-
Cipro I.V. Pharmacy Bulk Package (Bayer)
PHARMACY BULK PACKAGE--NOT FOR DIRECT INFUSION
To reduce the development of drug-resistant bacteria and maintain the effectiveness of CIPRO® I.V. and other antibacterial drugs, CIPRO I.V. should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria.
DESCRIPTION
The pharmacy bulk package is a single-entry container of a sterile preparation for parenteral use that contains many single doses. It contains ciprofloxacin as a 1% aqueous solution concentrate. The contents are intended for use in a pharmacy admixture program and are restricted to the preparation of admixtures for intravenous infusion.
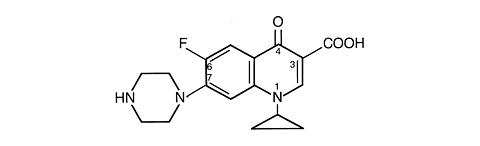
CIPRO I.V. (ciprofloxacin) is a synthetic broad-spectrum antimicrobial agent for intravenous (I.V.) administration. Ciprofloxacin, a fluoroquinolone, is 1-cyclopropyl-6-fluoro-1, 4-dihydro-4-oxo-7-(1-piperazinyl)-3-quinolinecarboxylic acid. Its empirical formula is C 17 H 18 FN 3 O 3 and its chemical structure is:
Ciprofloxacin is a faint to light yellow crystalline powder with a molecular weight of 331.4. It is soluble in dilute (0.1N) hydrochloric acid and is practically insoluble in water and ethanol. CIPRO I.V. solution is available as a sterile 1.0% aqueous concentrate, which is intended for dilution prior to administration. Ciprofloxacin solution contains lactic acid as a solubilizing agent and hydrochloric acid for pH adjustment. The pH range for the 1.0% aqueous concentrate is 3.3 to 3.9.
CLINICAL PHARMACOLOGY
Absorption
Following 60-minute intravenous infusions of 200 mg and 400 mg ciprofloxacin to normal volunteers, the mean maximum serum concentrations achieved were 2.1 and 4.6 µg/mL, respectively; the concentrations at 12 hours were 0.1 and 0.2 µg/mL, respectively.
Steady-state Ciprofloxacin Serum Concentrations (µg/mL)
After 60-minute I.V. Infusions q 12 h.Time after starting the infusion Dose30 min. 1 hr 3 hr 6 hr 8 hr 12 hr 200 mg1.7 2.1 0.6 0.3 0.2 0.1 400 mg3.7 4.6 1.3 0.7 0.5 0.2 The pharmacokinetics of ciprofloxacin are linear over the dose range of 200 to 400 mg administered intravenously. Comparison of the pharmacokinetic parameters following the 1st and 5th I.V. dose on a q 12 h regimen indicates no evidence of drug accumulation.
The absolute bioavailability of oral ciprofloxacin is within a range of 70-80% with no substantial loss by first pass metabolism. An intravenous infusion of 400-mg ciprofloxacin given over 60 minutes every 12 hours has been shown to produce an area under the serum concentration time curve (AUC) equivalent to that produced by a 500-mg oral dose given every 12 hours. An intravenous infusion of 400 mg ciprofloxacin given over 60 minutes every 8 hours has been shown to produce an AUC at steady-state equivalent to that produced by a 750-mg oral dose given every 12 hours. A 400-mg I.V. dose results in a C max similar to that observed with a 750-mg oral dose. An infusion of 200 mg ciprofloxacin given every 12 hours produces an AUC equivalent to that produced by a 250-mg oral dose given every 12 hours.
Steady-state Pharmacokinetic Parameter Following Multiple Oral and I.V. Doses Parameters500 mg
q12h, P.O.400 mg
q12h, I.V.750 mg
q12h, P.O.400 mg
q8h, I.V.AUC (µg·hr/mL)13.7 a 12.7 a 31.6 b 32.9 c C max (µg/mL)2.97 4.56 3.59 4.07 a AUC 0-12h b AUC 24h=AUC 0-12h × 2 c AUC 24h=AUC 0-8h × 3 Distribution
After intravenous administration, ciprofloxacin is present in saliva, nasal and bronchial secretions, sputum, skin blister fluid, lymph, peritoneal fluid, bile, and prostatic secretions. It has also been detected in the lung, skin, fat, muscle, cartilage, and bone. Although the drug diffuses into cerebrospinal fluid (CSF), CSF concentrations are generally less than 10% of peak serum concentrations. Levels of the drug in the aqueous and vitreous chambers of the eye are lower than in serum.
Metabolism
After I.V. administration, three metabolites of ciprofloxacin have been identified in human urine which together account for approximately 10% of the intravenous dose. The binding of ciprofloxacin to serum proteins is 20 to 40%.
Excretion
The serum elimination half-life is approximately 5-6 hours and the total clearance is around 35 L/hr. After intravenous administration, approximately 50% to 70% of the dose is excreted in the urine as unchanged drug. Following a 200-mg I.V. dose, concentrations in the urine usually exceed 200 µg/mL 0-2 hours after dosing and are generally greater than 15 µg/mL 8-12 hours after dosing. Following a 400-mg I.V. dose, urine concentrations generally exceed 400 µg/mL 0-2 hours after dosing and are usually greater than 30 µg/mL 8-12 hours after dosing. The renal clearance is approximately 22 L/hr. The urinary excretion of ciprofloxacin is virtually complete by 24 hours after dosing.
Although bile concentrations of ciprofloxacin are several fold higher than serum concentrations after intravenous dosing, only a small amount of the administered dose (< 1%) is recovered from the bile as unchanged drug. Approximately 15% of an I.V. dose is recovered from the feces within 5 days after dosing.
Special Populations
Pharmacokinetic studies of the oral (single dose) and intravenous (single and multiple dose) forms of ciprofloxacin indicate that plasma concentrations of ciprofloxacin are higher in elderly subjects (> 65 years) as compared to young adults. Although the C max is increased 16-40%, the increase in mean AUC is approximately 30%, and can be at least partially attributed to decreased renal clearance in the elderly. Elimination half-life is only slightly (~20%) prolonged in the elderly. These differences are not considered clinically significant. (See PRECAUTIONS : Geriatric Use .)
In patients with reduced renal function, the half-life of ciprofloxacin is slightly prolonged and dosage adjustments may be required. (See DOSAGE AND ADMINISTRATION .)
In preliminary studies in patients with stable chronic liver cirrhosis, no significant changes in ciprofloxacin pharmacokinetics have been observed. However, the kinetics of ciprofloxacin in patients with acute hepatic insufficiency have not been fully elucidated.
Following a single oral dose of 10 mg/kg ciprofloxacin suspension to 16 children ranging in age from 4 months to 7 years, the mean C max was 2.4 µg/mL (range: 1.5 - 3.4 µg/mL) and the mean AUC was 9.2 µg*h/mL (range: 5.8 - 14.9 µg*h/mL). There was no apparent age-dependence, and no notable increase in C max or AUC upon multiple dosing (10 mg/kg TID). In children with severe sepsis who were given intravenous ciprofloxacin (10 mg/kg as a 1-hour infusion), the mean C max was 6.1 µg/mL (range: 4.6 - 8.3 µg/mL) in 10 children less than 1 year of age; and 7.2 µg/mL (range: 4.7 - 11.8 µg/mL) in 10 children between 1 and 5 years of age. The AUC values were 17.4 µg*h/mL (range: 11.8 - 32.0 µg*h/mL) and 16.5 µg*h/mL (range: 11.0 - 23.8 µg*h/mL) in the respective age groups. These values are within the range reported for adults at therapeutic doses. Based on population pharmacokinetic analysis of pediatric patients with various infections, the predicted mean half-life in children is approximately 4-5 hours, and the bioavailability of the oral suspension is approximately 60%.
Drug-drug Interactions: The potential for pharmacokinetic drug interactions between ciprofloxacin and theophylline, caffeine, cyclosporins, phenytoin, sulfonylurea glyburide, metronidazole, warfarin, probenecid, and piperacillin sodium has been evaluated. (See PRECAUTIONS : Drug Interactions .)
MICROBIOLOGY
Ciprofloxacin has in vitro activity against a wide range of gram-negative and gram-positive microorganisms. The bactericidal action of ciprofloxacin results from inhibition of the enzymes topoisomerase II (DNA gyrase) and topoisomerase IV, which are required for bacterial DNA replication, transcription, repair, and recombination. The mechanism of action of fluoroquinolones, including ciprofloxacin, is different from that of penicillins, cephalosporins, aminoglycosides, macrolides, and tetracyclines; therefore, microorganisms resistant to these classes of drugs may be susceptible to ciprofloxacin and other quinolones. There is no known cross-resistance between ciprofloxacin and other classes of antimicrobials. In vitro resistance to ciprofloxacin develops slowly by multiple step mutations.
Ciprofloxacin is slightly less active when tested at acidic pH. The inoculum size has little effect when tested in vitro . The minimal bactericidal concentration (MBC) generally does not exceed the minimal inhibitory concentration (MIC) by more than a factor of 2.
Ciprofloxacin has been shown to be active against most strains of the following microorganisms, both in vitro and in clinical infections as described in the INDICATIONS AND USAGE section of the package insert for CIPRO I.V. (ciprofloxacin for intravenous infusion).
Aerobic gram-positive microorganisms
Enterococcus faecalis (Many strains are only moderately susceptible.)
Staphylococcus aureus (methicillin-susceptible strains only)
Staphylococcus epidermidis (methicillin-susceptible strains only)
Staphylococcus saprophyticus
Streptococcus pneumoniae (penicillin-susceptible strains)
Streptococcus pyogenes
Aerobic gram-negative microorganisms
Citrobacter diversus
Citrobacter freundii
Enterobacter cloacae
Escherichia coli
Haemophilus influenzae
Haemophilus parainfluenzae
Klebsiella pneumoniae
Moraxella catarrhalis
Morganella morganii
Proteus mirabilis
Proteus vulgaris
Providencia rettgeri
Providencia stuartii
Pseudomonas aeruginosa
Serratia marcescens
Ciprofloxacin has been shown to be active against Bacillus anthracis both in vitro and by use of serum levels as a surrogate marker (see INDICATIONS AND USAGE and INHALATIONAL ANTHRAX - ADDITIONAL INFORMATION ).
The following in vitro data are available, but their clinical significance is unknown .
Ciprofloxacin exhibits in vitro minimum inhibitory concentrations (MICs) of 1 µg/mL or less against most (>/= 90%) strains of the following microorganisms; however, the safety and effectiveness of ciprofloxacin intravenous formulations in treating clinical infections due to these microorganisms have not been established in adequate and well-controlled clinical trials.
Aerobic gram-positive microorganisms
Staphylococcus haemolyticus
Staphylococcus hominis
Streptococcus pneumoniae (penicillin-resistant strains)
Aerobic gram-negative microorganisms
Acinetobacter lwoffi
Aeromonas hydrophila
Campylobacter jejuni
Edwardsiella tarda
Enterobacter aerogenes
Klebsiella oxytoca
Legionella pneumophila
Neisseria gonorrhoeae
Pasteurella multocida
Salmonella enteritidis
Salmonella typhi
Shigella boydii
Shigella dysenteriae
Shigella flexneri
Shigella sonnei
Vibrio cholerae
Vibrio parahaemolyticus
Vibrio vulnificus
Yersinia enterocolitica
Most strains of Burkholderia cepacia and some strains of Stenotrophomonas maltophilia are resistant to ciprofloxacin as are most anaerobic bacteria, including Bacteroides fragilis and Clostridium difficile .
Susceptibility Tests
Dilution Techniques: Quantitative methods are used to determine antimicrobial minimum inhibitory concentrations (MICs). These MICs provide estimates of the susceptibility of bacteria to antimicrobial compounds. The MICs should be determined using a standardized procedure. Standardized procedures are based on a dilution method 1 (broth or agar) or equivalent with standardized inoculum concentrations and standardized concentrations of ciprofloxacin powder. The MIC values should be interpreted according to the following criteria:
For testing aerobic microorganisms other than Haemophilus influenzae, and Haemophilus parainfluenzae a :
MIC (µg/mL)Interpretation </= 1Susceptible (S) 2Intermediate (I) >/= 4Resistant (R) a These interpretive standards are applicable only to broth microdilution susceptibility tests with streptococci using cation-adjusted Mueller-Hinton broth with 2-5% lysed horse blood.
For testing Haemophilus influenzae and Haemophilus parainfluenzae b :
MIC (µg/mL)Interpretation </= 1Susceptible (S) b This interpretive standard is applicable only to broth microdilution susceptibility tests with Haemophilus influenzae and Haemophilus parainfluenzae using Haemophilus Test Medium 1 .
The current absence of data on resistant strains precludes defining any results other than "Susceptible". Strains yielding MIC results suggestive of a "nonsusceptible" category should be submitted to a reference laboratory for further testing.
A report of "Susceptible" indicates that the pathogen is likely to be inhibited if the antimicrobial compound in the blood reaches the concentrations usually achievable. A report of "Intermediate" indicates that the result should be considered equivocal, and, if the microorganism is not fully susceptible to alternative, clinically feasible drugs, the test should be repeated. This category implies possible clinical applicability in body sites where the drug is physiologically concentrated or in situations where high dosage of drug can be used. This category also provides a buffer zone, which prevents small uncontrolled technical factors from causing major discrepancies in interpretation. A report of "Resistant" indicates that the pathogen is not likely to be inhibited if the antimicrobial compound in the blood reaches the concentrations usually achievable; other therapy should be selected.
Standardized susceptibility test procedures require the use of laboratory control microorganisms to control the technical aspects of the laboratory procedures. Standard ciprofloxacin powder should provide the following MIC values:
OrganismMIC (µg/mL) E. faecalisATCC 29212 0.25 - 2.0 E. coliATCC 25922 0.004 - 0.015 H. influenzae aATCC 49247 0.004 - 0.03 P. aeruginosaATCC 27853 0.25 - 1.0 S. aureusATCC 29213 0.12 - 0.5 a This quality control range is applicable to only H. influenzae ATCC 49247 tested by a broth microdilution procedure using Haemophilus Test Medium (HTM) 1 .
Diffusion Techniques: Quantitative methods that require measurement of zone diameters also provide reproducible estimates of the susceptibility of bacteria to antimicrobial compounds. One such standardized procedure 2 requires the use of standardized inoculum concentrations. This procedure uses paper disks impregnated with 5-µg ciprofloxacin to test the susceptibility of microorganisms to ciprofloxacin.
Reports from the laboratory providing results of the standard single-disk susceptibility test with a 5-µg ciprofloxacin disk should be interpreted according to the following criteria:
For testing aerobic microorganisms other than Haemophilus influenzae, and Haemophilus parainfluenzae a :
Zone Diameter (mm)Interpretation >/= 21Susceptible (S) 16-20Intermediate (I) </= 15Resistant (R) a These zone diameter standards are applicable only to tests performed for streptococci using Mueller-Hinton agar supplemented with 5% sheep blood incubated in 5% CO 2 .
For testing Haemophilus influenzae and Haemophilus parainfluenzae b :
Zone Diameter (mm)Interpretation >/= 21Susceptible (S) b This zone diameter standard is applicable only to tests with Haemophilus influenzae and Haemophilus parainfluenzae using Haemophilus Test Medium (HTM) 2 .
The current absence of data on resistant strains precludes defining any results other than "Susceptible". Strains yielding zone diameter results suggestive of a "nonsusceptible" category should be submitted to a reference laboratory for further testing.
Interpretation should be as stated above for results using dilution techniques. Interpretation involves correlation of the diameter obtained in the disk test with the MIC for ciprofloxacin.
As with standardized dilution techniques, diffusion methods require the use of laboratory control microorganisms that are used to control the technical aspects of the laboratory procedures. For the diffusion technique, the 5-µg ciprofloxacin disk should provide the following zone diameters in these laboratory test quality control strains:
OrganismZone Diameter
(mm)E. coliATCC 25922 30-40 H. influenzae aATCC 49247 34-42 P. aeruginosaATCC 27853 25-33 S. aureusATCC 25923 22-30 a These quality control limits are applicable to only H. influenzae ATCC 49247 testing using Haemophilus Test Medium (HTM) 2 .
INDICATIONS AND USAGE
CIPRO I.V. is indicated for the treatment of infections caused by susceptible strains of the designated microorganisms in the conditions and patient populations listed below when the intravenous administration offers a route of administration advantageous to the patient. Please see DOSAGE AND ADMINISTRATION for specific recommendations.
Adult Patients:
Urinary Tract Infections caused by Escherichia coli (including cases with secondary bacteremia), Klebsiella pneumoniae subspecies pneumoniae, Enterobacter cloacae, Serratia marcescens, Proteus mirabilis, Providencia rettgeri, Morganella morganii, Citrobacter diversus, Citrobacter freundii, Pseudomonas aeruginosa, Staphylococcus epidermidis, Staphylococcus saprophyticus, or Enterococcus faecalis .
Lower Respiratory Infections caused by Escherichia coli, Klebsiella pneumoniae subspecies pneumoniae, Enterobacter cloacae, Proteus mirabilis, Pseudomonas aeruginosa, Haemophilus influenzae, Haemophilus parainfluenzae, or Streptococcus pneumoniae . Also, Moraxella catarrhalis for the treatment of acute exacerbations of chronic bronchitis.
NOTE: Although effective in clinical trials, ciprofloxacin is not a drug of first choice in the treatment of presumed or confirmed pneumonia secondary to Streptococcus pneumoniae .
Nosocomial Pneumonia caused by Haemophilus influenzae or Klebsiella pneumoniae .
Skin and Skin Structure Infections caused by Escherichia coli, Klebsiella pneumoniae subspecies pneumoniae, Enterobacter cloacae, Proteus mirabilis, Proteus vulgaris, Providencia stuartii, Morganella morganii, Citrobacter freundii, Pseudomonas aeruginosa, Staphylococcus aureus (methicillin susceptible), Staphylococcus epidermidis, or Streptococcus pyogenes .
Bone and Joint Infections caused by Enterobacter cloacae, Serratia marcescens, or Pseudomonas aeruginosa .
Complicated Intra-Abdominal Infections (used in conjunction with metronidazole) caused by Escherichia coli, Pseudomonas aeruginosa, Proteus mirabilis, Klebsiella pneumoniae, or Bacteroides fragilis .
Acute Sinusitis caused by Haemophilus influenzae, Streptococcus pneumoniae, or Moraxella catarrhalis .
Chronic Bacterial Prostatitis caused by Escherichia coli or Proteus mirabilis.
Empirical Therapy for Febrile Neutropenic Patients in combination with piperacillin sodium. (See CLINICAL STUDIES.)
Pediatric patients (1 to 17 years of age):
Complicated Urinary Tract Infections and Pyelonephritis due to Escherichia coli .
NOTE: Although effective in clinical trials, ciprofloxacin is not a drug of first choice in the pediatric population due to an increased incidence of adverse events compared to controls, including events related to joints and/or surrounding tissues. (See WARNINGS , PRECAUTIONS , Pediatric Use , ADVERSE REACTIONS and CLINICAL STUDIES .) Ciprofloxacin, like other fluoroquinolones, is associated with arthropathy and histopathological changes in weight-bearing joints of juvenile animals. (See ANIMAL PHARMACOLOGY .)
Adult and Pediatric Patients:
Inhalational anthrax (post-exposure): To reduce the incidence or progression of disease following exposure to aerosolized Bacillus anthracis.
Ciprofloxacin serum concentrations achieved in humans served as a surrogate endpoint reasonably likely to predict clinical benefit and provided the initial basis for approval of this indication. 4 Supportive clinical information for ciprofloxacin for anthrax post-exposure prophylaxis was obtained during the anthrax bioterror attacks of October 2001. (See also, INHALATIONAL ANTHRAX - ADDITIONAL INFORMATION ).
If anaerobic organisms are suspected of contributing to the infection, appropriate therapy should be administered.
Appropriate culture and susceptibility tests should be performed before treatment in order to isolate and identify organisms causing infection and to determine their susceptibility to ciprofloxacin. Therapy with CIPRO I.V. may be initiated before results of these tests are known; once results become available, appropriate therapy should be continued.
As with other drugs, some strains of Pseudomonas aeruginosa may develop resistance fairly rapidly during treatment with ciprofloxacin. Culture and susceptibility testing performed periodically during therapy will provide information not only on the therapeutic effect of the antimicrobial agent but also on the possible emergence of bacterial resistance.
To reduce the development of drug-resistant bacteria and maintain the effectiveness of CIPRO I.V. and other antibacterial drugs, CIPRO I.V. should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
CONTRAINDICATIONS
Ciprofloxacin is contraindicated in persons with a history of hypersensitivity to ciprofloxacin, any member of the quinolone class of antimicrobial agents, or any of the product components.
Concomitant administration with tizanidine is contraindicated.
WARNINGS
Pregnant Women: THE SAFETY AND EFFECTIVENESS OF CIPROFLOXACIN IN PREGNANT AND LACTATING WOMEN HAVE NOT BEEN ESTABLISHED. (See PRECAUTIONS : Pregnancy, and Nursing Mothers subsections.)
Pediatrics: Ciprofloxacin should be used in pediatric patients (less than 18 years of age) only for infections listed in the INDICATIONS AND USAGE section. An increased incidence of adverse events compared to controls, including events related to joints and/or surrounding tissues, has been observed. (See ADVERSE REACTIONS .)
In pre-clinical studies, oral administration of ciprofloxacin caused lameness in immature dogs. Histopathological examination of the weight-bearing joints of these dogs revealed permanent lesions of the cartilage. Related quinolone-class drugs also produce erosions of cartilage of weight-bearing joints and other signs of arthropathy in immature animals of various species. (See ANIMAL PHARMACOLOGY .)
Cytochrome P450: Ciprofloxacin is a moderate inhibitor of the CYP 450 1A2 isoenzymes. Coadministration of ciprofloxacin and other drugs primarily metabolized by the cytochrome P450 1A2 enzyme pathway (e.g. theophylline, methylxanthines) may result in increased plasma concentrations of the coadministered drug and could lead to clinically significant pharmacodynamic side effects.
Central Nervous System Disorders: Convulsions, increased intracranial pressure and toxic psychosis have been reported in patients receiving quinolones, including ciprofloxacin. Ciprofloxacin may also cause central nervous system (CNS) events including: dizziness, confusion, tremors, hallucinations, depression, and, rarely, suicidal thoughts or acts. These reactions may occur following the first dose. If these reactions occur in patients receiving ciprofloxacin, the drug should be discontinued and appropriate measures instituted. As with all quinolones, ciprofloxacin should be used with caution in patients with known or suspected CNS disorders that may predispose to seizures or lower the seizure threshold (e.g. severe cerebral arteriosclerosis, epilepsy), or in the presence of other risk factors that may predispose to seizures or lower the seizure threshold (e.g. certain drug therapy, renal dysfunction). (See PRECAUTIONS: General, Information for Patients, Drug Interaction and ADVERSE REACTIONS .)
Theophylline: SERIOUS AND FATAL REACTIONS HAVE BEEN REPORTED IN PATIENTS RECEIVING CONCURRENT ADMINISTRATION OF INTRAVENOUS CIPROFLOXACIN AND THEOPHYLLINE. These reactions have included cardiac arrest, seizure, status epilepticus, and respiratory failure. Although similar serious adverse events have been reported in patients receiving theophylline alone, the possibility that these reactions may be potentiated by ciprofloxacin cannot be eliminated. If concomitant use cannot be avoided, serum levels of theophylline should be monitored and dosage adjustments made as appropriate.
Hypersensitivity Reactions: Serious and occasionally fatal hypersensitivity (anaphylactic) reactions, some following the first dose, have been reported in patients receiving quinolone therapy. Some reactions were accompanied by cardiovascular collapse, loss of consciousness, tingling, pharyngeal or facial edema, dyspnea, urticaria, and itching. Only a few patients had a history of hypersensitivity reactions. Serious anaphylactic reactions require immediate emergency treatment with epinephrine and other resuscitation measures, including oxygen, intravenous fluids, intravenous antihistamines, corticosteroids, pressor amines, and airway management, as clinically indicated.
Severe hypersensitivity reactions characterized by rash, fever, eosinophilia, jaundice, and hepatic necrosis with fatal outcome have also been reported extremely rarely in patients receiving ciprofloxacin along with other drugs. The possibility that these reactions were related to ciprofloxacin cannot be excluded. Ciprofloxacin should be discontinued at the first appearance of a skin rash or any other sign of hypersensitivity.
Pseudomembranous Colitis: Pseudomembranous colitis has been reported with nearly all antibacterial agents, including ciprofloxacin, and may range in severity from mild to life-threatening. Therefore, it is important to consider this diagnosis in patients who present with diarrhea subsequent to the administration of antibacterial agents.
Treatment with antibacterial agents alters the normal flora of the colon and may permit overgrowth of clostridia. Studies indicate that a toxin produced by Clostridium difficile is one primary cause of "antibiotic-associated colitis."
After the diagnosis of pseudomembranous colitis has been established, therapeutic measures should be initiated. Mild cases of pseudomembranous colitis usually respond to drug discontinuation alone. In moderate to severe cases, consideration should be given to management with fluids and electrolytes, protein supplementation, and treatment with an antibacterial drug clinically effective against C. difficile colitis. Drugs that inhibit peristalsis should be avoided.
Peripheral neuropathy: Rare cases of sensory or sensorimotor axonal polyneuropathy affecting small and/or large axons resulting in paresthesias, hypoesthesias, dysesthesias and weakness have been reported in patients receiving quinolones, including ciprofloxacin. Ciprofloxacin should be discontinued if the patient experiences symptoms of neuropathy including pain, burning, tingling, numbness, and/or weakness, or is found to have deficits in light touch, pain, temperature, position sense, vibratory sensation, and/or motor strength in order to prevent the development of an irreversible condition.
Tendon Effects: Ruptures of the shoulder, hand, Achilles tendon or other tendons that required surgical repair or resulted in prolonged disability have been reported in patients receiving quinolones, including ciprofloxacin. Post-marketing surveillance reports indicate that this risk may be increased in patients receiving concomitant corticosteroids, especially the elderly. Ciprofloxacin should be discontinued if the patient experiences pain, inflammation, or rupture of a tendon. Patients should rest and refrain from exercise until the diagnosis of tendonitis or tendon rupture has been excluded. Tendon rupture can occur during or after therapy with quinolones, including ciprofloxacin.
PRECAUTIONS
General: INTRAVENOUS CIPROFLOXACIN SHOULD BE ADMINISTERED BY SLOW INFUSION OVER A PERIOD OF 60 MINUTES. Local I.V. site reactions have been reported with the intravenous administration of ciprofloxacin. These reactions are more frequent if infusion time is 30 minutes or less or if small veins of the hand are used. (See ADVERSE REACTIONS .)
Central Nervous System: Quinolones, including ciprofloxacin, may also cause central nervous system (CNS) events, including: nervousness, agitation, insomnia, anxiety, nightmares or paranoia. (See WARNINGS, Information for Patients, and Drug Interactions .)
Crystals of ciprofloxacin have been observed rarely in the urine of human subjects but more frequently in the urine of laboratory animals, which is usually alkaline. (See ANIMAL PHARMACOLOGY .) Crystalluria related to ciprofloxacin has been reported only rarely in humans because human urine is usually acidic. Alkalinity of the urine should be avoided in patients receiving ciprofloxacin. Patients should be well hydrated to prevent the formation of highly concentrated urine.
Renal Impairment: Alteration of the dosage regimen is necessary for patients with impairment of renal function. (See DOSAGE AND ADMINISTRATION .)
Phototoxicity: Moderate to severe phototoxicity manifested as an exaggerated sunburn reaction has been observed in some patients who were exposed to direct sunlight while receiving some members of the quinolone class of drugs. Excessive sunlight should be avoided.
As with any potent drug, periodic assessment of organ system functions, including renal, hepatic, and hematopoietic, is advisable during prolonged therapy.
Prescribing CIPRO I.V. in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
Information For Patients:
Patients should be advised:
- that antibacterial drugs including CIPRO I.V. should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When CIPRO I.V. is prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by CIPRO I.V. or other antibacterial drugs in the future.
- that ciprofloxacin may be associated with hypersensitivity reactions, even following a single dose, and to discontinue the drug at the first sign of a skin rash or other allergic reaction.
- that ciprofloxacin may cause dizziness and lightheadedness; therefore, patients should know how they react to this drug before they operate an automobile or machinery or engage in activities requiring mental alertness or coordination.
- that ciprofloxacin may increase the effects of theophylline and caffeine. There is a possibility of caffeine accumulation when products containing caffeine are consumed while taking ciprofloxacin.
- that peripheral neuropathies have been associated with ciprofloxacin use. If symptoms of peripheral neuropathy including pain, burning, tingling, numbness and/or weakness develop, they should discontinue treatment and contact their physicians.
- to discontinue treatment; rest and refrain from exercise; and inform their physician if they experience pain, inflammation, or rupture of a tendon.
- that convulsions have been reported in patients taking quinolones, including ciprofloxacin, and to notify their physician before taking this drug if there is a history of this condition.
- that ciprofloxacin has been associated with an increased rate of adverse events involving joints and surrounding tissue structures (like tendons) in pediatric patients (less than 18 years of age). Parents should inform their child's physician if the child has a history of joint-related problems before taking this drug. Parents of pediatric patients should also notify their child's physician of any joint-related problems that occur during or following ciprofloxacin therapy. (See WARNINGS , PRECAUTIONS , Pediatric Use and ADVERSE REACTIONS .)
Drug Interactions: In a pharmacokinetic study, tizanidine serum concentrations were significantly increased (C max 7-fold, AUC 10-fold) when the drug was given concomitantly with ciprofloxacin. Potentiated hypotensive and sedative effects were observed. Coadministration of tizanidine and ciprofloxacin must be avoided.
As with some other quinolones, concurrent administration of ciprofloxacin with theophylline may lead to elevated serum concentrations of theophylline and prolongation of its elimination half-life. This may result in increased risk of theophylline-related adverse reactions. (See WARNINGS .) If concomitant use cannot be avoided, serum levels of theophylline should be monitored and dosage adjustments made as appropriate.
Some quinolones, including ciprofloxacin, have also been shown to interfere with the metabolism of caffeine. This may lead to reduced clearance of caffeine and prolongation of its serum half-life.
Some quinolones, including ciprofloxacin, have been associated with transient elevations in serum creatinine in patients receiving cyclosporine concomitantly.
Altered serum levels of phenytoin (increased and decreased) have been reported in patients receiving concomitant ciprofloxacin.
The concomitant administration of ciprofloxacin with the sulfonylurea glyburide has, in some patients, resulted in severe hypoglycemia. Fatalities have been reported.
The serum concentrations of ciprofloxacin and metronidazole were not altered when these two drugs were given concomitantly.
Quinolones, including ciprofloxacin, have been reported to enhance the effects of the oral anticoagulant warfarin or its derivatives. When these products are administered concomitantly, prothrombin time or other suitable coagulation tests should be closely monitored.
Probenecid interferes with renal tubular secretion of ciprofloxacin and produces an increase in the level of ciprofloxacin in the serum. This should be considered if patients are receiving both drugs concomitantly.
Renal tubular transport of methotrexate may be inhibited by concomitant administration of ciprofloxacin potentially leading to increased plasma levels of methotrexate. This might increase the risk of methotrexate associated toxic reactions. Therefore, patients under methotrexate therapy should be carefully monitored when concomitant ciprofloxacin therapy is indicated.
Non-steroidal anti-inflammatory drugs (but not acetyl salicylic acid) in combination of very high doses of quinolones have been shown to provoke convulsions in pre-clinical studies.
Following infusion of 400 mg I.V. ciprofloxacin every eight hours in combination with 50 mg/kg I.V. piperacillin sodium every four hours, mean serum ciprofloxacin concentrations were 3.02 µg/mL ½ hour and 1.18 between 6-8 hours after the end of infusion.
Carcinogenesis, Mutagenesis, Impairment of Fertility: Eight in vitro mutagenicity tests have been conducted with ciprofloxacin. Test results are listed below:
Salmonella/Microsome Test (Negative)
E. coli DNA Repair Assay (Negative)
Mouse Lymphoma Cell Forward Mutation Assay (Positive)
Chinese Hamster V 79 Cell HGPRT Test (Negative)
Syrian Hamster Embryo Cell Transformation Assay (Negative)
Saccharomyces cerevisiae Point Mutation Assay (Negative)
Saccharomyces cerevisiae Mitotic Crossover and Gene Conversion Assay (Negative)
Rat Hepatocyte DNA Repair Assay (Positive)
Thus, two of the eight tests were positive, but results of the following three in vivo test systems gave negative results:
Rat Hepatocyte DNA Repair Assay
Micronucleus Test (Mice)
Dominant Lethal Test (Mice)
Long-term carcinogenicity studies in rats and mice resulted in no carcinogenic or tumorigenic effects due to ciprofloxacin at daily oral dose levels up to 250 and 750 mg/kg to rats and mice, respectively (approximately 1.7- and 2.5- times the highest recommended therapeutic dose based upon mg/m 2 ).
Results from photo co-carcinogenicity testing indicate that ciprofloxacin does not reduce the time to appearance of UV-induced skin tumors as compared to vehicle control. Hairless (Skh-1) mice were exposed to UVA light for 3.5 hours five times every two weeks for up to 78 weeks while concurrently being administered ciprofloxacin. The time to development of the first skin tumors was 50 weeks in mice treated concomitantly with UVA and ciprofloxacin (mouse dose approximately equal to maximum recommended human dose based upon mg/m 2 ), as opposed to 34 weeks when animals were treated with both UVA and vehicle. The times to development of skin tumors ranged from 16-32 weeks in mice treated concomitantly with UVA and other quinolones. 3
In this model, mice treated with ciprofloxacin alone did not develop skin or systemic tumors. There are no data from similar models using pigmented mice and/or fully haired mice. The clinical significance of these findings to humans is unknown.
Fertility studies performed in rats at oral doses of ciprofloxacin up to 100 mg/kg (approximately 0.7-times the highest recommended therapeutic dose based upon mg/m 2 ) revealed no evidence of impairment.
Pregnancy: Teratogenic Effects. Pregnancy Category C: There are no adequate and well-controlled studies in pregnant women. An expert review of published data on experiences with ciprofloxacin use during pregnancy by TERIS - the Teratogen Information System - concluded that therapeutic doses during pregnancy are unlikely to pose a substantial teratogenic risk (quantity and quality of data=fair), but the data are insufficient to state that there is no risk. 7
A controlled prospective observational study followed 200 women exposed to fluoroquinolones (52.5% exposed to ciprofloxacin and 68% first trimester exposures) during gestation. 8 In utero exposure to fluoroquinolones during embryogenesis was not associated with increased risk of major malformations. The reported rates of major congenital malformations were 2.2% for the fluoroquinolone group and 2.6% for the control group (background incidence of major malformations is 1-5%). Rates of spontaneous abortions, prematurity and low birth weight did not differ between the groups and there were no clinically significant musculoskeletal dysfunctions up to one year of age in the ciprofloxacin exposed children.
Another prospective follow-up study reported on 549 pregnancies with fluoroquinolone exposure (93% first trimester exposures). 9 There were 70 ciprofloxacin exposures, all within the first trimester. The malformation rates among live-born babies exposed to ciprofloxacin and to fluoroquinolones overall were both within background incidence ranges. No specific patterns of congenital abnormalities were found. The study did not reveal any clear adverse reactions due to in utero exposure to ciprofloxacin.
No differences in the rates of prematurity, spontaneous abortions, or birth weight were seen in women exposed to ciprofloxacin during pregnancy. 7,8 However, these small postmarketing epidemiology studies, of which most experience is from short term, first trimester exposure, are insufficient to evaluate the risk for less common defects or to permit reliable and definitive conclusions regarding the safety of ciprofloxacin in pregnant women and their developing fetuses. Ciprofloxacin should not be used during pregnancy unless the potential benefit justifies the potential risk to both fetus and mother (see WARNINGS ).
Reproduction studies have been performed in rats and mice using oral doses up to 100 mg/kg (0.6 and 0.3 times the maximum daily human dose based upon body surface area, respectively) and have revealed no evidence of harm to the fetus due to ciprofloxacin. In rabbits, oral ciprofloxacin dose levels of 30 and 100 mg/kg (approximately 0.4- and 1.3-times the highest recommended therapeutic dose based upon mg/m 2 ) produced gastrointestinal toxicity resulting in maternal weight loss and an increased incidence of abortion, but no teratogenicity was observed at either dose level. After intravenous administration of doses up to 20 mg/kg (approximately 0.3-times the highest recommended therapeutic dose based upon mg/m 2 ) no maternal toxicity was produced and no embryotoxicity or teratogenicity was observed. (See WARNINGS .)
Nursing Mothers: Ciprofloxacin is excreted in human milk. The amount of ciprofloxacin absorbed by the nursing infant is unknown. Because of the potential for serious adverse reactions in infants nursing from mothers taking ciprofloxacin, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use: Ciprofloxacin, like other quinolones, causes arthropathy and histological changes in weight-bearing joints of juvenile animals resulting in lameness. (See ANIMAL PHARMACOLOGY .)
Inhalational Anthrax (Post-Exposure)
Ciprofloxacin is indicated in pediatric patients for inhalational anthrax (post-exposure). The risk-benefit assessment indicates that administration of ciprofloxacin to pediatric patients is appropriate. For information regarding pediatric dosing in inhalational anthrax (post-exposure), see DOSAGE AND ADMINISTRATION and INHALATIONAL ANTHRAX - ADDITIONAL INFORMATION .
Complicated Urinary Tract Infection and Pyelonephritis
Ciprofloxacin is indicated for the treatment of complicated urinary tract infections and pyelonephritis due to Escherichia coli . Although effective in clinical trials, ciprofloxacin is not a drug of first choice in the pediatric population due to an increased incidence of adverse events compared to the controls, including those related to joints and/or surrounding tissues. The rates of these events in pediatric patients with complicated urinary tract infection and pyelonephritis within six weeks of follow-up were 9.3% (31/335) versus 6.0% (21/349) for control agents. The rates of these events occurring at any time up to the one year follow-up were 13.7% (46/335) and 9.5% (33/349), respectively. The rate of all adverse events regardless of drug relationship at six weeks was 41% (138/335) in the ciprofloxacin arm compared to 31% (109/349) in the control arm. (See ADVERSE REACTIONS and CLINICAL STUDIES .)
Cystic Fibrosis
Short-term safety data from a single trial in pediatric cystic fibrosis patients are available. In a randomized, double-blind clinical trial for the treatment of acute pulmonary exacerbations in cystic fibrosis patients (ages 5-17 years), 67 patients received ciprofloxacin I.V. 10 mg/kg/dose q8h for one week followed by ciprofloxacin tablets 20 mg/kg/dose q12h to complete 10-21 days treatment and 62 patients received the combination of ceftazidime I.V. 50 mg/kg/dose q8h and tobramycin I.V. 3 mg/kg/dose q8h for a total of 10-21 days. Patients less than 5 years of age were not studied. Safety monitoring in the study included periodic range of motion examinations and gait assessments by treatment-blinded examiners. Patients were followed for an average of 23 days after completing treatment (range 0-93 days). This study was not designed to determine long term effects and the safety of repeated exposure to ciprofloxacin.
Musculoskeletal adverse events in patients with cystic fibrosis were reported in 22% of the patients in the ciprofloxacin group and 21% in the comparison group. Decreased range of motion was reported in 12% of the subjects in the ciprofloxacin group and 16% in the comparison group. Arthralgia was reported in 10% of the patients in the ciprofloxacin group and 11% in the comparison group. Other adverse events were similar in nature and frequency between treatment arms. One of sixty-seven patients developed arthritis of the knee nine days after a ten day course of treatment with ciprofloxacin. Clinical symptoms resolved, but an MRI showed knee effusion without other abnormalities eight months after treatment. However, the relationship of this event to the patient's course of ciprofloxacin can not be definitively determined, particularly since patients with cystic fibrosis may develop arthralgias/arthritis as part of their underlying disease process.
Geriatric Use: In a retrospective analysis of 23 multiple-dose controlled clinical trials of ciprofloxacin encompassing over 3500 ciprofloxacin treated patients, 25% of patients were greater than or equal to 65 years of age and 10% were greater than or equal to 75 years of age. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals on any drug therapy cannot be ruled out. Ciprofloxacin is known to be substantially excreted by the kidney, and the risk of adverse reactions may be greater in patients with impaired renal function. No alteration of dosage is necessary for patients greater than 65 years of age with normal renal function. However, since some older individuals experience reduced renal function by virtue of their advanced age, care should be taken in dose selection for elderly patients, and renal function monitoring may be useful in these patients. (See CLINICAL PHARMACOLOGY and DOSAGE AND ADMINISTRATION .)
ADVERSE REACTIONS
Adverse Reactions in Adult Patients: During clinical investigations with oral and parenteral ciprofloxacin, 49,038 patients received courses of the drug. Most of the adverse events reported were described as only mild or moderate in severity, abated soon after the drug was discontinued, and required no treatment. Ciprofloxacin was discontinued because of an adverse event in 1.8% of intravenously treated patients.
The most frequently reported drug related events, from clinical trials of all formulations, all dosages, all drug-therapy durations, and for all indications of ciprofloxacin therapy were nausea (2.5%), diarrhea (1.6%), liver function tests abnormal (1.3%), vomiting (1.0%), and rash (1.0%).
In clinical trials the following events were reported, regardless of drug relationship, in greater than 1% of patients treated with intravenous ciprofloxacin: nausea, diarrhea, central nervous system disturbance, local I.V. site reactions, liver function tests abnormal, eosinophilia, headache, restlessness, and rash. Many of these events were described as only mild or moderate in severity, abated soon after the drug was discontinued, and required no treatment. Local I.V. site reactions are more frequent if the infusion time is 30 minutes or less. These may appear as local skin reactions which resolve rapidly upon completion of the infusion. Subsequent intravenous administration is not contraindicated unless the reactions recur or worsen.
Additional medically important events, without regard to drug relationship or route of administration, that occurred in 1% or less of ciprofloxacin patients are listed below:
BODY AS A WHOLE: abdominal pain/discomfort, foot pain, pain, pain in extremities
CARDIOVASCULAR: cardiovascular collapse, cardiopulmonary arrest, myocardial infarction, arrhythmia, tachycardia, palpitation, cerebral thrombosis, syncope, cardiac murmur, hypertension, hypotension, angina pectoris, atrial flutter, ventricular ectopy, (thrombo)-phlebitis, vasodilation, migraine
CENTRAL NERVOUS SYSTEM: convulsive seizures, paranoia, toxic psychosis, depression, dysphasia, phobia, depersonalization, manic reaction, unresponsiveness, ataxia, confusion, hallucinations, dizziness, lightheadedness, paresthesia, anxiety, tremor, insomnia, nightmares, weakness, drowsiness, irritability, malaise, lethargy, abnormal gait, grand mal convulsion, anorexia
GASTROINTESTINAL: ileus, jaundice, gastrointestinal bleeding, C. difficile associated diarrhea, pseudomembranous colitis, pancreatitis, hepatic necrosis, intestinal perforation, dyspepsia, epigastric pain, constipation, oral ulceration, oral candidiasis, mouth dryness, anorexia, dysphagia, flatulence, hepatitis, painful oral mucosa
HEMIC/LYMPHATIC: agranulocytosis, prolongation of prothrombin time, lymphadenopathy, petechia
METABOLIC/NUTRITIONAL: amylase increase, lipase increase
MUSCULOSKELETAL: arthralgia, jaw, arm or back pain, joint stiffness, neck and chest pain, achiness, flare up of gout, myasthenia gravis
RENAL/UROGENITAL: renal failure, interstitial nephritis, nephritis, hemorrhagic cystitis, renal calculi, frequent urination, acidosis, urethral bleeding, polyuria, urinary retention, gynecomastia, candiduria, vaginitis, breast pain. Crystalluria, cylindruria, hematuria and albuminuria have also been reported.
RESPIRATORY: respiratory arrest, pulmonary embolism, dyspnea, laryngeal or pulmonary edema, respiratory distress, pleural effusion, hemoptysis, epistaxis, hiccough, bronchospasm
SKIN/HYPERSENSITIVITY: allergic reactions, anaphylactic reactions including life-threatening anaphylactic shock, erythema multiforme/Stevens-Johnson syndrome, exfoliative dermatitis, toxic epidermal necrolysis, vasculitis, angioedema, edema of the lips, face, neck, conjunctivae, hands or lower extremities, purpura, fever, chills, flushing, pruritus, urticaria, cutaneous candidiasis, vesicles, increased perspiration, hyperpigmentation, erythema nodosum, thrombophlebitis, burning, paresthesia, erythema, swelling, photosensitivity (See WARNINGS .)
SPECIAL SENSES: decreased visual acuity, blurred vision, disturbed vision (flashing lights, change in color perception, overbrightness of lights, diplopia), eye pain, anosmia, hearing loss, tinnitus, nystagmus, chromatopsia, a bad taste
In several instances, nausea, vomiting, tremor, irritability, or palpitation were judged by investigators to be related to elevated serum levels of theophylline possibly as a result of drug interaction with ciprofloxacin.
In randomized, double-blind controlled clinical trials comparing ciprofloxacin (I.V. and I.V./P.O. sequential) with intravenous beta-lactam control antibiotics, the CNS adverse event profile of ciprofloxacin was comparable to that of the control drugs.
Adverse Reactions in Pediatric Patients: Ciprofloxacin, administered I.V. and/or orally, was compared to a cephalosporin for treatment of complicated urinary tract infections (cUTI) or pyelonephritis in pediatric patients 1 to 17 years of age (mean age of 6 ± 4 years). The trial was conducted in the US, Canada, Argentina, Peru, Costa Rica, Mexico, South Africa, and Germany. The duration of therapy was 10 to 21 days (mean duration of treatment was 11 days with a range of 1 to 88 days). The primary objective of the study was to assess musculoskeletal and neurological safety within 6 weeks of therapy and through one year of follow-up in the 335 ciprofloxacin- and 349 comparator-treated patients enrolled.
An Independent Pediatric Safety Committee (IPSC) reviewed all cases of musculoskeletal adverse events as well as all patients with an abnormal gait or abnormal joint exam (baseline or treatment-emergent). These events were evaluated in a comprehensive fashion and included such conditions as arthralgia, abnormal gait, abnormal joint exam, joint sprains, leg pain, back pain, arthrosis, bone pain, pain, myalgia, arm pain, and decreased range of motion in a joint. The affected joints included: knee, elbow, ankle, hip, wrist, and shoulder. Within 6 weeks of treatment initiation, the rates of these events were 9.3% (31/335) in the ciprofloxacin-treated group versus 6.0 % (21/349) in comparator-treated patients. The majority of these events were mild or moderate in intensity. All musculoskeletal events occurring by 6 weeks resolved (clinical resolution of signs and symptoms), usually within 30 days of end of treatment. Radiological evaluations were not routinely used to confirm resolution of the events. The events occurred more frequently in ciprofloxacin-treated patients than control patients, regardless of whether they received I.V. or oral therapy. Ciprofloxacin-treated patients were more likely to report more than one event and on more than one occasion compared to control patients. These events occurred in all age groups and the rates were consistently higher in the ciprofloxacin group compared to the control group. At the end of 1 year, the rate of these events reported at any time during that period was 13.7% (46/335) in the ciprofloxacin-treated group versus 9.5% (33/349) comparator-treated patients.
An adolescent female discontinued ciprofloxacin for wrist pain that developed during treatment. An MRI performed 4 weeks later showed a tear in the right ulnar fibrocartilage. A diagnosis of overuse syndrome secondary to sports activity was made, but a contribution from ciprofloxacin cannot be excluded. The patient recovered by 4 months without surgical intervention.
Findings Involving Joint or Peri-articular Tissues as
Assessed by the IPSCCiprofloxacin Comparator All Patients (within
6 weeks)31/335 (9.3%) 21/349 (6.0%) 95% Confidence Interval *(-0.8%, +7.2%) Age Group>/= 12 months < 24 months1/36 (2.8%) 0/41 >/= 2 years < 6 years5/124 (4.0%) 3/118 (2.5%) >/= 6 years < 12 years18/143 (12.6%) 12/153 (7.8%) >/= 12 years to
17 years7/32 (21.9%) 6/37 (16.2 %) All Patients (within
1 year)46/335 (13.7%) 33/349 (9.5%) 95% Confidence Interval *(-0.6%, +9.1%) *The study was designed to demonstrate that the arthropathy rate for the ciprofloxacin group did not exceed that of the control group by more than + 6%. At both the 6 week and 1 year evaluations, the 95% confidence interval indicated that it could not be concluded that the ciprofloxacin group had findings comparable to the control group.The incidence rates of neurological events within 6 weeks of treatment initiation were 3% (9/335) in the ciprofloxacin group versus 2% (7/349) in the comparator group and included dizziness, nervousness, insomnia, and somnolence.
In this trial, the overall incidence rates of adverse events regardless of relationship to study drug and within 6 weeks of treatment initiation were 41% (138/335) in the ciprofloxacin group versus 31% (109/349) in the comparator group. The most frequent events were gastrointestinal: 15% (50/335) of ciprofloxacin patients compared to 9% (31/349) of comparator patients. Serious adverse events were seen in 7.5% (25/335) of ciprofloxacin-treated patients compared to 5.7% (20/349) of control patients. Discontinuation of drug due to an adverse event was observed in 3% (10/335) of ciprofloxacin-treated patients versus 1.4% (5/349) of comparator patients. Other adverse events that occurred in at least 1% of ciprofloxacin patients were diarrhea 4.8%, vomiting 4.8%, abdominal pain 3.3%, accidental injury 3.0%, rhinitis 3.0%, dyspepsia 2.7%, nausea 2.7%, fever 2.1%, asthma 1.8% and rash 1.8%.
In addition to the events reported in pediatric patients in clinical trials, it should be expected that events reported in adults during clinical trials or post-marketing experience may also occur in pediatric patients.
Post-Marketing Adverse Events: The following adverse events have been reported from worldwide marketing experience with quinolones, including ciprofloxacin. Because these events are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. Decisions to include these events in labeling are typically based on one or more of the following factors: (1) seriousness of the event, (2) frequency of the reporting, or (3) strength of causal connection to the drug.
Agitation, agranulocytosis, albuminuria, anosmia, candiduria, cholesterol elevation (serum), confusion, constipation, delirium, dyspepsia, dysphagia, erythema multiforme, exfoliative dermatitis, fixed eruption, flatulence, glucose elevation (blood), hemolytic anemia, hepatic failure, hepatic necrosis, hyperesthesia, hypertonia, hypesthesia, hypotension (postural), jaundice, marrow depression (life threatening), methemoglobinemia, moniliasis (oral, gastrointestinal, vaginal), myalgia, myasthenia, myasthenia gravis (possible exacerbation), myoclonus, nystagmus, pancreatitis, pancytopenia (life threatening or fatal outcome), peripheral neuropathy, phenytoin alteration (serum), potassium elevation (serum), prothrombin time prolongation or decrease, pseudomembranous colitis (The onset of pseudomembranous colitis symptoms may occur during or after antimicrobial treatment.), psychosis (toxic), renal calculi, serum sickness like reaction, Stevens-Johnson syndrome, taste loss, tendinitis, tendon rupture, torsade de pointesde pointes, toxic epidermal necrolysis (Lyell's Syndrome), triglyceride elevation (serum), twitching, vaginal candidiasis, and vasculitis. (See PRECAUTIONS .)
Adverse events were also reported by persons who received ciprofloxacin for anthrax post-exposure prophylaxis following the anthrax bioterror attacks of October 2001 (See also INHALATIONAL ANTHRAX - ADDITIONAL INFORMATION ).
Adverse Laboratory Changes: The most frequently reported changes in laboratory parameters with intravenous ciprofloxacin therapy, without regard to drug relationship are listed below:
Hepatic--elevations of AST (SGOT), ALT (SGPT), alkaline phosphatase, LDH, and serum bilirubin
Hematologic--elevated eosinophil and platelet counts, decreased platelet counts, hemoglobin and/or hematocrit
Renal--elevations of serum creatinine, BUN, and uric acid
Other--elevations of serum creatine phosphokinase, serum theophylline (in patients receiving theophylline concomitantly), blood glucose, and triglycerides
Other changes occurring infrequently were: decreased leukocyte count, elevated atypical lymphocyte count, immature WBCs, elevated serum calcium, elevation of serum gamma-glutamyl transpeptidase ((gamma) GT), decreased BUN, decreased uric acid, decreased total serum protein, decreased serum albumin, decreased serum potassium, elevated serum potassium, elevated serum cholesterol. Other changes occurring rarely during administration of ciprofloxacin were: elevation of serum amylase, decrease of blood glucose, pancytopenia, leukocytosis, elevated sedimentation rate, change in serum phenytoin, decreased prothrombin time, hemolytic anemia, and bleeding diathesis.
OVERDOSAGE
In the event of acute overdosage, the patient should be carefully observed and given supportive treatment, including monitoring of renal function. Adequate hydration must be maintained. Only a small amount of ciprofloxacin (< 10%) is removed from the body after hemodialysis or peritoneal dialysis.
In mice, rats, rabbits and dogs, significant toxicity including tonic/clonic convulsions was observed at intravenous doses of ciprofloxacin between 125 and 300 mg/kg.
DOSAGE AND ADMINISTRATION - ADULTS
CIPRO I.V. should be administered to adults by intravenous infusion over a period of 60 minutes at dosages described in the Dosage Guidelines table. Slow infusion of a dilute solution into a larger vein will minimize patient discomfort and reduce the risk of venous irritation. (See Preparation of CIPRO I.V. for Administration section.)
The determination of dosage for any particular patient must take into consideration the severity and nature of the infection, the susceptibility of the causative microorganism, the integrity of the patient's host-defense mechanisms, and the status of renal and hepatic function.
ADULT DOSAGE GUIDELINES Infection **/*Severity Dose Frequency Usual Duration Urinary TractMild/Moderate
Severe/Complicated200 mg
400 mgq12h
q12h7-14 Days
7-14 DaysLower
Respiratory TractMild/Moderate
Severe/Complicated400 mg
400 mgq12h
q8h7-14 Days
7-14 DaysNosocomial
PneumoniaMild/Moderate/Severe 400 mg q8h 10-14 Days Skin and
Skin StructureMild/Moderate
Severe/Complicated400 mg
400 mgq12h
q8h7-14 Days
7-14 DaysBone and JointMild/Moderate
Severe/Complicated400 mg
400 mgq12h
q8h>/= 4-6 Weeks
>/= 4-6 WeeksIntra-Abdominal *Complicated 400 mg q12h 7-14 Days Acute SinusitisMild/Moderate 400 mg q12h 10 Days Chronic Bacterial
ProstatitisMild/Moderate 400 mg q12h 28 Days Empirical Therapy
in Febrile
Neutropenic
PatientsSevere
Ciprofloxacin
+
Piperacillin
400 mg
50 mg/kg
Not to exceed
24 g/day
q8h
q4h
7-14 DaysInhalational anthrax
(post-exposure) **400 mg q12h 60 Days *used in conjunction with metronidazole. (See product labeling for prescribing information.)**/* DUE TO THE DESIGNATED PATHOGENS (See INDICATIONS AND USAGE .)**Drug administration should begin as soon as possible after suspected or confirmed exposure. This indication is based on a surrogate endpoint, ciprofloxacin serum concentrations achieved in humans, reasonably likely to predict clinical benefit. 4 For a discussion of ciprofloxacin serum concentrations in various human populations, see INHALATIONAL ANTHRAX - ADDITIONAL INFORMATION . Total duration of ciprofloxacin administration (I.V. or oral) for inhalational anthrax (post-exposure) is 60 days.CIPRO I.V. should be administered by intravenous infusion over a period of 60 minutes.
Conversion of I.V. to Oral Dosing in Adults: CIPRO Tablets and CIPRO Oral Suspension for oral administration are available. Parenteral therapy may be switched to oral CIPRO when the condition warrants, at the discretion of the physician. (See CLINICAL PHARMACOLOGY and table below for the equivalent dosing regimens.)
Equivalent AUC Dosing Regimens CIPRO Oral DosageEquivalent CIPRO
I.V. Dosage250 mg Tablet q 12 h200 mg I.V. q 12 h 500 mg Tablet q 12 h400 mg I.V. q 12 h 750 mg Tablet q 12 h400 mg I.V. q 8 h Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration.
Adults with Impaired Renal Function: Ciprofloxacin is eliminated primarily by renal excretion; however, the drug is also metabolized and partially cleared through the biliary system of the liver and through the intestine. These alternative pathways of drug elimination appear to compensate for the reduced renal excretion in patients with renal impairment. Nonetheless, some modification of dosage is recommended for patients with severe renal dysfunction. The following table provides dosage guidelines for use in patients with renal impairment:
RECOMMENDED STARTING AND MAINTENANCE DOSES
FOR PATIENTS WITH IMPAIRED RENAL FUNCTIONCreatinine Clearance (mL/min) Dosage > 30 See usual dosage. 5-29 200-400 mg q 18-24 hr When only the serum creatinine concentration is known, the following formula may be used to estimate creatinine clearance:
Men: Creatinine clearance (mL/min)= Weight (kg) × (140 -age)
72 × serum creatinine (mg/dL)Women: 0.85 × the value calculated for men.The serum creatinine should represent a steady state of renal function.
For patients with changing renal function or for patients with renal impairment and hepatic insufficiency, careful monitoring is suggested.
DOSAGE AND ADMINISTRATION - PEDIATRICS
CIPRO I.V. should be administered as described in the Dosage Guidelines table. An increased incidence of adverse events compared to controls, including events related to joints and/or surrounding tissues, has been observed. (See ADVERSE REACTIONS and CLINICAL STUDIES .)
Dosing and initial route of therapy (i.e., I.V. or oral) for complicated urinary tract infection or pyelonephritis should be determined by the severity of the infection. In the clinical trial, pediatric patients with moderate to severe infection were initiated on 6 to 10 mg/kg I.V. every 8 hours and allowed to switch to oral therapy (10 to 20 mg/kg every 12 hours), at the discretion of the physician.
PEDIATRIC DOSAGE GUIDELINES Infection Route of Administration Dose
(mg/kg)Frequency Total Duration Complicated Urinary Tract
or
Pyelonephritis (patients from 1 to 17 years of age)Intravenous 6 to 10 mg/kg
(maximum 400 mg per dose; not to be exceeded even in patients weighing
> 51 kg)Every 8 hours 10-21 days * Oral 10 mg/kg to 20 mg/kg
(maximum 750 mg per dose; not to be exceeded even in patients weighing
> 51 kg)Every 12 hours Inhalational Anthrax (Post-Exposure) ** Intravenous 10 mg/kg
(maximum 400 mg per dose)Every 12 hours 60 days Oral 15 mg/kg
(maximum 500 mg per dose)Every 12 hours * The total duration of therapy for complicated urinary tract infection and pyelonephritis in the clinical trial was determined by the physician. The mean duration of treatment was 11 days (range 10 to 21 days). ** Drug administration should begin as soon as possible after suspected or confirmed exposure to Bacillus anthracis spores. This indication is based on a surrogate endpoint, ciprofloxacin serum concentrations achieved in humans, reasonably likely to predict clinical benefit. 4 For a discussion of ciprofloxacin serum concentrations in various human populations, see INHALATIONAL ANTHRAX - ADDITIONAL INFORMATION . Pediatric patients with moderate to severe renal insufficiency were excluded from the clinical trial of complicated urinary tract infection and pyelonephritis. No information is available on dosing adjustments necessary for pediatric patients with moderate to severe renal insufficiency (i.e., creatinine clearance of < 50 mL/min/1.73m 2 ).
Preparation of CIPRO I.V. for Administration
PHARMACY BULK PACKAGE: The pharmacy bulk package is a single-entry container of a sterile preparation for parenteral use that contains many single doses. It contains ciprofloxacin as a 1% aqueous solution concentrate. The contents are intended for use in a pharmacy admixture program and are restricted to the preparation of admixtures for intravenous infusion. THE CLOSURE SHALL BE PENETRATED ONLY ONE TIME with a suitable sterile transfer set or dispensing device which allows measured dispensing of the contents.
The pharmacy bulk package is to be used only in a suitable work area such as laminar flow hood or an equivalent clean air or compounding area. THIS PREPARATION MUST BE DILUTED BEFORE USE. The intravenous dose should be prepared by aseptically withdrawing the CIPRO I.V. concentrate from the pharmacy bulk package and diluting the appropriate volume with a suitable intravenous solution to a final concentration of 0.5-2mg/mL. See COMPATIBILITY AND STABILITY .) The resulting solution should be infused over a period of 60 minutes by direct infusion or through a Y-type intravenous infusion set which may already be in place.
If the Y-type or "piggyback" method of administration is used, it is advisable to discontinue temporarily the administration of any other solutions during the infusion of CIPRO I.V. If the concomitant use of CIPRO I.V. and another drug is necessary each drug should be given separately in accordance with the recommended dosage and route of administration for each drug.
COMPATIBILITY AND STABILITY
Ciprofloxacin injection 1% (10 mg/mL), when diluted with the following intravenous solutions to concentrations of 0.5 to 2.0 mg/mL, is stable for up to 14 days at refrigerated or room temperature storage.
0.9% Sodium Chloride Injection, USP
5% Dextrose Injection, USP
Sterile Water for Injection
10% Dextrose for Injection
5% Dextrose and 0.225% Sodium Chloride for Injection
5% Dextrose and 0.45% Sodium Chloride for Injection
Lactated Ringer's for Injection
HOW SUPPLIED
CIPRO I.V. (ciprofloxacin) is available as a clear, colorless to slightly yellowish solution supplied in the pharmacy bulk package as follows:
CONTAINERSIZE STRENGTH NDC NUMBER Pharmacy Bulk Package:120 mL 1200 mg, 1% 0026-8566-65 CIPRO I.V. (ciprofloxacin) is also available as follows:
VIAL: manufactured by Bayer Pharmaceuticals Corporation by Bayer HealthCare LLC, Shawnee, Kanas.SIZE STRENGTH NDC NUMBER 20 mL 200 mg, 1% 0085-1763-03 40 mL 400 mg, 1% 0085-1731-01 FLEXIBLE CONTAINER: manufactured for Bayer Pharmaceuticals Corporation by Hospira, Inc., Lake Forest, IL 60045.SIZE STRENGTH NDC NUMBER 100 mL 5% Dextrose 200 mg, 0.2% 0085-1755-02 200 mL 5% Dextrose 400 mg, 0.2% 0085-1741-02 FLEXIBLE CONTAINER: manufactured for Bayer Pharmaceuticals Corporation by Baxter Healthcare Corporation, Deerfield, IL 60015.SIZE STRENGTH NDC NUMBER 100 mL 5% Dextrose 200 mg, 0.2% 0085-1781-01 200 mL 5% Dextrose 400 mg, 0.2% 0085-1762-01
STORAGE
Pharmacy Bulk Package: Store between 5-30°C (41-86°F).
Protect from light, avoid excessive heat, protect from freezing.
Ciprofloxacin is also available as CIPRO (ciprofloxacin HCl)Tablets 250, 500, and 750 mg and CIPRO (ciprofloxacin * ) 5% and 10% Oral Suspension.
* Does not comply with USP with regards to "loss on drying" and "residue on ignition".
ANIMAL PHARMACOLOGY
Ciprofloxacin and other quinolones have been shown to cause arthropathy in immature animals of most species tested. (See WARNINGS .) Damage of weight bearing joints was observed in juvenile dogs and rats. In young beagles, 100 mg/kg ciprofloxacin, given daily for 4 weeks, caused degenerative articular changes of the knee joint. At 30 mg/kg, the effect on the joint was minimal. In a subsequent study in young beagle dogs, oral ciprofloxacin doses of 30 mg/kg and 90 mg/kg ciprofloxacin (approximately 1.3- and 3.5-times the pediatric dose based upon comparative plasma AUCs) given daily for 2 weeks caused articular changes which were still observed by histopathology after a treatment-free period of 5 months. At 10 mg/kg (approximately 0.6-times the pediatric dose based upon comparative plasma AUCs), no effects on joints were observed. This dose was also not associated with arthrotoxicity after an additional treatment-free period of 5 months. In another study, removal of weight bearing from the joint reduced the lesions but did not totally prevent them.
Crystalluria, sometimes associated with secondary nephropathy, occurs in laboratory animals dosed with ciprofloxacin. This is primarily related to the reduced solubility of ciprofloxacin under alkaline conditions, which predominate in the urine of test animals; in man, crystalluria is rare since human urine is typically acidic. In rhesus monkeys, crystalluria without nephropathy was noted after single oral doses as low as 5 mg/kg (approximately 0.07-times the highest recommended therapeutic dose based upon mg/m 2 ). After 6 months of intravenous dosing at 10 mg/kg/day, no nephropathological changes were noted; however, nephropathy was observed after dosing at 20 mg/kg/day for the same duration (approximately 0.2-times the highest recommended therapeutic dose based upon mg/m 2 ).
In dogs, ciprofloxacin administered at 3 and 10 mg/kg by rapid intravenous injection (15 sec.) produces pronounced hypotensive effects. These effects are considered to be related to histamine release because they are partially antagonized by pyrilamine, an antihistamine. In rhesus monkeys, rapid intravenous injection also produces hypotension, but the effect in this species is inconsistent and less pronounced.
In mice, concomitant administration of nonsteroidal anti-inflammatory drugs, such as phenylbutazone and indomethacin, with quinolones has been reported to enhance the CNS stimulatory effect of quinolones.
Ocular toxicity, seen with some related drugs, has not been observed in ciprofloxacin-treated animals.
INHALATIONAL ANTHRAX - ADDITIONAL INFORMATION
The mean serum concentrations of ciprofloxacin associated with a statistically significant improvement in survival in the rhesus monkey model of inhalational anthrax are reached or exceeded in adult and pediatric patients receiving oral and intravenous regimens. (See DOSAGE AND ADMINISTRATION .) Ciprofloxacin pharmacokinetics have been evaluated in various human populations. The mean peak serum concentration achieved at steady-state in human adults receiving 500 mg orally every 12 hours is 2.97 µg/mL, and 4.56 µg/mL following 400 mg intravenously every 12 hours. The mean trough serum concentration at steady-state for both of these regimens is 0.2 µg/mL. In a study of 10 pediatric patients between 6 and 16 years of age, the mean peak plasma concentration achieved is 8.3 µg/mL and trough concentrations range from 0.09 to 0.26 µg/mL, following two 30-minute intravenous infusions of 10 mg/kg administered 12 hours apart. After the second intravenous infusion patients switched to 15 mg/kg orally every 12 hours achieve a mean peak concentration of 3.6 µg/mL after the initial oral dose. Long-term safety data, including effects on cartilage, following the administration of ciprofloxacin to pediatric patients are limited. (For additional information, see PRECAUTIONS , Pediatric Use .) Ciprofloxacin serum concentrations achieved in humans serve as a surrogate endpoint reasonably likely to predict clinical benefit and provide the basis for this indication. 4
A placebo-controlled animal study in rhesus monkeys exposed to an inhaled mean dose of 11 LD 50 (~5.5 × 10 5 ) spores (range 5-30 LD 50 ) of B. anthracis was conducted. The minimal inhibitory concentration (MIC) of ciprofloxacin for the anthrax strain used in this study was 0.08 µg/mL. In the animals studied, mean serum concentrations of ciprofloxacin achieved at expected T max (1 hour post-dose) following oral dosing to steady-state ranged from 0.98 to 1.69 µg/mL. Mean steady-state trough concentrations at 12 hours post-dose ranged from 0.12 to 0.19 µg/mL. 5 . Mortality due to anthrax for animals that received a 30-day regimen of oral ciprofloxacin beginning 24 hours post-exposure was significantly lower (1/9), compared to the placebo group (9/10) [p=0.001]. The one ciprofloxacin-treated animal that died of anthrax did so following the 30-day drug administration period. 6
More than 9300 persons were recommended to complete a minimum of 60 days of antibiotic prophylaxis against possible inhalational exposure to B. anthracis during 2001. Ciprofloxacin was recommended to most of those individuals for all or part of the prophylaxis regimen. Some persons were also given anthrax vaccine or were switched to alternative antibiotics. No one who received ciprofloxacin or other therapies as prophylactic treatment subsequently developed inhalational anthrax. The number of persons who received ciprofloxacin as all or part of their post-exposure prophylaxis regimen is unknown.
Among the persons surveyed by the Centers for Disease Control and Prevention, over 1000 reported receiving ciprofloxacin as sole post-exposure prophylaxis for inhalational anthrax. Gastrointestinal adverse events (nausea, vomiting, diarrhea, or stomach pain), neurological adverse events (problems sleeping, nightmares, headache, dizziness or lightheadedness) and musculoskeletal adverse events (muscle or tendon pain and joint swelling or pain) were more frequent than had been previously reported in controlled clinical trials. This higher incidence, in the absence of a control group, could be explained by a reporting bias, concurrent medical conditions, other concomitant medications, emotional stress or other confounding factors, and/or a longer treatment period with ciprofloxacin. Because of these factors and limitations in the data collection, it is difficult to evaluate whether the reported symptoms were drug-related.
CLINICAL STUDIES
EMPIRICAL THERAPY IN ADULT FEBRILE NEUTROPENIC PATIENTS
The safety and efficacy of ciprofloxacin, 400 mg I.V. q 8h, in combination with piperacillin sodium, 50 mg/kg I.V. q 4h, for the empirical therapy of febrile neutropenic patients were studied in one large pivotal multicenter, randomized trial and were compared to those of tobramycin, 2 mg/kg I.V. q 8h, in combination with piperacillin sodium, 50 mg/kg I.V. q 4h.
Clinical response rates observed in this study were as follows:
OutcomesCiprofloxacin/Piperacillin
N = 233
Success (%)Tobramycin/Piperacillin
N = 237
Success (%)Clinical Resolution of
Initial Febrile Episode
with No Modifications of
Empirical Regimen *63 (27.0%) 52 (21.9%) Clinical Resolution of
Initial Febrile Episode
Including Patients with
Modifications of
Empirical Regimen187 (80.3%) 185 (78.1%) Overall Survival224 (96.1%) 223 (94.1%) * To be evaluated as a clinical resolution, patients had to have: (1) resolution of fever; (2) microbiological eradication of infection (if an infection was microbiologically documented); (3) resolution of signs/symptoms of infection; and (4) no modification of empirical antibiotic regimen.Complicated Urinary Tract Infection and Pyelonephritis - Efficacy in Pediatric Patients:
NOTE: Although effective in clinical trials, ciprofloxacin is not a drug of first choice in the pediatric population due to an increased incidence of adverse events compared to controls, including events related to joints and/or surrounding tissues.
Ciprofloxacin, administered I.V. and/or orally, was compared to a cephalosporin for treatment of complicated urinary tract infections (cUTI) and pyelonephritis in pediatric patients 1 to 17 years of age (mean age of 6 ± 4 years). The trial was conducted in the US, Canada, Argentina, Peru, Costa Rica, Mexico, South Africa, and Germany. The duration of therapy was 10 to 21 days (mean duration of treatment was 11 days with a range of 1 to 88 days). The primary objective of the study was to assess musculoskeletal and neurological safety.
Patients were evaluated for clinical success and bacteriological eradication of the baseline organism(s) with no new infection or superinfection at 5 to 9 days post-therapy (Test of Cure or TOC). The Per Protocol population had a causative organism(s) with protocol specified colony count(s) at baseline, no protocol violation, and no premature discontinuation or loss to follow-up (among other criteria).
The clinical success and bacteriologic eradication rates in the Per Protocol population were similar between ciprofloxacin and the comparator group as shown below.
Clinical Success and Bacteriologic Eradication at Test of Cure
(5 to 9 Days Post-Therapy)CIPRO Comparator Randomized Patients337 352 Per Protocol Patients211 231 Clinical Response at 5 to 9 Days Post-Treatment95.7% (202/211) 92.6% (214/231) 95% CI [-1.3%, 7.3%] Bacteriologic Eradication by Patient at 5 to 9 Days Post-Treatment *84.4% (178/211) 78.3% (181/231) 95% CI [-1.3%, 13.1%] Bacteriologic Eradication of the Baseline Pathogen at 5 to 9 Days Post-TreatmentEscherichia coli156/178 (88%) 161/179 (90%) * Patients with baseline pathogen(s) eradicated and no new infections or superinfections/total number of patients. There were 5.5% (6/211) ciprofloxacin and 9.5% (22/231) comparator patients with superinfections or new infections. References:
- National Committee for Clinical Laboratory Standards, Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically - Fifth Edition. Approved Standard NCCLS Document M7-A5, Vol. 20, No. 2, NCCLS, Wayne, PA, January, 2000.
- National Committee for Clinical Laboratory Standards, Performance Standards for Antimicrobial Disk Susceptibility Tests - Seventh Edition. Approved Standard NCCLS Document M2-A7, Vol. 20, No. 1, NCCLS, Wayne, PA, January, 2000.
- Report presented at the FDA's Anti-Infective Drug and Dermatological Drug Products Advisory Committee Meeting, March 31, 1993, Silver Spring, MD. Report available from FDA, CDER, Advisors and Consultants Staff, HFD-21, 1901 Chapman Avenue, Room 200, Rockville, MD 20852, USA.
- 21 CFR 314.510 (Subpart H - Accelerated Approval of New Drugs for Life-Threatening Illnesses).
- Kelly DJ, et al. Serum concentrations of penicillin, doxycycline, and ciprofloxacin during prolonged therapy in rhesus monkeys. J Infect Dis 1992; 166: 1184-7.
- Friedlander AM, et al. Postexposure prophylaxis against experimental inhalational anthrax. J Infect Dis 1993; 167: 1239-42.
- Friedman J, Polifka J. Teratogenic effects of drugs: a resource for clinicians (TERIS). Baltimore, Maryland: Johns Hopkins University Press, 2000:149-195.
- Loebstein R, Addis A, Ho E, et al. Pregnancy outcome following gestational exposure to fluoroquinolones: a multicenter prospective controlled study. Antimicrob Agents Chemother. 1998;42(6): 1336-1339.
- Schaefer C, Amoura-Elefant E, Vial T, et al. Pregnancy outcome after prenatal quinolone exposure. Evaluation of a case registry of the European network of teratology information services (ENTIS). Eur J Obstet Gynecol Reprod Biol. 1996;69:83-89.
Bayer HealthCare
Manufactured for:
Bayer Pharmaceuticals Corporation
400 Morgan Lane
West Haven, CT 06516 USA
CIPRO is a registered trademark of Bayer Aktiengesellschaft and is used under license by Schering Corporation.
Rx Only
08709923, R.4 7/05 BAY q 3939
© 2005 Bayer Pharmaceuticals Corporation 12773
Printed In U.S.A.
Subscribe to the "News" RSS Feed 
TOP ۞
