-
Benicar Tablets (Sankyo)
USE IN PREGNANCY
When used in pregnancy during the second and third trimesters, drugs that act directly on the renin-angiotensin system can cause injury and even death to the developing fetus. When pregnancy is detected, BENICAR® should be discontinued as soon as possible. See WARNINGS , Fetal/Neonatal Morbidity and Mortality .
DESCRIPTION
BENICAR® (olmesartan medoxomil), a prodrug, is hydrolyzed to olmesartan during absorption from the gastrointestinal tract. Olmesartan is a selective AT 1 subtype angiotensin II receptor antagonist.
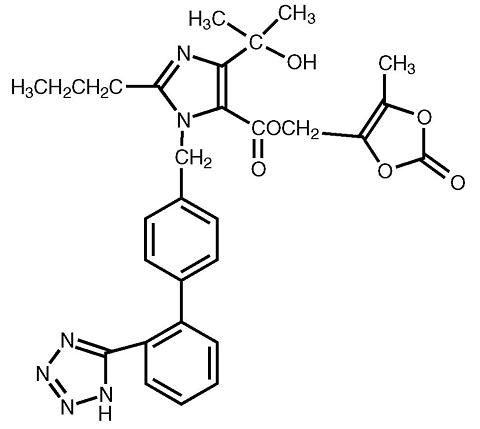
Olmesartan medoxomil is described chemically as 2,3-dihydroxy-2-butenyl 4-(1-hydroxy-1-methylethyl)-2-propyl-1-[ p -( o -1 H -tetrazol-5-ylphenyl)benzyl]imidazole-5-carboxylate, cyclic 2,3-carbonate.
Its empirical formula is C 29 H 30 N 6 O 6 and its structural formula is:
Olmesartan medoxomil is a white to light yellowish-white powder or crystalline powder with a molecular weight of 558.59. It is practically insoluble in water and sparingly soluble in methanol. BENICAR® is available for oral use as film-coated tablets containing 5 mg, 20 mg, or 40 mg of olmesartan medoxomil and the following inactive ingredients: hydroxypropylcellulose, lactose, low-substituted hydroxypropylcellulose, magnesium stearate, microcrystalline cellulose, talc, titanium dioxide, and (5 mg only) yellow iron oxide.
CLINICAL PHARMACOLOGY
Mechanism of Action
Angiotensin II is formed from angiotensin I in a reaction catalyzed by angiotensin converting enzyme (ACE, kininase II). Angiotensin II is the principal pressor agent of the renin-angiotensin system, with effects that include vasoconstriction, stimulation of synthesis and release of aldosterone, cardiac stimulation and renal reabsorption of sodium. Olmesartan blocks the vasoconstrictor effects of angiotensin II by selectively blocking the binding of angiotensin II to the AT 1 receptor in vascular smooth muscle. Its action is, therefore, independent of the pathways for angiotensin II synthesis.
An AT 2 receptor is found also in many tissues, but this receptor is not known to be associated with cardiovascular homeostasis. Olmesartan has more than a 12,500-fold greater affinity for the AT 1 receptor than for the AT 2 receptor.
Blockade of the renin-angiotensin system with ACE inhibitors, which inhibit the biosynthesis of angiotensin II from angiotensin I, is a mechanism of many drugs used to treat hypertension. ACE inhibitors also inhibit the degradation of bradykinin, a reaction also catalyzed by ACE. Because olmesartan medoxomil does not inhibit ACE (kininase II), it does not affect the response to bradykinin. Whether this difference has clinical relevance is not yet known.
Blockade of the angiotensin II receptor inhibits the negative regulatory feedback of angiotensin II on renin secretion, but the resulting increased plasma renin activity and circulating angiotensin II levels do not overcome the effect of olmesartan on blood pressure.
Pharmacokinetics
General
Olmesartan medoxomil is rapidly and completely bioactivated by ester hydrolysis to olmesartan during absorption from the gastrointestinal tract. Olmesartan appears to be eliminated in a biphasic manner with a terminal elimination half-life of approximately 13 hours. Olmesartan shows linear pharmacokinetics following single oral doses of up to 320 mg and multiple oral doses of up to 80 mg. Steady-state levels of olmesartan are achieved within 3 to 5 days and no accumulation in plasma occurs with once-daily dosing.
The absolute bioavailability of olmesartan is approximately 26%. After oral administration, the peak plasma concentration (C max ) of olmesartan is reached after 1 to 2 hours. Food does not affect the bioavailability of olmesartan.
Metabolism and Excretion
Following the rapid and complete conversion of olmesartan medoxomil to olmesartan during absorption, there is virtually no further metabolism of olmesartan. Total plasma clearance of olmesartan is 1.3 L/h, with a renal clearance of 0.6 L/h. Approximately 35% to 50% of the absorbed dose is recovered in urine while the remainder is eliminated in feces via the bile.
Distribution
The volume of distribution of olmesartan is approximately 17 L. Olmesartan is highly bound to plasma proteins (99%) and does not penetrate red blood cells. The protein binding is constant at plasma olmesartan concentrations well above the range achieved with recommended doses.
In rats, olmesartan crossed the blood-brain barrier poorly, if at all. Olmesartan passed across the placental barrier in rats and was distributed to the fetus. Olmesartan was distributed to milk at low levels in rats.
Special Populations
Pediatric: The pharmacokinetics of olmesartan have not been investigated in patients <18 years of age.
Geriatrics: The pharmacokinetics of olmesartan were studied in the elderly (>/=65 years). Overall, maximum plasma concentrations of olmesartan were similar in young adults and the elderly. Modest accumulation of olmesartan was observed in the elderly with repeated dosing; AUC ss, [tgr ] was 33% higher in elderly patients, corresponding to an approximate 30% reduction in CL R .
Gender: Minor differences were observed in the pharmacokinetics of olmesartan in women compared to men. AUC and C max were 10-15% higher in women than in men.
Renal Insufficiency: In patients with renal insufficiency, serum concentrations of olmesartan were elevated compared to subjects with normal renal function. After repeated dosing, the AUC was approximately tripled in patients with severe renal impairment (creatinine clearance <20 mL/min). The pharmacokinetics of olmesartan in patients undergoing hemodialysis has not been studied.
Hepatic Insufficiency: Increases in AUC 0-(infinity) and C max were observed in patients with moderate hepatic impairment compared to those in matched controls, with an increase in AUC of about 60%.
Drug Interactions: See PRECAUTIONS , Drug Interactions .
Pharmacodynamics
Olmesartan medoxomil doses of 2.5 to 40 mg inhibit the pressor effects of angiotensin I infusion. The duration of the inhibitory effect was related to dose, with doses of olmesartan medoxomil >40 mg giving >90% inhibition at 24 hours.
Plasma concentrations of angiotensin I and angiotensin II and plasma renin activity (PRA) increase after single and repeated administration of olmesartan medoxomil to healthy subjects and hypertensive patients. Repeated administration of up to 80 mg olmesartan medoxomil had minimal influence on aldosterone levels and no effect on serum potassium.
Clinical Trials
The antihypertensive effects of BENICAR® have been demonstrated in seven placebo-controlled studies at doses ranging from 2.5 to 80 mg for 6 to 12 weeks, each showing statistically significant reductions in peak and trough blood pressure. A total of 2693 patients (2145 BENICAR®; 548 placebo) with essential hypertension were studied. BENICAR® once daily (QD) lowered diastolic and systolic blood pressure. The response was dose-related, as shown in the following graph. An olmesartan medoxomil dose of 20 mg daily produces a trough sitting BP reduction over placebo of about 10/6 mm Hg and a dose of 40 mg daily produces a trough sitting BP reduction over placebo of about 12/7 mm Hg. Olmesartan medoxomil doses greater than 40 mg had little additional effect. The onset of the antihypertensive effect occurred within 1 week and was largely manifest after 2 weeks.
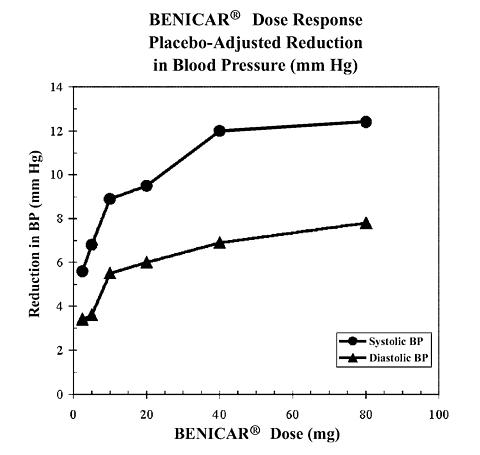
Data above are from seven placebo-controlled studies (2145 BENICAR® patients, 548 placebo patients). The blood pressure lowering effect was maintained throughout the 24-hour period with BENICAR® once daily, with trough-to-peak ratios for systolic and diastolic response between 60 and 80%.
The blood pressure lowering effect of BENICAR®, with and without hydrochlorothiazide, was maintained in patients treated for up to 1 year. There was no evidence of tachyphylaxis during long-term treatment with BENICAR® or rebound effect following abrupt withdrawal of olmesartan medoxomil after 1 year of treatment.
The antihypertensive effect of BENICAR® was similar in men and women and in patients older and younger than 65 years. The effect was smaller in black patients (usually a low-renin population), as has been seen with other ACE inhibitors, angiotensin receptor blockers and beta-blockers. BENICAR® had an additional blood pressure lowering effect when added to hydrochlorothiazide.
INDICATIONS AND USAGE
BENICAR® is indicated for the treatment of hypertension. It may be used alone or in combination with other antihypertensive agents.
CONTRAINDICATIONS
BENICAR® is contraindicated in patients who are hypersensitive to any component of this product.
WARNINGS
Fetal/Neonatal Morbidity and Mortality
Drugs that act directly on the renin-angiotensin system can cause fetal and neonatal morbidity and death when administered to pregnant women. Several dozen cases have been reported in the world literature of patients who were taking angiotensin converting enzyme inhibitors. When pregnancy is detected, BENICAR® should be discontinued as soon as possible.
The use of drugs that act directly on the renin-angiotensin system during the second and third trimesters of pregnancy has been associated with fetal and neonatal injury, including hypotension, neonatal skull hypoplasia, anuria, reversible or irreversible renal failure and death. Oligohydramnios has also been reported, presumably resulting from decreased fetal function; oligohydramnios in this setting has been associated with fetal limb contractures, craniofacial deformation and hypoplastic lung development. Prematurity, intrauterine growth retardation and patent ductus arteriosus have also been reported, although it is not clear whether these occurrences were due to exposure to the drug.
These adverse effects do not appear to have resulted from intrauterine drug exposure that has been limited to the first trimester. Mothers whose embryos and fetuses are exposed to an angiotensin II receptor antagonist only during the first trimester should be so informed. Nonetheless, when patients become pregnant, physicians should have the patient discontinue the use of BENICAR® as soon as possible.
Rarely (probably less often than once in every thousand pregnancies), no alternative to a drug acting on the renin-angiotensin system will be found. In these rare cases, the mothers should be apprised of the potential hazards to their fetuses and serial ultrasound examinations should be performed to assess the intra-amniotic environment.
If oligohydramnios is observed, BENICAR® should be discontinued unless it is considered life-saving for the mother. Contraction stress testing (CST), a nonstress test (NST) or biophysical profiling (BPP) may be appropriate, depending upon the week of pregnancy. Patients and physicians should be aware, however, that oligohydramnios may not appear until after the fetus has sustained irreversible injury.
Infants with histories of in utero exposure to an angiotensin II receptor antagonist should be closely observed for hypotension, oliguria and hyperkalemia. If oliguria occurs, attention should be directed toward support of blood pressure and renal perfusion. Exchange transfusion or dialysis may be required as means of reversing hypotension and/or substituting for disordered renal function.
There is no clinical experience with the use of BENICAR® in pregnant women. No teratogenic effects were observed when olmesartan medoxomil was administered to pregnant rats at oral doses up to 1000 mg/kg/day (240 times the maximum recommended human dose [MRHD] of olmesartan medoxomil on a mg/m 2 basis) or pregnant rabbits at oral doses up to 1 mg/kg/day (half the MRHD on a mg/m 2 basis; higher doses could not be evaluated for effects on fetal development as they were lethal to the does). In rats, significant decreases in pup birth weight and weight gain were observed at doses >/=1.6 mg/kg/day, and delays in developmental milestones (delayed separation of ear auricula, eruption of lower incisors, appearance of abdominal hair, descent of testes, and separation of eyelids) and dose-dependent increases in the incidence of dilation of the renal pelvis were observed at doses >/=8 mg/kg/day. The no observed effect dose for developmental toxicity in rats is 0.3 mg/kg/day, about one-tenth the MRHD of 40 mg/day.
Hypotension in Volume- or Salt-Depleted Patients
In patients with an activated renin-angiotensin system, such as volume- and/or salt-depleted patients (e.g., those being treated with high doses of diuretics), symptomatic hypotension may occur after initiation of treatment with BENICAR®. Treatment should start under close medical supervision. If hypotension does occur, the patient should be placed in the supine position and, if necessary, given an intravenous infusion of normal saline (See DOSAGE AND ADMINISTRATION ). A transient hypotensive response is not a contraindication to further treatment, which usually can be continued without difficulty once the blood pressure has stabilized.
PRECAUTIONS
General
Impaired Renal Function: As a consequence of inhibiting the renin-angiotensin-aldosterone system, changes in renal function may be anticipated in susceptible individuals treated with olmesartan medoxomil. In patients whose renal function may depend upon the activity of the renin-angiotensin-aldosterone system (e.g. patients with severe congestive heart failure), treatment with angiotensin converting enzyme inhibitors and angiotensin receptor antagonists has been associated with oliguria and/or progressive azotemia and (rarely) with acute renal failure and/or death. Similar results may be anticipated in patients treated with olmesartan medoxomil. (See CLINICAL PHARMACOLOGY , Special Populations .)
In studies of ACE inhibitors in patients with unilateral or bilateral renal artery stenosis, increases in serum creatinine or blood urea nitrogen (BUN) have been reported. There has been no long-term use of olmesartan medoxomil in patients with unilateral or bilateral renal artery stenosis, but similar results may be expected.
Information for Patients
Pregnancy: Female patients of childbearing age should be told about the consequences of second and third trimester exposure to drugs that act on the renin-angiotensin system and they should be told also that these consequences do not appear to have resulted from intrauterine drug exposure that has been limited to the first trimester. These patients should be asked to report pregnancies to their physicians as soon as possible.
Drug Interactions
No significant drug interactions were reported in studies in which olmesartan medoxomil was co-administered with digoxin or warfarin in healthy volunteers. The bioavailability of olmesartan was not significantly altered by the co-administration of antacids [A1(OH) 3 /Mg(OH) 2 ]. Olmesartan medoxomil is not metabolized by the cytochrome P450 system and has no effects on P450 enzymes; thus, interactions with drugs that inhibit, induce or are metabolized by those enzymes are not expected.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Olmesartan medoxomil was not carcinogenic when administered by dietary administration to rats for up to 2 years. The highest dose tested (2000 mg/kg/day) was, on a mg/m 2 basis, about 480 times the maximum recommended human dose (MRHD) of 40 mg/day. Two carcinogenicity studies conducted in mice, a 6-month gavage study in the p53 knockout mouse and a 6-month dietary administration study in the Hras2 transgenic mouse, at doses of up to 1000 mg/kg/day (about 120 times the MRHD), revealed no evidence of a carcinogenic effect of olmesartan medoxomil.
Both olmesartan medoxomil and olmesartan tested negative in the in vitro Syrian hamster embryo cell transformation assay and showed no evidence of genetic toxicity in the Ames (bacterial mutagenicity) test. However, both were shown to induce chromosomal aberrations in cultured cells in vitro (Chinese hamster lung) and tested positive for thymidine kinase mutations in the in vitro mouse lymphoma assay. Olmesartan medoxomil tested negative in vivo for mutations in the MutaMouse intestine and kidney and for clastogenicity in mouse bone marrow (micronucleus test) at oral doses of up to 2000 mg/kg (olmesartan not tested).
Fertility of rats was unaffected by administration of olmesartan medoxomil at dose levels as high as 1000 mg/kg/day (240 times the MRHD) in a study in which dosing was begun 2 (female) or 9 (male) weeks prior to mating.
Pregnancy
Pregnancy Categories C (first trimester) and D (second and third trimesters). See WARNINGS , Fetal/Neonatal Morbidity and Mortality .
Nursing Mothers
It is not known whether olmesartan is excreted in human milk, but olmesartan is secreted at low concentration in the milk of lactating rats. Because of the potential for adverse effects on the nursing infant, a decision should be made whether to discontinue nursing or discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
Safety and effectiveness in pediatric patients have not been established.
Geriatric Use
Of the total number of hypertensive patients receiving BENICAR® in clinical studies, more than 20% were 65 years of age and over, while more than 5% were 75 years of age and older. No overall differences in effectiveness or safety were observed between elderly patients and younger patients. Other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
ADVERSE REACTIONS
BENICAR® has been evaluated for safety in more than 3825 patients/subjects, including more than 3275 patients treated for hypertension in controlled trials. This experience included about 900 patients treated for at least 6 months and more than 525 for at least 1 year. Treatment with BENICAR® was well tolerated, with an incidence of adverse events similar to placebo. Events generally were mild, transient and had no relationship to the dose of olmesartan medoxomil.
The overall frequency of adverse events was not dose-related. Analysis of gender, age and race groups demonstrated no differences between olmesartan medoxomil and placebo-treated patients. The rate of withdrawals due to adverse events in all trials of hypertensive patients was 2.4% (i.e. 79/3278) of patients treated with olmesartan medoxomil and 2.7% (i.e. 32/1179) of control patients. In placebo-controlled trials, the only adverse event that occurred in more than 1% of patients treated with olmesartan medoxomil and at a higher incidence versus placebo was dizziness (3% vs. 1%).
The following adverse events occurred in placebo-controlled clinical trials at an incidence of more than 1% of patients treated with olmesartan medoxomil, but also occurred at about the same or greater incidence in patients receiving placebo: back pain, bronchitis, creatine phosphokinase increased, diarrhea, headache, hematuria, hyperglycemia, hypertriglyceridemia, influenza-like symptoms, pharyngitis, rhinitis and sinusitis.
The incidence of cough was similar in placebo (0.7%) and BENICAR® (0.9%) patients.
Other (potentially important) adverse events that have been reported with an incidence of greater than 0.5%, whether or not attributed to treatment, in the more than 3100 hypertensive patients treated with olmesartan medoxomil monotherapy in controlled or open-label trials are listed below.
Body as a Whole: chest pain, peripheral edema
Central and Peripheral Nervous System: vertigo
Gastrointestinal: abdominal pain, dyspepsia, gastroenteritis, nausea
Heart Rate and Rhythm Disorders: tachycardia
Metabolic and Nutritional Disorders: hypercholesterolemia, hyperlipemia, hyperuricemia
Musculoskeletal: arthralgia, arthritis, myalgia
Skin and Appendages: rash
Facial edema was reported in 5 patients receiving olmesartan medoxomil. Angioedema has been reported with angiotensin II antagonists.
Laboratory Test Findings: In controlled clinical trials, clinically important changes in standard laboratory parameters were rarely associated with administration of olmesartan medoxomil.
Hemoglobin and Hematocrit: Small decreases in hemoglobin and hematocrit (mean decreases of approximately 0.3 g/dL and 0.3 volume percent, respectively) were observed.
Liver Function Tests: Elevations of liver enzymes and/or serum bilirubin were observed infrequently. Five patients (0.1%) assigned to olmesartan medoxomil and one patient (0.2%) assigned to placebo in clinical trials were withdrawn because of abnormal liver chemistries (transaminases or total bilirubin). Of the five olmesartan medoxomil patients, three had elevated transaminases, which were attributed to alcohol use, and one had a single elevated bilirubin value, which normalized while treatment continued.
Post-Marketing Experience: The following adverse reactions have been reported in post- marketing experience:
Body as a Whole: Asthenia, angioedema
Gastrointestinal: Vomiting
Musculoskeletal: Rhabdomyolysis
Urogenital System: Acute renal failure, increased blood creatinine levels
Skin and Appendages: Alopecia, pruritus, urticaria
OVERDOSAGE
Limited data are available related to overdosage in humans. The most likely manifestations of overdosage would be hypotension and tachycardia; bradycardia could be encountered if parasympathetic (vagal) stimulation occurs. If symptomatic hypotension should occur, supportive treatment should be initiated. The dialyzability of olmesartan is unknown.
DOSAGE AND ADMINISTRATION
Dosage must be individualized. The usual recommended starting dose of BENICAR® is 20 mg once daily when used as monotherapy in patients who are not volume-contracted. For patients requiring further reduction in blood pressure after 2 weeks of therapy, the dose of BENICAR® may be increased to 40 mg. Doses above 40 mg do not appear to have greater effect. Twice-daily dosing offers no advantage over the same total dose given once daily.
No initial dosage adjustment is recommended for elderly patients, for patients with moderate to marked renal impairment (creatinine clearance <40mL/min) or with moderate to marked hepatic dysfunction (see CLINICAL PHARMACOLOGY , Special Populations ). For patients with possible depletion of intravascular volume (e.g., patients treated with diuretics, particularly those with impaired renal function), BENICAR® should be initiated under close medical supervision and consideration should be given to use of a lower starting dose (see WARNINGS , Hypotension in Volume- and Salt-Depleted Patients ).
BENICAR® may be administered with or without food.
If blood pressure is not controlled by BENICAR® alone, a diuretic may be added. BENICAR® may be administered with other antihypertensive agents.
HOW SUPPLIED
BENICAR® is supplied as yellow, round, film-coated tablets containing 5 mg of olmesartan medoxomil, as white, round, film-coated tablets containing 20 mg of olmesartan medoxomil, and as white, oval-shaped, film-coated tablets containing 40 mg of olmesartan medoxomil. Tablets are debossed with Sankyo on one side and C12, C14, or C15 on the other side of the 5, 20, and 40 mg tablets, respectively.
Tablets are supplied as follows:
5 mg20 mg40 mgBottle of 30NDC 65597-101-30NDC 65597-103-30NDC 65597-104-30Bottle of 90Not availableNDC 65597-103-90NDC 65597-104-90Blister 10 cards X 10NDC 65597-103-10NDC 65597-104-10Storage
Store at 20-25°C (68-77°F) [See USP Controlled Room Temperature].
Manufactured for Sankyo Pharma Inc., Parsippany, New Jersey 07054
Rx Only
Copyright © Sankyo Pharma Inc. 2004. All rights reserved.
P180606 Revised July 2005
Subscribe to the "News" RSS Feed 
TOP ۞
