901)
(n = 1,922)Month 13-18
(n = 1,725)
(n = 1,714)Month 19-24
(n = 1,605)
(n = 1,555)ImpotenceDutasteride4.7% 1.4% 1.0% 0.8% Placebo1.7% 1.5% 0.5% 0.9% Decreased libidoDutasteride3.0% 0.7% 0.3% 0.3% Placebo1.4% 0.6% 0.2% 0.1% Ejaculation disorderDutasteride1.4% 0.5% 0.5% 0.1% Placebo0.5% 0.3% 0.1% 0.0% Gynecomastia **/*Dutasteride0.5% 0.8% 1.1% 0.6% Placebo0.2% 0.3% 0.3% 0.1% * A drug-related adverse event is one considered by the investigator to have a reasonable possibility of being caused by the study medication. In assessing causality, investigators were asked to select from 1 of 2 options: reasonably related to study medication or unrelated to study medication.**/* Includes breast tenderness and breast enlargement.Long-Term Treatment (Up to 4 Years): There is no evidence of increased drug-related sexual adverse events (impotence, decreased libido and ejaculation disorder) or gynecomastia with increased duration of treatment. The relationship between long-term use of dutasteride and male breast neoplasia is currently unknown.
Postmarketing Experience: The following adverse reactions have been identified during postapproval use of AVODART. Because these reactions are reported voluntarily from a population of uncertain size, it is not possible to reliably estimate their frequency or establish a causal relationship to drug exposure. Decisions to include these reactions in labeling are based on one or more of the following factors: (1) seriousness of the reaction, (2) frequency of reporting, or (3) potential causal connection to AVODART.
- allergic reactions, including rash, pruritus, urticaria, and localized edema.
OVERDOSAGE
In volunteer studies, single doses of dutasteride up to 40 mg (80 times the therapeutic dose) for 7 days have been administered without significant safety concerns. In a clinical study, daily doses of 5 mg (10 times the therapeutic dose) were administered to 60 subjects for 6 months with no additional adverse effects to those seen at therapeutic doses of 0.5 mg.
There is no specific antidote for dutasteride. Therefore, in cases of suspected overdosage symptomatic and supportive treatment should be given as appropriate, taking the long half-life of dutasteride into consideration.
DOSAGE AND ADMINISTRATION
The recommended dose of AVODART is 1 capsule (0.5 mg) taken orally once a day. The capsules should be swallowed whole. AVODART may be administered with or without food.
No dosage adjustment is necessary for subjects with renal impairment or for the elderly (see CLINICAL PHARMACOLOGY : Pharmacokinetics : Special Populations : Geriatric and Renal Impairment ). Due to the absence of data in patients with hepatic impairment, no dosage recommendation can be made (see PRECAUTIONS : General ).
HOW SUPPLIED
AVODART Soft Gelatin Capsules 0.5 mg are oblong, opaque, dull yellow, gelatin capsules imprinted with "GX CE2" in red ink on one side packaged in bottles of 30 (NDC 0173-0712-15) and 90 (NDC 0173-0712-04) with child-resistant closures.
Storage and Handling: Store at 25°C (77°F); excursions permitted to 15-30°C (59-86°F) [see USP Controlled Room Temperature].
Dutasteride is absorbed through the skin. AVODART Soft Gelatin capsules should not be handled by women who are pregnant or who may become pregnant because of the potential for absorption of dutasteride and the subsequent potential risk to a developing male fetus (see CLINICAL PHARMACOLOGY : Pharmacokinetics , WARNINGS : Exposure of Women--Risk to Male Fetus , and PRECAUTIONS : Information for Patients and Pregnancy ).
Manufactured by Cardinal Health
Beinheim, France for
Glaxosmithkline, Research Triangle Park, NC 27709
©2005, Glaxosmithkline. All rights reserved.
May 2005/RL-2188
Subscribe to the "News" RSS Feed 
TOP ۞
