-
Iveegam EN (Baxter Healthcare)
DESCRIPTION
IVEEGAM EN, Immune Globulin Intravenous (Human) [IGIV], is a sterile freeze-dried concentrate of immunoglobulin G (IgG). Reconstitution of the freeze-dried powder with the accompanying quantity of Sterile Water for Injection, U.S.P. gives a 5% protein solution suitable for intravenous administration. This final solution contains, per mL, 50±5 mg of IgG, 50 mg of glucose as a stabilizer, and 3 mg of sodium chloride. Trace amounts of IgM and IgA are also present. The reconstituted solution is clear, colorless, and free of detectable aggregates. It contains no preservative.
IVEEGAM EN is prepared from large pools of human plasma. The pooled plasma is fractionated by a modified cold ethanol process. Cohn Fraction II is subjected to treatment with immobilized trypsin and purified by sequential precipitation steps with polyethylene glycol (PEG). Poly-thylene glycol may be present in the final product at levels below 0.5 g/dL. The IVEEGAM EN manufacturing process provides a significant viral reduction in in vitro studies. These studies, summarized in Table 1, demonstrate virus clearance during IVEEGAM EN manufacturing using infectious Human Immunodeficiency virus, Type 1 (HIV-1); Tick-Borne Encephalitis virus (TBEV), a model virus for Hepatitis C virus; Pseudorabies virus (PRV), a model virus for lipid-enveloped DNA viruses; Equine Rhinovirus, Type 1 (ERV-1), a model virus for non-lipid enveloped RNA viruses; Mouse Murine virus (MMV), a model virus for B19 Parvovirus; and infectious Hepatitis A virus (HAV). These reductions are achieved through a combination of precipitation of Cohn Fraction II + III, 12% alcohol precipitation, DEAE-Sephadex adsorption, incubation with immobilized hydrolases and PEG precipitation.
[See table below]Table 1
In Vitro Virus Clearance During IVEEGAM EN
ManufacturingManufacturing
StepVirus Clearance, log 10 HIV-1TBEV 1 PRV 2 ERV-1 3 MMV 4 HAV Precipitation of Cohn Fraction II + III2.2 1.6 1.2 4.2 ND ND 12% Alcohol> 4.9 > 4.8 4.7 > 5.0 ND ND DEAE Sephadex> 4.3 5.0 1.5 > 5.1 >6.6 >5.4 Hydrolase Incubation4.1 4.8 > 5.4 5.6 <1.0 ND PEG Precipitation4.1 > 4.4 > 6.1 4.6 ND ND Cumulative Reduction>19.6 >20.6 >18.9 >24.5 >6.6 >5.4 ND = Not Done; 1 Model virus for Hepatitis C virus (HCV); 2 Model virus for lipid enveloped DNA viruses; 3 Model virus for non-lipid enveloped RNA viruses; 4 Model virus for B19 Parvovirus
CLINICAL PHARMACOLOGY
Patients with primary humoral immunodeficiency are at high risk for the development of acute and chronic bacterial infections because of their low levels of circulating IgG (1,2). IVEEGAM EN, Immune Globulin Intravenous (Human) provides a broad spectrum of IgG antibodies (3). The opsonizing, neutralizing, and complement binding activities of these antibodies help prevent or attenuate a multiplicity of infectious diseases.
When administered intravenously, 100% of the IgG antibodies are available in the circulation immediately. The distribution of the intravenously administered preparation between intra- and extravascular compartments requires several days to reach an equilibrium. The serum IgG level therefore drops to approximately 40-50% of the peak level during the first week postinfusion (4, 5).
IVEEGAM EN has a half-life of approximately three to four weeks, which is in agreement with that reported for intramuscular immunoglobulin (4, 6). In six agammaglobulinemic patients, the half-life of IVEEGAM was determined by measuring the activity of tetanus antibody during a four week period after infusion of 150 mg/kg body mass. The half-life ranged from 23 to 29 days (6). Variation in half-life has been observed among patients and is important in determining the dosage regimen for each patient.
IgG serum levels were measured in 21 patients with primary immunodeficiencies treated with IVEEGAM with an average monthly dose of 225 mg/kg body mass for approximately 16 months. Serum levels increased from an average preinfusion level of 406 mg IgG/dL to an average of 762 mg IgG/dL postinfusion. The average increase in individual patients' serum IgG levels calculated per 100 mg IgG/kg body mass varied from 44 to 309 mg/dL.
Infections were evaluated in 12 primary immunodeficient children receiving one of two dose levels of IVEEGAM: 150 mg/kg (low dose) or 500 mg/kg (high dose). Eight children had been previously treated with fresh plasma for up to two years. The number of days with infections was reduced when comparing low dose IVEEGAM to plasma and when comparing high dose to low dose IVEEGAM. The geometric means and ranges (mg/dL) of serum IgG levels for eight patients were: plasma: 169 (62-435), low dose IVEEGAM: 212 (68-425), and high dose IVEEGAM: 557 (315-810) (7).
Studies were performed to monitor for the presence of antibody to Human Immunodeficiency Virus (HIV) and markers for viral hepatitis. No evidence of viral transmission has been observed in more than 30 patients on various dosage regimens followed for periods of 4 to 12 months and tested at intervals ranging from 3 to 6 weeks.
In order to evaluate the efficacy and safety of IVEEGAM in the treatment of Kawasaki syndrome (KS), two controlled, multi-center, randomized studies were performed. The first study compared the efficacy and safety of IVEEGAM plus aspirin with that of aspirin alone in reducing the frequency of coronary artery abnormalities in children with acute KS (8). Children randomly assigned to the immune globulin group received IVEEGAM, 400 mg/kg body mass per day, for four consecutive days. Both treatment groups received aspirin, 100 mg/kg body mass each day through the fourteenth day of illness, and 3 to 5 mg/kg each day thereafter for approximately five weeks. Two weeks after enrollment, coronary artery abnormalities were present in 18 (23%) of 78 children in the aspirin only group as compared to 6 (8%) of 75 in the IVEEGAM group (p<0.01). Seven weeks after enrollment, abnormalities were present in 14 (18%) of 79 patients in the aspirin only group and 3 (4%) of 79 in the IVEEGAM group (p<0.005). It was concluded that high-dose IVEEGAM is safe and effective in reducing the prevalence of coronary artery abnormalities when administered early in the course of KS.
The second clinical trial was a multi-center, randomized trial involving 549 children with acute KS (9). Children were randomly assigned to receive IVEEGAM either in a single infusion of 2 g/kg over 10 hours or in daily infusions of 400 mg/kg for four consecutive days. Both treatment groups received aspirin, 100 mg/kg each day through the fourteenth day of illness, then 3 to 5 mg/kg each day thereafter. Results showed that at two weeks after enrollment coronary artery abnormalities were present in 24 (9.1%) of 263 children in the four-day group as compared to 12 (4.6%) of 260 in the single-infusion group (p<0.05). Seven weeks after enrollment abnormalities were present in 7.2% of the four-day group and in 3.9% of the single-infusion group (p<0.1). The two groups had a similar incidence of adverse effects, occurring in approximately 3% of children overall.
The second study thus supports the efficacy of IVEEGAM EN in treating acute KS, and further demonstrates that a single dose of 2 g/kg of IVEEGAM EN infused over 10 hours is at least as effective as four conservative daily doses of 400 mg/kg.
INDICATIONS AND USAGE
Immunodeficiency Syndromes
IVEEGAM EN, Immune Globulin Intravenous (Human) is indicated for replacement therapy in patients with primary immunodeficiency syndromes such as congenital agammaglobulinemia, common variable immunodeficiency, x-linked agammaglobulinemia (with or without hyper IgM) and Wiskott-Aldrich syndrome (2).
Patients with severe combined immunodeficiency have, in addition to a T-cell defect, an impairment of antibody production. They may benefit from replacement therapy with IVEEGAM EN even though this therapy will not correct the cellular immune defect.
IVEEGAM EN is especially useful when high levels or rapid elevation of circulating antibodies are desired or when intramuscular injections are contraindicated.
Kawasaki Syndrome
IVEEGAM EN is indicated in the treatment of Kawasaki syndrome. When administered in conjunction with aspirin, within ten days of onset of disease, treatment with either a single dose of 2000 mg IVEEGAM/kg body mass given over a ten hour period, or 400 mg IVEEGAM/kg body mass on four consecutive days resulted in a 65% to 78% decrease in the incidence of coronary artery abnormalities compared to treatment with aspirin alone (8, 9).
CONTRAINDICATIONS
IVEEGAM EN is contraindicated in individuals who are known to have had an anaphylactic or severe systemic response to Immune Globulin (Human).
Individuals with selective IgA deficiency should not receive IVEEGAM EN since these patients may experience severe reactions to the IgA which may be present.
WARNINGS
Warning
Immune Globulin Intravenous (Human) products have been reported to be associated with renal dysfunction, acute renal failure, osmotic nephrosis, and death (10). Patients predisposed to acute renal failure include patients with any degree of pre-existing renal insufficiency, diabetes mellitus, age greater than 65, volume depletion, sepsis, paraproteinemia, or patients receiving known nephrotoxic drugs. Especially in such patients, IGIV products should be administered at the minimum concentration available and the minimum rate of infusion practicable. While these reports of renal dysfunction and acute renal failure have been associated with the use of many of the licensed IGIV products, those containing sucrose as a stabilizer accounted for a disproportionate share of the total number. *
See PRECAUTIONS and DOSAGE AND ADMINISTRATION sections for important information intended to reduce the risk of acute renal failure.
* IVEEGAM EN does not contain sucrose
IVEEGAM EN should be administered only intravenously as the intramuscular and subcutaneous routes have not been evaluated.
Although not observed in the clinical studies with this product, severe anaphylactic reactions have been observed following administration of other immunoglobulin preparations (11-14). These reactions have been attributed to the presence of immunoglobulin A in certain preparations, and in certain instances, to antigen-antibody interactions, if patients had antigenemia and the respective antibodies were present in the product (12).
IF ANAPHYLACTIC OR SEVERE ANAPHYLACTOID REACTIONS OCCUR, THE INFUSION IS TO BE DISCONTINUED IMMEDIATELY. Whenever IVEEGAM EN is administered, appropriate therapy should be available to treat a severe anaphylactic reaction, e.g. epinephrine.
IVEEGAM EN is made from human plasma. Products made from human plasma may contain infectious agents, such as viruses, that can cause disease. The risk that such products will transmit an infectious agent has been reduced by screening plasma donors for prior exposure to certain viruses, by testing for the presence of certain current virus infections, and by inactivating and/or removing certain viruses (see DESCRIPTION ). Despite these measures, such products can still potentially transmit disease. Because this product is made from human blood, it may carry a risk of transmitting infectious agents, e.g., viruses and theoretically, the Creutzfeldt-Jakob disease (CJD) agent. ALL infections thought by a physician possibly to have been transmitted by this product should be reported by the physician or other healthcare provider to Baxter Healthcare Corporation, at 1-800-423-2862 (in the U.S.). The physician should discuss the risks and benefits of this product with the patient.
PRECAUTIONS
General
Assure that patients are not volume depleted prior to the initiation of the infusion of IGIV.
Periodic monitoring of renal function tests and urine output is particularly important in patients judged to have a potential increased risk for developing acute renal failure. Renal function, including measurement of blood urea nitrogen (BUN)/serum creatinine, should be assessed prior to the initial infusion of IVEEGAM EN and again at appropriate intervals thereafter. If renal function deteriorates, discontinuation of the product should be considered.
For patients judged to be at risk for developing renal dysfunction, it may be prudent to reduce the amount of product infused per unit time by infusing IVEEGAM EN at a rate less than 1.5 mg Ig per kg body weight per minute (0.03 mL/kg/minute).
Any vial which has been reconstituted should be used promptly.
Partially used vials should be discarded. Patients with severe antibody deficiency syndromes are more likely to react adversely to the initial infusions of homologous IGIV. Modified dosage regimens have been used to prevent such reactions. See DOSAGE AND ADMINISTRATION Section.
In isolated cases and mostly with the use of high doses, administration of IGIV from different manufacturers has been associated with the development of aseptic meningitis manifesting as neck rigidity with severe headache, nausea, vomiting, fever, drowsiness, photophobia, pain when moving the eyes, and dizziness (10). These symptoms can begin within hours or a few days after the infusion. These symptoms were reversible with or without therapy, and disappeared completely within a few hours or days.
Hemolysis
Immune Globulin Intravenous (Human) [IGIV] products can contain blood group antibodies which may act as hemolysins and induce in vivo coating of red blood cells with immunoglobulin, causing a positive direct antiglobulin reaction and, rarely, hemolysis (15-18) Hemolytic anemia can develop subsequent to IGIV therapy due to enhanced RBC sequestration (18) (See ADVERSE REACTIONS ). IGIV recipients should be monitored for clinical signs and symptoms of hemolysis (See PRECAUTIONS : LABORATORY TESTS ).
Transfusion-Related Acute Lung Injury (TRALI)
There have been reports of noncardiogenic pulmonary edema (Transfusion Related Acute Lung Injury [TRALI]) in patients administered IGIV (19). TRALI is characterized by severe respiratory distress, pulmonary edema, hypoxemia, normal left ventricular function, and fever and typically occurs within 1-6 hours after transfusion. Patients with TRALI may be managed using oxygen therapy with adequate ventilatory support.
IGIV recipients should be monitored for pulmonary adverse reactions. If TRALI is suspected, appropriate tests should be performed for the presence of anti-neutrophil antibodies in both the product and patient serum (See PRECAUTIONS : LABORATORY TESTS ).
Thrombotic Events
Thrombotic events have been reported in association with IGIV (20-22) (See ADVERSE REACTIONS Section). Patients at risk may include those with a history of atherosclerosis, multiple cardiovascular risk factors, advanced age, impaired cardiac output, and/or known or suspected hyperviscosity, hypercoaguable disorders and prolonged periods of immobilization. The potential risks and benefits of IGIV should be weighed against those of alternative therapies for all patients for whom IGIV administration is being considered. Baseline assessment of blood viscosity should be considered in patients at risk for hyperviscosity, including those with cryoglobulins, fasting chylomicronemia/markedly high triacylgycerols (triglycerides), or monoclonal gammopathies (See PRECAUTIONS : LABORATORY TESTS ).
Laboratory Tests
If signs and/or symptoms of hemolysis are present after IGIV infusion, appropriate confirmatory laboratory testing should be done (see PRECAUTIONS ).
If TRALI is suspected, appropriate tests should be performed for the presence of antineutrophil antibodies in both the product and patient serum (see PRECAUTIONS ).
Because of the potentially increased risk of thrombosis, baseline assessment of blood viscosity should be considered in patients at risk for hyperviscosity, including those with cryoglobulins, fasting chylomicronemia/markedly high triacylglycerols (triglycerides), or monoclonal gammopathies (see PRECAUTIONS ).
Information For Patient
Patients should be instructed to immediately report symptoms of decreased urine output, sudden weight gain, fluid retention/edema, and/or shortness of breath (which may suggest kidney damage) to their physicians.
Some viruses, such as parvovirus B19, are particularly difficult to remove or inactivate at this time. Parvovirus B19 most seriously affects pregnant women, or immune compromised individuals.
Symptoms of parvovirus B19 infection include fever, drowsiness, chills and runny nose followed about two weeks later by a rash, and joint pain. Patients should be encouraged to consult their physician if such symptoms appear.
Drug Interactions
For compatibility issues see DOSAGE AND ADMINISTRATION Section.
It is reported that antibodies in immune globulin preparations may interfere with the responses by patients to live viral vaccines such as measles, mumps, and rubella. Immunizing physicians should be informed of recent therapy with Immune Globulin Intravenous (Human), so that appropriate precautions may be taken.
Pregnancy Category C
Animal reproduction studies have not been carried out with IVEEGAM EN, Immune Globulin Intravenous (Human). It is also not known whether IVEEGAM EN can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. IVEEGAM EN should be given to a pregnant woman only if clearly needed.
ADVERSE REACTIONS
Increases in creatinine and blood urea nitrogen (BUN) have been observed as soon as one to two days following infusion. Progression to oliguria and anuria requiring dialysis has been observed, although some patients have improved spontaneously following cessation of treatment (23).
Types of severe renal adverse reactions that have been seen following IGIV therapy include:
- acute renal failure
- acute tubular necrosis (24)
- proximal tubular nephropathy
- osmotic nephrosis (10; see also 25-27)
Reported reactions to IVEEGAM in patients with primary humoral immunodeficiency have been mild and transient in nature, and have included flushing, increased blood pressure, malaise, headache, nausea, vomiting, low-grade fever, and rash. In clinical trials involving more than 1300 infusions, adverse reaction rates have ranged from 0.3% to 0.8% (4-7, 28). Although not observed in clinical trials with IVEEGAM, severe anaphylactic reactions have been reported with other immunoglobulin preparations.
In the first clinical trial of IVEEGAM in the treatment of Kawasaki syndrome, mild congestive heart failure developed with comparable frequency in the aspirin only group (5%) and in the aspirin plus IVEEGAM group (4%). In each of the latter cases, the child tolerated subsequent infusions without difficulty. After the first infusion, one child had shaking chills and itching, which resolved after treatment with diphenhydramine. These symptoms did not recur with subsequent infusions. One child had sepsis secondary to an intravenous line. One child treated with IVEEGAM had neutropenia and splenomegaly for several months after treatment; one child in the aspirin group also had neutropenia.
In the second Kawasaki syndrome clinical trial, 3.3% of children overall had possible complications attributable to IVEEGAM. Two children (0.36%) had hypotension, two (0.36%) had pruritus, nine (1.6%) had mild worsening of congestive heart failure, and five (0.91%) had other events, including infiltrates at the site of the i.v. line and skin slough (1), generalized edema without congestive heart failure (2), acute onset of nasal congestion and cough without urticaria, pruritus, or hypotension, responding to Benadryl Diphenhydramine HCl without interruption of infusion (1), and probable autoimmune hemolytic anemia (1). There were no life-threatening complications in either study.
No long-term hematological or biochemical changes attributable to IVEEGAM therapy were detected during the course of either study. No evidence for the transmission of non-A/non-B hepatitis or human immunodeficiency virus was associated with the use of IVEEGAM.
Postmarketing:
The following list of adverse reaction have been identified and reported during the post-approval use of IGIV products:
Respiratory cyanosis, hypoxemia, pulmo-
nary edema, dyspnea, broncho-
spasmCardiovascular thromboembolism, hypotension Neurological seizures, tremor Hematologic hemolysis, positive direct anti-
globulin (Coombs) testGeneral/Body as a Whole pyrexia, rigors Musculoskeletal back pain Gastrointestinal hepatic dysfunction, abdominal pain Rare and Uncommon Adverse Events:
Respiratory apnea, Acute Respiratory Distress Syndrome (ARDS),Transfusion Associated Lung Injury (TRALI) Integumentary bullous dermatitis, epidermolysis, erythema multiforme, Stevens-Johnson syndrome Cardiovascular cardiac arrest, vascular collapse Neurological coma, loss of consciousness Hematologic pancytopenia, leukopenia
Because postmarketing reporting of these reactions is voluntary and the at-risk populations are of uncertain size, it is not always possible to reliably estimate the frequency of the reaction or establish a causal relationship to exposure to the product. Such is also the case with literature reports authored independently (29). See PRECAUTIONS Section.DOSAGE AND ADMINISTRATION
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration whenever solution and container permit. Reconstituted vials found to contain particles or to be discolored should not be used.
Reconstitute IVEEGAM EN, Immune Globulin Intravenous (Human) with Sterile Water for Injection, U.S.P. only. The reconstituted product may be diluted with 5% dextrose or saline.
Interactions or incompatibilities with other drugs have not been evaluated.
Do not mix IVEEGAM EN with other brands of intravenous immunoglobulins in preparing a large dose.
If administered with other preparations, always use separate infusion lines. When using primary infusion lines, rinse with saline prior to the infusion of IVEEGAM EN.
IVEEGAM EN, Immune Globulin Intravenous (Human) must be administered intravenously after reconstitution. The usual rate of administration is 1 mL per minute up to a maximum of 2 mL per minute for the 5% solution.
For patients judged to be at risk for developing renal dysfunction, it may be prudent to reduce the amount of product infused per unit time by infusing IVEEGAM EN at a rate less than 1.5 mg Ig per kg body weight per minute (0.03 mL/kg/minute).
No prospective data are presently available to identify a maximum safe dose, concentration, and rate of infusion in patients determined to be at increased risk of acute renal failure. In the absence of prospective data, the recommended doses should not be exceeded and the concentration and infusion rate selected should be the minimum level practicable. Reduction in dose, concentration, and/or rate of administration in patients at risk of acute renal failure has been proposed in the literature in order to reduce the risk of acute renal failure (30).
Immunodeficiency Syndromes
A dose of 200 mg/kg per month is recommended for treatment of primary humoral immunodeficiency syndromes.
If the desired clinical results are not obtained, the dose may be increased up to 4-fold or intervals between infusions shortened. Doses of IVEEGAM EN, Immune Globulin Intravenous (Human) up to 800 mg/kg body mass per month were tolerated by immunodeficient patients (6).
If adequate doses are given at regular intervals, pre-infusion IgG levels may be expected to rise steadily over a period of 6-12 months until a plateau is reached. The minimum serum concentration of IgG necessary for protection has not been established.
Dose regimens have been modified in an attempt to pre-vent adverse reactions in previously untreated, severe, immunodeficient patients. In a limited number of such patients, treatment has been initiated with lower doses of IVEEGAM EN diluted with saline or 5% dextrose. With gradually increasing dose levels and protein concentrations (up to 5% protein) adverse reactions were not observed (6).
Kawasaki Syndrome
Treatment with IVEEGAM EN should be initiated within ten days of onset of the disease. Either a dosage of 400 mg/kg body mass daily for four consecutive days or a single dose of 2000 mg/kg given over a ten hour period may be used. Because all studies of this product, to date, have involved concurrent administration of aspirin, the treatment regimen should include aspirin, 100 mg/kg each day through the fourteenth day of illness, then 3 to 5 mg/kg each day thereafter for a period of five weeks.
Reconstitution
Reconstitution with Sterile Water for Injection, U.S.P (diluent) provided in each package results in a 5% solution.
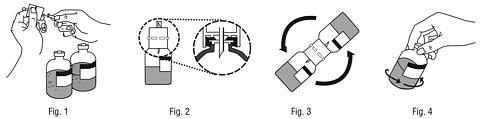
- Remove protective caps from the concentrate and diluent bottles and disinfect rubber stoppers of both bottles.
- Remove protective covering from one end of the accompanying transfer device (Fig. 1) and insert the exposed spike end perpendicularly through the center of the diluent bottle stopper. Press down firmly so that the transfer device fits snugly against the diluent bottle (Fig. 2). Caution: Failure to use center of stopper may result in dislodging the stopper.
- Remove protective cap from the other end of the transfer device. Do not touch the exposed spike end.
-
Hold concentrate bottle firmly and at an angle of approximately 45 degrees. Invert the diluent bottle with the transfer device at an angle complementary to the concentrate bottle (approximately 45 degrees) and firmly insert the transfer device into the concentrate bottle through the center of the rubber stopper (Fig. 3). Diluent will be drawn into the concentrate bottle by vaccum.
Note: Invert the diluent bottle with attached transfer device rapidly into the concentrate bottle in order to avoid loss of diluent.
Caution: Failure to use center of stopper may result in dislodging the stopper and loss of vacuum. - Disconnect the two bottles, leaving the transfer device on the diluent bottle. Accelerate reconstitution by agitating or rotating the concentrate bottle (Fig. 4). Do Not Shake Vigorously.
- Either draw up the clear solution into a syringe using the accompanying filter needle (500 mg and 1000 mg sizes) or administer the solution directly using the accompanying infusion set with filter (2500 mg and 5000 mg sizes).
HOW SUPPLIED
IVEEGAM EN, Immune Globulin Intravenous (Human) 500 mg:
1 vial containing 500 mg of freeze-dried IVEEGAM EN, Immune Globulin Intravenous (Human),
1 vial containing 10 mL of Sterile Water for Injection, U.S.P.
(This Product Contains Dry Natural Rubber.),
1 transfer device,
1 filter needle.
IVEEGAM EN, Immune Globulin Intravenous (Human) 1000 mg:
1 vial containing 1000 mg of freeze-dried IVEEGAM EN, Immune Globulin Intravenous (Human),
1 vial containing 20 mL of Sterile Water for Injection, U.S.P.
(This Product Contains Dry Natural Rubber.),
1 transfer device,
1 filter needle.
IVEEGAM EN, Immune Globulin Intravenous (Human) 2500 mg:
1 infusion bottle containing 2500 mg of freeze-dried IVEEGAM EN, Immune Globulin Intravenous (Human),
1 vial containing 50 mL of Sterile Water for Injection, U.S.P.
(This Product Contains Dry Natural Rubber.),
1 transfer device,
1 infusion set with filter.
IVEEGAM EN, Immune Globulin Intravenous (Human) 5000 mg:
1 infusion bottle containing 5000 mg of freeze-dried IVEEGAM EN, Immune Globulin Intravenous (Human),
1 vial containing 100 mL of Sterile Water for Injection, U.S.P.
(This Product Contains Dry Natural Rubber.),
1 transfer device,
1 infusion set with filter.
Rx only
STORAGE
Store at +2°C to +8°C (+35°F to +46°F).
Avoid freezing, which may damage the diluent bottle.
Do not use after expiration date.
REFERENCES
- JANEWAY C. A., ROSEN F. S.: The Gamma Globulins: IV. Therapeutic Uses of Gamma Globulin. N. Engl. J. Med. 275, 1966, pp. 826-831.
- ROSEN F. S., WEDGWOOD R. J., EIBL M.: Primary Immunodeficiency Diseases. Report of a WHO Scientific Group. Clin. Immunol. Immunopathol. 40, 1986, pp. 166-196.
- EIBL M.: Treatment of Defects of Humoral Immunity. In: Primary Immunodeficiency Diseases; Birth Defects: Original Article Series. Edited by R. J. WEDGWOOD and F. S. ROSEN. Alan R. Liss, Inc. New York, Vol. 19, No. 3, 1983, pp. 193-200.
- EIBL M.: Intravenous Immunoglobulins: Clinical and Experimental Studies. In: Immunoglobulins: Characteristics and Uses of Intravenous Preparations. Edited by B. M. ALVING and J. S. FINLAYSON. U. S. Department of Health and Human Services, Public Health Service, FDA, DHHS Publication No. (FDA)-80-9005, 1979, pp. 23-30.
- WALDMANN T. A., et al.: Metabolism of Immunoglobulins. In: Progress in Allergy. Edited by P. KALLOS and B. H. WAKSMAN. Karger, Basel, Vol. 13, 1969, pp. 1-110.
- Data on File, Baxter AG, Vienna.
- BERNATOWSKA E., et al: Results of a Prospective Controlled Two-Dose Crossover Study with Intravenous Immunoglobulin and Comparison (Retrospective) with Plasma Treatment. Clin. Immunol. Immunopathol. 43, 1987, pp. 153-162.
- NEWBURGER J. W., et al.: The Treatment of Kawasaki Syndrome with Intravenous Gamma Globulin. N. Engl. J. Med. 315, 1986, pp. 341-347.
- NEWBURGER J. W., et al.: A Single Intravenous Infusion of Gamma Globulin as Compared with Four Infusions in the Treatment of Acute Kawasaki Syndrome. N. Engl. J. Med. 324, 1991, pp. 1633-1639.
- CAYCO A. V., PERAZELLA M. A., HAYSLETT J. P.: Renal insufficiency after intravenous immune globulin therapy: A Report of Two Cases and an Analysis of the Literature. J Amer Soc Nephrology. 8, 1997, pp. 1788-1793.
- BURKS A. W., et al.: Anaphylactic Reactions after Gammaglobulin Administration in Patients with Hypogammaglobulinemia. Detection of IgG Antibodies to IgA. N. Engl. J. Med. 314, 1986, pp. 560-564.
- CUNNINGHAM-RUNDLES C., et al.: Reactions to Intravenous Gammaglobulin Infusions and Immune Complex Formation. In: Immuno Hemotherapy. A Guide to Immunoglobulin Prophylaxis and Therapy. Edited by U.E. NYDEGGER. Academic Press, London, 1982, pp. 447-450.
- LEIKOLA J., et al.: IgA-Induced Anaphylactic Transfusion Reactions: A Report of Four Cases. Blood. 42, 1973, pp. 111-119.
- THOMPSON R. A., REES-JONES A.: The Antibody Deficiency Syndrome: A Report on Current Management. J. Infect. 1, 1979, pp. 49-60.
- COPELAN E. A., STROHM P. L., KENNEDY M. S., TUTSCHKA P. J.: Hemolysis following intravenous immune globulin therapy. Transfusion. 26, 1986, pp. 410-412.
- THOMAS M. J., MISBAH S. A., CHAPEL H. M., JONES M., ELRINGTON G., NEWSOM-DAVIS J.: Hemolysis after high-dose intravenous Ig. Blood. 15, 1993, pp. 3789.
- WILSON J. R., BHOOPALAM N., FISHER M.: Hemoytic anemia associated with intravenous immunoglobulin. Muscle & Nerve. 20, 1997, pp. 1142-1145.
- KESSARY-SHOHAM H., LEVY Y., SHOENFELD Y., LORBER M., GERSHON H.: In vivo administration of intravenous immunoglobulin (IVIg) can lead to enhanced erythrocyte sequestration. J Autoimmune. 13, 1999, pp. 129-135.
- RIZK A., GORSON K. C., KENNEY L., WEINSTEIN R.: Transfusion-related acute lung injury after the infusion of IVIG. Transfusion. 41, 2001, pp. 264-268.
- DALAKAS M. C.: High-dose intravenous immunoglobulin and serum viscosity: Risk of precipitating thromboembolic events. Neurology. 44, 2: 1994, pp. 223-226.
- WOODRUFF R. K., GRIGG A. P., FIRKIN F. C., SMITH I. L.: Fatal thrombotic events during treatment of autoimmune thrombocytopenia with intravenous immunoglobulin in elderly patients. Lancet. 2, 1986, pp. 217-218.
- WOLBERG A. S., KON R. H., MONROE D. M., HOFFMAN M.: Coagulation factor XI is a contaminant in intravenous immunoglobulin preparations. Am J Hematol. 65, 2000, pp. 30-34.
- WINWARD D. B., BROPHY M. T.: Acute renal failure after administration of intravenous immunoglobulin: review of the literature and case report. Pharmacotherapy. 15, 1995, pp. 765-772.
- PHILLIPS A. O.: Renal failure and intravenous immunoglobulin (letter, comment). Clin Nephrol. 36, 1992, pp. 83-86.
- ANDERSON W., BETHEA W.: Renal lesions following administration of hypertonic solutions of sucrose. JAMA. 114, 1940, pp. 1983-1987.
- LINDBERG H., WALD A.: Renal changes following the administration of hypertonic solutions. Arch Intern Med. 63, 1939, pp. 907-918.
- RIGDON R. H., CARDWELL E. S.: Renal lesions following the intravenous injection of hypertonic solution of sucrose: A clinical and experimental study. Arch Intern Med. 69, 1942, pp. 670-690.
- EIBL M., et al.: Safety and Efficacy of a Monomeric, Functionally Intact Intravenous IgG Preparation in Patients with Primary Immunodeficiency Syndromes. Clin. Immunol. Immunopathol. 31, 1984, pp. 151-160.
- PIERCE LR, JAIN N.: Risks associated with the use of intravenous immunoglobulin. Trans Med Rev. 17, 2003, pp. 241-251.
- TAN E., HAJINAZARIAN M., BAY, et al.: Acute renal failure resulting from intravenous immunoglobulin therapy. Arch Neurology. 50, 1993, pp. 137-139.
BIBLIOGRAPHY
ALVING B. M., FINLAYSON J. S. (Eds.): Immunoglobulins: Characteristics and Uses of Intravenous Preparations. U.S. Department of Health and Human Services, Public Health Service, DHHS Publication No. (FDA)-80-9005, 1979.
AMMANN A. J., ASHMAN R. F., BUCKLEY R. H., HARDIE W. R., KRANTMANN H. J., NELSON J., OCHS H., STIEHM E. R., TILLER T., WARA D. W., WEDGWOOD R.: Use of Intravenous g-Globulin in Antibody Immunodeficiency: Results of a Multicenter Controlled Trial. Clin. Immunol. Immunopathol. 22, 1982, pp. 60-67.
BARANDUN S., SKVARIL F., MORELL A.: Prophylaxe und Therapie mit g-Globulin. Allgemeine Charakterisierung und klinische Anwendung von g-Globulin-Präparaten. Schweiz. med. Wschr. 106, 1976, pp. 533-542.
BARANDUN S., MORELL A., SKVARIL F.: Clinical Use of Intravenous Gamma-Globulin. Biblthca haemat. 46, 1980, pp. 170-174.
BUCKLEY R. H.: Long Term Use of Intravenous Immune Globulin in Patients with Primary Immunodeficiency Diseases: Inadequacy of Current Dosage Practices and Approaches to the Problem. J. Clin. Immunol. 2 (Suppl.) 1982, pp. 15S-21S.
EIBL. M.: Treatment of Defects of Humoral Immunity. In: Primary Immunodeficiency Diseases; Birth Defects: Original Articles Series. Edited by R. J. WEDGWOOD and F. S. ROSEN. Alan R. Liss, Inc. New York, Vol. 19, No. 3, 1983, pp. 193-200.
KISHIMOTO S.: The Application of Immunoglobulin Preparations. Proc. Symp. Immunoglob., 1979, pp. 24-29.
KOBAYASHI M.: Replacement Therapy for Immunodeficiency Syndrome. Proc. Symp. on Immunoglobulin Therapy (Ed.: K. Mashimo) Tokyo, 1979, pp. 94-100.
LITMAN G. W., GOOD R. A. (Eds.): Immunoglobulins. Comprehensive Immunology 5. (Series editors: R. A. Good, S. B. Day). Plenum Medical Book Company, New York and London, 1978.
MAGILAVY D. B., CASSIDY J. T., TUBERGEN D. G., PETTY R. E., CHISHOLM R., McCALL K.: Intravenous Gamma Globulin in the Management of Patients with Hypogammaglobulinemia. J. Allergy Clin. Immunol. 61, 1978, pp. 378-383.
MAZZUCCONI M. G., MELONI G., BOTTINI F., ROMOLI D.: Sperimentazione Clinica e Tollerabilit[agrave][nbsp ] di un Nuovo Preparato di Immunoglobuline per Uso Endovenoso. Quaderni di Medicina e Chirurgia, 43; Suppl. a Malattie del Torace e Cardiovascolari, Vol. VII, 1975.
MORELL A., SCH[Uuml ]RCH B., RYSER D., HOFER F., SKVARIL F., BARANDUN S.: In vivo Behaviour of Gamma Globulin Preparations. Vox Sang. 38, 1980, pp. 272-283.
MORELL A., BARANDUN S.: Substitution mit Immunglobulinen bei primärem Antikörpermangelsyndrom. Beitr. Infusions-therapie klin. Ernähr. 9, 1982, pp. 16-24.
NOLTE M. T., PIROFSKY B., GERRITZ G. A., GOLDING B.: Intravenous Immunoglobulin Therapy for Antibody Deficiency. Clin. Exp. Immunol. 36, 1979, pp. 237-243.
R[Ouml ]MER J., MORGENTHALER J.-J., SCHERZ R., SKVARIL F.: Characterization of Various Immunoglobulin Preparations for Intravenous Application. I. Protein Composition and Antibody Content. Vox. Sang. 42, 1982, pp. 62-73.
R[Ouml ]MER J., SP[Auml ]TH P. J., SKVARIL F., NYDEGGER U. E.: Characterization of Various Immunoglobulin Preparations for Intravenous Application. II. Complement Activation and Binding to Staphylococcus Protein A. Vox. Sang. 42, 1982, pp. 74-80.
ROSEN F. S.: The Immunodeficiency Syndromes. In: Immunological Diseases. (Ed.: M. Samter). Third Edition, Vol. 1. Little, Brown and Comp., Boston, 1978, pp. 472-498.
ROSEN F. S. in: Panel Discussion on Indications and Limitations of Immunoglobulin Prophylaxis and Therapy. In: Immuno Hemotherapy. A Guide to Immunoglobulin Prophylaxis and Therapy, 1981, pp. 451-460.
SKVARIL F., PROBST M., AUDRAN R., STEINBUCH M.: Distribution of IgG Subclasses in Commercial and Some Experimental g-Globulin Preparations. Vox Sang. 32, 1977, pp. 335-338.
Benadryl is a trademark of Warner Lambert Consumer Healthcare
IVEEGAM is a trademark of Baxter AG. Baxter is a trademark of Baxter International, Inc.
IVEEGAM and Baxter are registered in the U.S. Patent and Trademark office.
U.S. Pat. Nos. 4,814,277, 4,886,758, 5,094,949, 5,122,373,
5,234,685 and 5,324,628Revised June 2004 Baxter Healthcare Corporation
© 2000 Baxter AG Westlake Village, CA 91362 USA All Rights Reserved U.S. License No. 140 6224000EH16
Subscribe to the "News" RSS Feed 
TOP ۞
