-
Clindesse Vaginal Cream (Ther-Rx)
DESCRIPTION
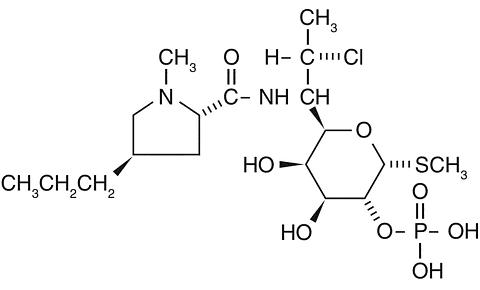
Clindamycin phosphate is a water soluble ester of the semi-synthetic antibiotic produced by a 7(S)-chloro-substitution of the 7(R)-hydroxyl group of the parent antibiotic lincomycin. The chemical name for clindamycin phosphate is methyl 7-chloro-6,7,8-trideoxy-6-(1-methyl- trans -4-propyl-L-2-pyrrolidinecarboxamido)-1-thio-L- threo - (alpha) - D-galacto -octopyranoside 2-(dihydrogen phosphate). It has a molecular weight of 504.96, and the molecular formula is C 18 H 34 CIN 2 O 8 PS. The structural formula is represented below:
Clindesse™ is a semi-solid, white cream, which contains clindamycin phosphate, USP, at a concentration equivalent to 20 mg clindamycin base per gram. The cream also contains edetate disodium, glycerol monoisostearate, lecithin, methylparaben, microcrystalline wax, mineral oil, polyglyceryl-3-oleate, propylparaben, purified water, silicon dioxide and sorbitol solution.
* Does not comply with the pH test of the USP monograph for clindamycin phosphate vaginal cream.CLINICAL PHARMACOLOGY
Pharmacokinetics
Following a single intravaginal application of Clindesse™ cream to twenty healthy women, the mean (range) AUC 0-inf and C max estimates were 175 (38.6 to 541) ng/mL·hr and 6.6 (0.8 to 39) ng/mL, respectively. The mean C max of clindamycin for Clindesse™ was approximately 0.3%, 0.1%, and 7.6% of that observed after the administration of a 150 mg Cleocin® oral capsule (2.5 [micro ]g/mL), a 600 mg Cleocin® intravenous injection (10.9 [micro ]g/mL), and a single dose of 100 mg of Cleocin® Vaginal Cream (86.5 ng/mL), respectively. The peak serum concentration of clindamycin was attained approximately 20 hours post dosing for Clindesse™ .
MICROBIOLOGY
Clindamycin inhibits bacterial protein synthesis at the level of the bacterial ribosome. The antibiotic binds preferentially to the 50S ribosomal subunit and affects the process of peptide chain initiation. Although clindamycin phosphate is inactive in vitro , rapid in vivo hydrolysis converts this compound to the antibacterially active clindamycin.
Culture and sensitivity testing of bacteria are not routinely performed to establish the diagnosis of bacterial vaginosis (see INDICATIONS AND USAGE ). Standard methodology for the susceptibility testing of the potential bacterial vaginosis pathogens, Gardnerella vaginalis, Mobiluncus spp., or Mycoplasma hominis , has not been defined. Nonetheless, clindamycin is an antimicrobial agent active in vitro against most strains of the following organisms that have been reported to be associated with bacterial vaginosis:
Bacteroides spp.
Gardnerella vaginalis
Mobiluncus spp.
Mycoplasma hominis
Peptostreptococcus spp.
INDICATIONS AND USAGE
Clindesse™ is indicated for the treatment of bacterial vaginosis (formerly referred to as Haemophilus vaginitis, Gardnerella vaginitis, nonspecific vaginitis, Corynebacterium vaginitis, or anaerobic vaginosis) in non-pregnant women. There are no adequate and well-controlled studies of Clindesse™ in pregnant women.
Note: For purposes of this indication, a clinical diagnosis of bacterial vaginosis is usually defined by the presence of a homogeneous vaginal discharge that (a) has a pH of greater than 4.5, (b) emits a "fishy" amine odor when mixed with a 10% KOH solution, and (c) contains clue cells on microscopic examination. Gram's stain results consistent with a diagnosis of bacterial vaginosis include (a) markedly reduced or absent Lactobacillus morphology, (b) predominance of Gardnerella morphotype, and (c) absent or few white blood cells.
Other pathogens commonly associated with vulvovaginitis, e.g., Trichomonas vaginalis, Chlamydia trachomatis , N. gonorrhoeae, Candida albicans, and Herpes simplex virus should be ruled out.
CONTRAINDICATIONS
Clindesse™ is contraindicated in individuals with a history of hypersensitivity to clindamycin, lincomycin, or any of the components of this vaginal cream. Clindesse™ is also contraindicated in individuals with a history of regional enteritis, ulcerative colitis, or a history of "antibiotic-associated" colitis.
WARNINGS
This cream contains mineral oil that may weaken latex or rubber products such as condoms or vaginal contraceptive diaphragms. Therefore, the use of such barrier contraceptives is not recommended concurrently or for 5 days following treatment with Clindesse™. During this time period, condoms may not be reliable for preventing pregnancy or for protecting against transmission of HIV and other sexually transmitted diseases.
Pseudomembranous colitis has been reported with nearly all antibacterial agents, including clindamycin, and may range in severity from mild to life-threatening. Orally and parenterally administered clindamycin has been associated with severe colitis which may end fatally. Diarrhea, bloody diarrhea, and colitis (including pseudomembranous colitis) have been reported with the use of orally and parenterally administered clindamycin, as well as with topical (dermal) formulations of clindamycin. Therefore, it is important to consider this diagnosis in patients who present with diarrhea subsequent to the administration of clindamycin, even though there is minimal systemic absorption of clindamycin from the vagina with administration of Clindesse™ cream (see CLINICAL PHARMACOLOGY ).
Treatment with antibacterial agents alters the normal flora of the colon and may permit overgrowth of clostridia. Studies indicate that a toxin produced by Clostridium [not ]difficile is a primary cause of "antibiotic-associated" colitis
After the diagnosis of pseudomembranous colitis has been established, therapeutic measures should be initiated. Mild cases of pseudomembranous colitis usually respond to discontinuation of the drug alone. In moderate to severe cases, consideration should be given to management with fluids and electrolytes, protein supplementation, and treatment with an antibacterial drug clinically effective against Clostridium difficile colitis. Onset of pseudomembranous colitis symptoms may occur during or after antimicrobial treatment.
PRECAUTIONS
General
Clindesse™ contains ingredients that will cause burning and irritation of the eye. In the event of accidental contact with the eye, rinse the eye with copious amounts of cool tap water and consult your physician.
The use of clindamycin may result in the overgrowth of nonsusceptible organisms in the vagina. In clinical studies involving a total of 368 women who received a single administration of Clindesse™, a vaginal fungal infection was diagnosed in 14.1% of women throughout the studies.
Information for the Patient
The patient should be instructed not to engage in vaginal intercourse, or use other vaginal products (such as tampons or douches) during treatment with this product.
The patient should also be advised that this cream contains mineral oil that may weaken latex or rubber products such as condoms or vaginal contraceptive diaphragms. Therefore, the use of such barrier contraceptives is not recommended concurrently or for 5 days following treatment with Clindesse™. During this time period, condoms may not be reliable for preventing pregnancy or for protecting against transmission of HIV and other sexually transmitted diseases (see WARNINGS ).
Drug Interactions
Clindamycin has been shown to have neuromuscular blocking properties that may enhance the action of other neuromuscular blocking agents. Therefore, it should be used with caution in patients receiving such agents.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term studies in animals have not been performed with clindamycin to evaluate carcinogenic potential. Genotoxicity tests performed included a rat micronucleus test and an Ames test. Both tests were negative. Fertility studies in rats treated orally with up to 300 mg/kg/day (31 times the human exposure based on mg/m 2 ) revealed no effects on fertility or mating ability.
Pregnancy: Teratogenic Effects
Pregnancy Category B
There are no adequate and well-controlled studies of Clindesse™ in pregnant women.
Clindesse™ should be used during pregnancy only if clearly needed.
Another intravaginal formulation containing 2% clindamycin phosphate has been studied in pregnant women during the second trimester. In women treated for seven days, abnormal labor was reported in 1.1% of patients who received that clindamycin vaginal cream formulation compared with 0.5% of patients who received placebo.
Reproduction studies have been performed in rats and mice using oral and parenteral doses of clindamycin up to 600 mg/kg/day (62 and 25 times, respectively, the maximum human exposure based on mg/m 2 ) and have revealed no evidence of harm to the fetus due to clindamycin. In one mouse strain, cleft palates were observed in treated fetuses; this outcome was not produced in other mouse strains or in other species and is, therefore, considered to be a strain specific effect.
Nursing Mothers
Clindamycin has been detected in human milk after oral or parenteral administration. It is not known if clindamycin is excreted in human milk following the use of vaginally administered clindamycin phosphate.
Because of the potential for serious adverse reactions in nursing infants from clindamycin phosphate, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
The safety and efficacy of Clindesse™ in the treatment of bacterial vaginosis in post-menarchal females have been established on the extrapolation of clinical trial data from adult women. The safety and efficacy of Clindesse™ in premenarchal females have not been established.
Geriatric Use
Clinical studies with Clindesse™ did not include suffficient numbers of subjects 65 years of age or older to determine whether they respond differently than younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients.
ADVERSE REACTIONS
Clinical Trials
In clinical trials totaling 368 women treated with a single dose of Clindesse™ , 1.6% of the patients discontinued therapy due to adverse events. Medical events judged to be definitely related, probably related, or possibly drugrelated were reported for 10.6% of the patients after receiving a single dose of Clindesse™ and in 17.6% of patients treated with placebo. Adverse events occurred in 126 of 368 patients (34.2%) treated with Clindesse™ and in 32 of 85 patients (37.6%) treated with placebo. Events occurring in >/=1% of patients receiving Clindesse™ in 3 clinical studies are shown in Table 1.
Table 1. All Adverse Events Reported in >/= 1% of Patients Receiving Clindesse™ in Clinical Studies Adverse EventsClindesse™
N=368
n (5)Placebo
N=85
n (%)Any adverse event126 (34.2) 32 (37.6) Vaginosis fungal NOS *52 (14.1) 7 (8.2) Vulvovaginal pruritus12 (3.3) 3 (3.5) Headache NOS *10 (2.7) 2 (2.4) Constipation4 (1.1) 0 (0) Nasopharyngitis4 (1.1) 0 (0) Back pain6 (1.6) 1 (1.2) Nausea5 (1.4) 3 (3.5) Urinary tract infection NOS *4 (1.1) 0 (0) Vaginal discharge4 (1.1) 2 (2.4) N=number of patients in intent-to-treat populationn (%)=number and percentage of patients with reported adverse eventNOS=not otherwise specifiedOther events not necessarily related to Clindesse™ but reported by < 1% of those women treated with Clindesse™:
Dermatologic: dermatitis, dry skin, pruritic rash
Gastrointestinal: diarrhea, dyspepsia, flatulence, hemorrhoids, vomiting
General: fatigue, pain, pyrexia, increased tendency to bruise, palpable lymph node
Immune System: hypersensitivity, food allergy
Infections: bladder infection, fungal infection, Herpes simplex, influenza, papilloma virus infection, sinusitis, tooth abscess, upper respiratory tract infection, vaginal infection, vulvovaginal trichomoniasis
Musculoskeletal: arthralgia, myalgia, neck pain, sciatica
Nervous System: dizziness, hypoeshesia
Psychiatric: anxiety disorder
Renal and Urinary Tract: bladder spasm
Reproductive System: pregnancy, cervical dysplasia, dysfunctional uterine bleeding, dysmenorrhea, intermenstrual bleeding, pelvic pain, uterine cervical disorder, uterine spasm, vaginal burning, vaginal irritation, atrophic vaginitis, vulvar erythema, vulvar laceration, vulvitis, vulvovaginal discomfort, vulvovaginal dryness, vulvovaginitis
Respiratory Tract: cough, epistaxis, pharyngitis, rhinorrhea, sinusitis, wheezing
Other Clindamycin Formulations
Clindesse™ Vaginal Cream affords minimal peak serum levels and systemic exposure (AUCs) of clindamycin compared to an oral or intravenous dose of clindamycin (see CLINICAL PHARMACOLOGY ). Although these lower levels of exposure are less likely to produce the common reactions seen with oral clindamycin, the possibility of these and other reactions cannot be excluded presently. Data from well-controlled trials directly comparing clindamycin administered orally to clindamycin administered vaginally are not available.
The following adverse reactions and altered laboratory tests have been reported with the oral or parenteral use of clindamycin:
Gastrointestinal: Abdominal pain, esophagitis, nausea, vomiting, diarrhea and pseudomembranous colitis (see WARNINGS ).
Hematopoietic: Transient neutropenia (leukopenia), eosinophilia, agranulocytosis, and thrombocytopenia have been reported. No direct etiologic relationship to concurrent clindamycin therapy could be made in any of these reports.
Hypersensitivity Reactions: Maculopapular rash, vesiculobullous rash, and urticaria have been observed during drug therapy. Generalized mild to moderate morbilliform-like skin rashes are the most frequently reported of all adverse reactions. Rare instances of erythema multiforme, some resembling Stevens-Johnson syndrome, have been associated with clindamycin. A few cases of anaphylactoid reactions have been reported.
Liver: Jaundice and abnormalities in liver function tests have been observed during clindamycin therapy.
Musculoskeletal: Rare instances of polyarthritis have been reported.
Renal: Although no direct relationship of clindamycin to renal damage has been established, renal dysfunction as evidenced by azotemia, oliguria, and/or proteinuria has been observed in rare instances.
OVERDOSAGE
Vaginally applied clindamycin phosphate vaginal cream 2% could be absorbed in sufficient amounts to produce systemic effects (see WARNINGS and ADVERSE REACTIONS ).
DOSAGE AND ADMINISTRATION
The recommended dose is a single applicatorful of Clindesse™ (approximately 5 g of vaginal cream containing approximately 100 mg of clindamycin phosphate) administered once intravaginally at any time of the day.
CLINICAL STUDIES
Two clinical studies were conducted to evaluate the efficacy of Clindesse™ for the treatment of bacterial vaginosis. In one clinical study involving 144 patients with a baseline Nugent score >/=4, Clindesse™ demonstrated superior efficacy over placebo intravaginal cream as measured by therapeutic cure, clinical cure, and Nugent score cure (Table 2). Therapeutic cure was a composite endpoint which required both clinical cure and Nugent score cure. Clinical cure required normal vaginal discharge, vaginal pH < 4.7,< 20% clue cells on wet mount preparation, and negative "whiff" test (detection of amine odor on addition of 10% KOH to sample of the vaginal discharge). A Nugent score of 0-3 was considered a Nugent score cure. The Nugent scoring is based on microscopic examination of the Gram's stained vaginal smears for quantification of specific bacterial morphotypes.
Table 2. Efficacy of Clindesse™ for Treatment of Bacterial Vaginosis in a Randomized, Double-Blind,
Placebo-Controlled, Parallel Group StudyOutcomeClindesse™
N =78
% CurePlacebo
N =66
% CureTreatment
Difference **/* (%) [97.5%
Confidence Interval]Therapeutic Cure **/**29.5 3.0 26.5 [14.0, 39.0] Clinical Cure41.0 19.7 21.3 [4.7, 38.0] Nugent Score Cure44.9 6.1 38.8 [24.6, 53.1] N=number of patients in treatment group (modified intent-to-treat population defined as all subjects randomized who received at least one dose of study medication, and who had a baseline Nugent score of at least 4)**/* Treatment difference=Clindesse™ minus placebo cure rates**/** Primary efficacy outcome measureIn a second controlled clinical study involving 432 patients with a baseline Nugent score of >/=4, 221 women self-administered a single dose of Clindesse™ , and 211 women self-administered a single daily dose of Cleocin® Vaginal Cream 2% for 7 days. A single dose of Clindesse™ was shown to be similar to 7 daily doses of Cleocin® Vaginal Cream 2% for treatment of bacterial vaginosis as measured by therapeutic cure, clinical cure or Nugent score cure (Table 3). The study endpoints were identical to those described above for the placebo-controlled study.
The cure rates reported in the clinical studies with Clindesse™ were based on resolution of 4 out of 4 Amsel criteria and a Nugent score of <4, while the criteria for cure in previous clinical studies with Cleocin® Vaginal Cream were based solely on resolution of 2 out of 4 Amsel criteria, resulting in higher reported rates of cure for bacterial vaginosis.
Table 3. Efficacy of Clindesse™ in Treatment of Bacterial Vaginosis in a Randomized, Investigator-Blind, Active-Controlled Comparative StudyOutcomeClindesse™
Single dose
N =221
% CureCleocin® Vaginal
Cream (7 doses)
N =211
% CureTreatment
Difference **/* (%)
[95% Confidence
Interval]Therapeutic Cure **/**33.0 37.0 -3.9 [-12.9,5.1] Clinical Cure53.4 54.0 -0.6 [-10.0, 8.8] Nugent Score Cure45.7 49.3 -3.6 [-13.1, 5.8]. **/* Treatment difference=Clindesse™ minus Cleocin® Vaginal Cream cure ratesN=number of patients in treatment group (modified intent-to-treat population defined as all subjects randomized who received at least one dose of study medication, and who had a baseline Nugent score of at least 4)**/** Primary efficacy outcome measureTable 4. Efficacy of Clindesse™ in Treatment of Bacterial Vaginosis in a Randomized, Investigator-Blind, Active-Controlled Comparative Study - Per ProtocolOutcomeClindessee™
Single dose
N =126
% CureCleocin® Vaginal
Cream (7 doses)
N =125
% Cur eTreatment
Difference **/* (%)
[95% Confidence
Interval]Therapeutic Cure **/**42.1 45.6 -3.5 [-15.5, 8.7] Clinical Cure64.3 63.2 1.1 [-10.8, 13.0] Nugent Score Cure56.5 § 57.7 § -1.3 [-13.6, 11.1] **/* Treatment difference=Clindesse™ minus Cleocin® Vaginal Cream cure ratesN=number of patients in treatment group (per protocol population defined as all subjects included in the modified intent-to-treat population who completed the study without significant protocol violation)**/** Primary efficacy outcome measure§ Four subject (2 from each treatment group) did not have complete Nugent scores and were not included in the Nugent Score cure analysis.HOW SUPPLIED
Clindesse™ (clindamycin phosphate) Vaginal Cream, 2%, is available in cartons containing one single-dose, pre-filled disposable applicator (NDC 64011-124-08). Each applicator delivers approximately 5 g of vaginal cream containing approximately 100 mg of clindamycin phosphate.
Store at controlled room temperature 25°C (77°F); excursions permitted to 15°-30°C (59°-86°F). [See USP Controlled Room Temperature.] Avoid heat above 30°C (86°F).
U.S. Patent No. 5,266,329; Other patents pending.
Marketed by Ther-Rx Corporation
St. Louis, MO 63044
Rev. 11/04 P4250
Subscribe to the "News" RSS Feed 
TOP ۞
