-
Humulin 70/30 Pen (Lilly)
INFORMATION FOR THE PATIENT
3 ML DISPOSABLE INSULIN DELIVERY DEVICEWARNINGS
THIS Lilly HUMAN INSULIN PRODUCT DIFFERS FROM ANIMAL-SOURCE INSULINS BECAUSE IT IS STRUCTURALLY IDENTICAL TO THE INSULIN PRODUCED BY YOUR BODY'S PANCREAS AND BECAUSE OF ITS UNIQUE MANUFACTURING PROCESS.
ANY CHANGE OF INSULIN SHOULD BE MADE CAUTIOUSLY AND ONLY UNDER MEDICAL SUPERVISION. CHANGES IN STRENGTH, MANUFACTURER, TYPE (E.G., REGULAR, NPH, LENTE, ETC), SPECIES (BEEF, PORK, BEEF-PORK, HUMAN), OR METHOD OF MANUFACTURE (rDNA VERSUS ANIMAL-SOURCE INSULIN) MAY RESULT IN THE NEED FOR A CHANGE IN DOSAGE.
SOME PATIENTS TAKING HUMULIN® (HUMAN INSULIN, rDNA ORIGIN) MAY REQUIRE A CHANGE IN DOSAGE FROM THAT USED WITH ANIMAL-SOURCE INSULINS. IF AN ADJUSTMENT IS NEEDED, IT MAY OCCUR WITH THE FIRST DOSE OR DURING THE FIRST SEVERAL WEEKS OR MONTHS.
TO OBTAIN AN ACCURATE DOSE, CAREFULLY READ AND FOLLOW THE "DISPOSABLE INSULIN DELIVERY DEVICE USER MANUAL" AND THIS "INFORMATION FOR THE PATIENT" INSERT BEFORE USING THIS PRODUCT.
BEFORE EACH INJECTION, YOU SHOULD PRIME THE PEN, A NECESSARY STEP TO MAKE SURE THE PEN IS READY TO DOSE. PRIMING THE PEN IS IMPORTANT TO CONFIRM THAT INSULIN COMES OUT WHEN YOU PUSH THE INJECTION BUTTON AND TO REMOVE AIR THAT MAY COLLECT IN THE INSULIN CARTRIDGE DURING NORMAL USE. IF YOU DO NOT PRIME, YOU MAY RECEIVE TOO MUCH OR TOO LITTLE INSULIN ( see also INSTRUCTIONS FOR INSULIN PEN USE section).
DIABETES
Insulin is a hormone produced by the pancreas, a large gland that lies near the stomach. This hormone is necessary for the body's correct use of food, especially sugar. Diabetes occurs when the pancreas does not make enough insulin to meet your body's needs.
To control your diabetes, your doctor has prescribed injections of insulin products to keep your blood glucose at a near-normal level. You have been instructed to test your blood and/or your urine regularly for glucose. Studies have shown that some chronic complications of diabetes such as eye disease, kidney disease, and nerve disease can be significantly reduced if the blood sugar is maintained as close to normal as possible. The American Diabetes Association recommends that if your pre-meal glucose levels are consistently above 130 mg/dL or your hemoglobin A 1c (HbA 1c ) is more than 7%, consult your doctor. A change in your diabetes therapy may be needed. If your blood tests consistently show below-normal glucose levels, you should also let your doctor know. Proper control of your diabetes requires close and constant cooperation with your doctor. Despite diabetes, you can lead an active and healthy life if you eat a balanced diet, exercise regularly, and take your insulin injections as prescribed.
Always keep an extra supply of insulin as well as a spare syringe and needle on hand. Always wear diabetic identification so that appropriate treatment can be given if complications occur away from home.
70/30 HUMAN INSULIN
Description
Humulin is synthesized in a non-disease-producing special laboratory strain of Escherichia coli bacteria that has been genetically altered by the addition of the human gene for insulin production. Humulin® 70/30 is a mixture of 70% Human Insulin Isophane Suspension and 30% Human Insulin Injection, (rDNA origin). It is an intermediate-acting insulin combined with the more rapid onset of action of regular insulin. The duration of activity may last up to 24 hours following injection. The time course of action of any insulin may vary considerably in different individuals or at different times in the same individual. As with all insulin preparations, the duration of action of Humulin 70/30 is dependent on dose, site of injection, blood supply, temperature, and physical activity. Humulin 70/30 is a sterile suspension and is for subcutaneous injection only. It should not be used intravenously or intramuscularly. The concentration of Humulin 70/30 in the Humulin 70/30 Pen is 100 units/mL (U-100).
Identification
Humulin disposable insulin delivery devices, by Eli Lilly and Company, are available in 2 formulations -- NPH and 70/30.
Your doctor has prescribed the type of insulin that he/she believes is best for you. DO NOT USE ANY OTHER INSULIN EXCEPT ON HIS/HER ADVICE AND DIRECTION.
The Humulin 70/30 Pen is available in boxes of 5 disposable insulin delivery devices ("insulin Pens"). The Humulin 70/30 Pen is not designed to allow any other insulin to be mixed in its cartridge, or for the cartridge to be removed.
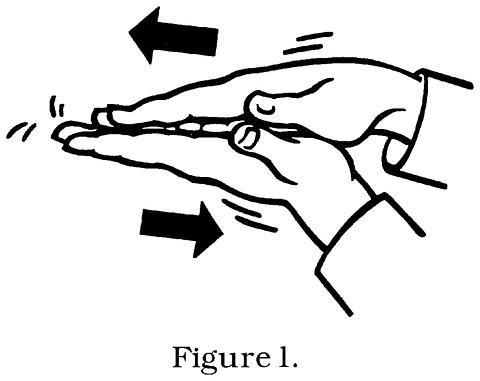
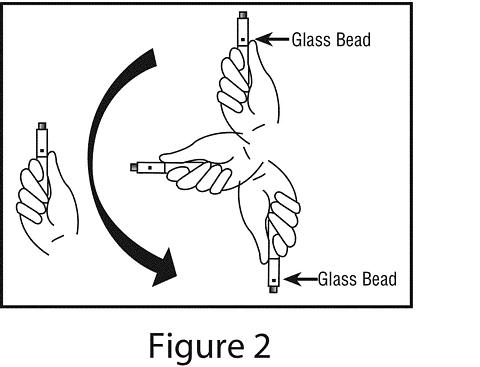
Always examine the appearance of Humulin 70/30 suspension in the insulin Pen before administering a dose. A cartridge of Humulin 70/30 contains a small glass bead to assist in mixing. Humulin 70/30 Pen must be rolled between the palms 10 times and inverted 180° 10 times before each injection so that the contents are uniformly mixed ( see Figures 1 and 2). Inspect the Humulin 70/30 suspension for uniform mixing and repeat the above steps as necessary.
Humulin 70/30 should look uniformly cloudy or milky after mixing. Do not use if the insulin substance (the white material) remains visibly separated from the liquid after mixing. Do not use the Humulin 70/30 Pen if there are clumps in the insulin after mixing. Do not use the Humulin 70/30 Pen if solid white particles stick to the walls of the cartridge, giving it a frosted appearance.
Always check the appearance of the Humulin 70/30 suspension in the insulin Pen before using, and if you note anything unusual in the appearance of Humulin 70/30 suspension or notice your insulin requirements changing markedly, consult your doctor.
Never attempt to remove the cartridge from the Humulin 70/30 Pen. Inspect the cartridge through the clear cartridge holder.
Storage
Not in-use (unopened): Humulin 70/30 Pens not in-use should be stored in a refrigerator but not in the freezer. Do not use a Humulin 70/30 Pen if it has been frozen.
In-use: Humulin 70/30 Pens in-use should NOT be refrigerated but should be kept at room temperature (below 86°F [30°C]) away from direct heat and light. Humulin 70/30 Pens in-use must be discarded after 10 days, even if they still contain Humulin 70/30.
Do not use Humulin 70/30 Pens after the expiration date stamped on the label.
INSTRUCTIONS FOR INSULIN PEN USE
It is important to read, understand, and follow the instructions in the "Disposable Insulin Delivery Device User Manual" before using. Failure to follow instructions may result in getting too much or too little insulin. The needle must be changed and the Pen must be primed before each injection to make sure the Pen is ready to dose. Performing these steps before each injection is important to confirm that insulin comes out when you push the injection button, and to remove air that may collect in the insulin cartridge during normal use.
Every time you inject:
- Use a new needle.
- Prime to make sure the Pen is ready to dose.
- Make sure you got your full dose.
NEVER SHARE INSULIN PENS, CARTRIDGES, OR NEEDLES.
PREPARING THE INSULIN PEN FOR INJECTION
- Always check the appearance of the Humulin 70/30 suspension in the insulin Pen before using.
- Roll the Humulin 70/30 Pen between the palms 10 times ( see Figure 1).
- Holding the Humulin 70/30 Pen by one end, invert it 180° slowly 10 times to allow the small glass bead to travel the full length of the cartridge with each inversion ( see Figure 2). The cartridge is contained in the clear cartridge holder of the Humulin 70/30 Pen.
- Inspect the appearance of the Humulin 70/30 suspension to make sure the contents look uniformly cloudy or milky. If not, repeat the above steps until the contents are mixed. Do not use a Humulin 70/30 Pen if there are clumps in the insulin or if solid white particles stick to the walls of the cartridge.
- Follow the instructions in the "Disposable Insulin Delivery Device User Manual" for these steps:
- Preparing the Pen
- Attaching the Needle. Use a new needle for each injection.
- Priming the Pen. The Pen must be primed before each injection to make sure the Pen is ready to dose. Performing the priming step is important to confirm that insulin comes out when you push the injection button, and to remove air that may collect in the insulin cartridge during normal use.
- Setting a Dose
- Injecting a Dose. To make sure you have received your full dose, you must push the injection button all the way down until you see a diamond or an arrow (->) in the center of the dose window.
- Following an Injection
PREPARING FOR INJECTION
- Wash your hands.
- To avoid tissue damage, choose a site for each injection that is at least 1/2 inch from the previous injection site. The usual sites of injection are abdomen, thighs, and arms.
- Cleanse the skin with alcohol where the injection is to be made.
- With one hand, stabilize the skin by spreading it or pinching up a large area.
- Inject the dose as instructed by your doctor. Hold the needle under the skin for at least 5 seconds after injecting.
- After injecting a dose, pull the needle out and apply gentle pressure over the injection site for several seconds. Do not rub the area.
- Immediately after an injection, remove the needle from the Humulin 70/30 Pen. Doing so will guard against contamination, leakage, reentry of air, and needle clogs. Do not reuse needles. Place the used needle in a puncture-resistant disposable container and properly dispose of it as directed by your Health Care Professional.
DOSAGE
Your doctor has told you which insulin to use, how much, and when and how often to inject it. Because each patient's case of diabetes is different, this schedule has been individualized for you.
Your usual Humulin 70/30 dose may be affected by changes in your food, activity, or work schedule. Carefully follow your doctor's instructions to allow for these changes. Other things that may affect your Humulin 70/30 dose are:
Illness
Illness, especially with nausea and vomiting, may cause your insulin requirements to change. Even if you are not eating, you will still require insulin. You and your doctor should establish a sick day plan for you to use in case of illness. When you are sick, test your blood glucose/urine glucose and ketones frequently and call your doctor as instructed.
Pregnancy
Good control of diabetes is especially important for you and your unborn baby. Pregnancy may make managing your diabetes more difficult. If you are planning to have a baby, are pregnant, or are nursing a baby, consult your doctor.
Medication
Insulin requirements may be increased if you are taking other drugs with hyperglycemic activity, such as oral contraceptives, corticosteroids, or thyroid replacement therapy. Insulin requirements may be reduced in the presence of drugs with blood-glucose-lowering activity, such as oral antidiabetic agents, salicylates (for example, aspirin), sulfa antibiotics, alcohol, and certain antidepressants. Always discuss any medications you are taking with your doctor.
Exercise
Exercise may lower your body's need for insulin during and for some time after the physical activity. Exercise may also speed up the effect of a Humulin 70/30 dose, especially if the exercise involves the area of injection site (for example, the leg should not be used for injection just prior to running). Discuss with your doctor how you should adjust your regimen to accommodate exercise.
Travel
Persons traveling across more than 2 time zones should consult their doctor concerning adjustments in their insulin schedule.
COMMON PROBLEMS OF DIABETES
Hypoglycemia (Low Blood Sugar)
Hypoglycemia (too little glucose in the blood) is one of the most frequent adverse events experienced by insulin users. It can be brought about by:
- Taking too much insulin.
- Missing or delaying meals.
- Exercising or working more than usual.
- An infection or illness (especially with diarrhea or vomiting).
- A change in the body's need for insulin.
- Diseases of the adrenal, pituitary or thyroid gland, or progression of kidney or liver disease.
- Interactions with other drugs that lower blood glucose, such as oral antidiabetic agents, salicylates (for example, aspirin), sulfa antibiotics, and certain antidepressants.
- Consumption of alcoholic beverages.
Symptoms of mild to moderate hypoglycemia may occur suddenly and can include:
- sweating
- dizziness
- palpitation
- tremor
- hunger
- restlessness
- tingling in the hands, feet, lips, or tongue
- lightheadedness
- inability to concentrate
- headache
- drowsiness
- sleep disturbances
- anxiety
- blurred vision
- slurred speech
- depressed mood
- irritability
- abnormal behavior
- unsteady movement
- personality changes
Signs of severe hypoglycemia can include:
- disorientation
- unconsciousness
- seizures
- death
Therefore, it is important that assistance be obtained immediately.
Early warning symptoms of hypoglycemia may be different or less pronounced under certain conditions, such as long duration of diabetes, diabetic nerve disease, medications such as beta-blockers, change in insulin preparations, or intensified control (3 or more insulin injections per day) of diabetes.
A few patients who have experienced hypoglycemic reactions after transfer from animal-source insulin to human insulin have reported that the early warning symptoms of hypoglycemia were less pronounced or different from those experienced with their previous insulin.
Without recognition of early warning symptoms, you may not be able to take steps to avoid more serious hypoglycemia. Be alert for all of the various types of symptoms that may indicate hypoglycemia. Patients who experience hypoglycemia without early warning symptoms should monitor their blood glucose frequently, especially prior to activities such as driving. If the blood glucose is below your normal fasting glucose, you should consider eating or drinking sugar-containing foods to treat your hypoglycemia.
Mild to moderate hypoglycemia may be treated by eating foods or drinks that contain sugar. Patients should always carry a quick source of sugar, such as candy mints or glucose tablets. More severe hypoglycemia may require the assistance of another person. Patients who are unable to take sugar orally or who are unconscious require an injection of glucagon or should be treated with intravenous administration of glucose at a medical facility.
You should learn to recognize your own symptoms of hypoglycemia. If you are uncertain about these symptoms, you should monitor your blood glucose frequently to help you learn to recognize the symptoms that you experience with hypoglycemia.
If you have frequent episodes of hypoglycemia or experience difficulty in recognizing the symptoms, you should con-sult your doctor to discuss possible changes in therapy, meal plans, and/or exercise programs to help you avoid hypoglycemia.
Hyperglycemia and Diabetic Ketoacidosis (DKA)
Hyperglycemia (too much glucose in the blood) may develop if your body has too little insulin. Hyperglycemia can be brought about by:
- Omitting your insulin or taking less than the doctor has prescribed.
- Eating significantly more than your meal plan suggests.
- Developing a fever, infection, or other significant stressful situation.
In patients with type 1 or insulin-dependent diabetes, prolonged hyperglycemia can result in DKA. The first symptoms of DKA usually come on gradually, over a period of hours or days, and include a drowsy feeling, flushed face, thirst, loss of appetite, and fruity odor on the breath. With DKA, urine tests show large amounts of glucose and ketones. Heavy breathing and a rapid pulse are more severe symptoms. If uncorrected, prolonged hyperglycemia or DKA can lead to nausea, vomiting, stomach pains, dehydration, loss of consciousness or death. Therefore, it is important that you obtain medical assistance immediately.
Lipodystrophy
Rarely, administration of insulin subcutaneously can result in lipoatrophy (depression in the skin) or lipohypertrophy (enlargement or thickening of tissue). If you notice either of these conditions, consult your doctor. A change in your injection technique may help alleviate the problem.
Allergy to Insulin
Local Allergy --Patients occasionally experience redness, swelling, and itching at the site of injection of insulin. This condition, called local allergy, usually clears up in a few days to a few weeks. In some instances, this condition may be related to factors other than insulin, such as irritants in the skin cleansing agent or poor injection technique. If you have local reactions, contact your doctor.
Systemic Allergy --Less common, but potentially more serious, is generalized allergy to insulin, which may cause rash over the whole body, shortness of breath, wheezing, reduction in blood pressure, fast pulse, or sweating. Severe cases of generalized allergy may be life threatening. If you think you are having a generalized allergic reaction to insulin, notify a doctor immediately.
ADDITIONAL INFORMATION
Additional information about diabetes may be obtained from your diabetes educator.
DIABETES FORECAST is a magazine designed especially for people with diabetes and their families. It is available by subscription from the American Diabetes Association (ADA), P.O. Box 363, Mt. Morris, IL 61054-0363, 1-800-DIABETES (1-800-342-2383).
Another publication, COUNTDOWN, is available from the Juvenile Diabetes Research Foundation International (JDRFI), 120 Wall Street 19th Floor, New York, NY 10005, 1-800-533-CURE (1-800-533-2873).
Additional information about Humulin and Humulin 70/30 Pens can be obtained by calling The Lilly Answers Center at 1-800-LillyRx (1-800-545-5979).
Literature revised April 22, 2004
Manufactured by Lilly France S.A.S.
F-67640 Fegersheim, France
for Eli Lilly and Company
Indianapolis, IN 46285, USA
Copyright © 1998, 2004, Eli Lilly and Company. All rights reserved.
PA 9145 FSAMP
Subscribe to the "News" RSS Feed 
TOP ۞
