-
Neoral Oral Solution, Neoral Soft Gelatin Capsules (Novartis)
The following prescribing information is based on official labeling in effect July 2005.
Prescribing Information
WARNING
Only physicians experienced in management of systemic immunosuppressive therapy for the indicated disease should prescribe Neoral®. At doses used in solid organ transplantation, only physicians experienced in immunosuppressive therapy and management of organ transplant recipients should prescribe Neoral®. Patients receiving the drug should be managed in facilities equipped and staffed with adequate laboratory and supportive medical resources. The physician responsible for maintenance therapy should have complete information requisite for the follow-up of the patient.
Neoral®, a systemic immunosuppressant, may increase the susceptibility to infection and the development of neoplasia. In kidney, liver, and heart transplant patients Neoral® may be administered with other immunosuppressive agents. Increased susceptibility to infection and the possible development of lymphoma and other neoplasms may result from the increase in the degree of immunosuppression in transplant patients.
Neoral® Soft Gelatin Capsules (cyclosporine cap-sules, USP) MODIFIED and Neoral® Oral Solution (cyclosporine oral solution, USP) MODIFIED have increased bioavailability in comparison to Sandimmune® Soft Gelatin Capsules (cyclosporine capsules, USP) and Sandimmune® Oral Solution (cyclosporine oral solution, USP). Neoral® and Sandimmune® are not bioequivalent and cannot be used without physician supervision. For a given trough concentration, cyclosporine exposure will be greater with Neoral® than with Sandimmune®. If a patient who is receiving exceptionally high doses of Sandimmune® is converted to Neoral®, particular caution should be exercised. Cyclosporine blood concentrations should be monitored in transplant and rheumatoid arthritis patients taking Neoral® to avoid toxicity due to high concentrations. Dose adjustments should be made in transplant patients to minimize possible organ rejection due to low concentrations. Comparison of blood concentrations in the published literature with blood concentrations obtained using current assays must be done with detailed knowledge of the assay methods employed.
For Psoriasis Patients (See also Boxed WARNINGS above )
Psoriasis patients previously treated with PUVA and to a lesser extent, methotrexate or other immunosuppressive agents, UVB, coal tar, or radiation therapy, are at an increased risk of developing skin malignancies when taking Neoral®.
Cyclosporine, the active ingredient in Neoral®, in recommended dosages, can cause systemic hypertension and nephrotoxicity. The risk increases with increasing dose and duration of cyclosporine therapy. Renal dysfunction, including structural kidney damage, is a potential consequence of cyclosporine, and therefore, renal function must be monitored during therapy.
DESCRIPTION
Neoral® is an oral formulation of cyclosporine that immediately forms a microemulsion in an aqueous environment.
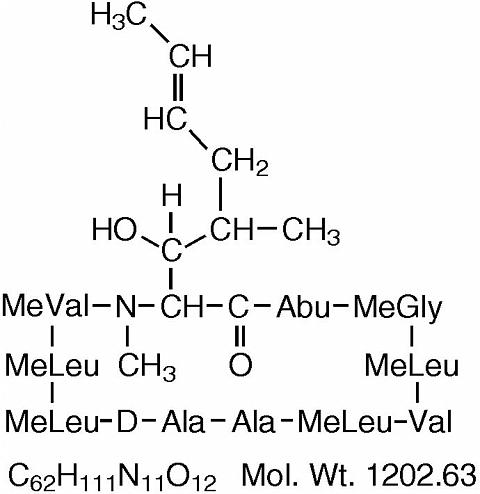
Cyclosporine, the active principle in Neoral®, is a cyclic polypeptide immunosuppressant agent consisting of 11 amino acids. It is produced as a metabolite by the fungus species Beauveria nivea .
Chemically, cyclosporine is designated as [ R -[ R *, R *-( E )]]-cyclic-(L-alanyl-D-alanyl- N -methyl-L-leucyl- N -meth-yl-L-leucyl- N -methyl-L-valyl-3-hydroxy- N ,4-dimethyl-L-2-amino-6-octenoyl-L-(alpha)-amino-butyryl- N -methylglycyl- N -methyl-L-leucyl-L-valyl- N -methyl-L-leucyl).
Neoral® Soft Gelatin Capsules (cyclosporine capsules, USP) MODIFIED are available in 25 mg and 100 mg strengths.
Each 25 mg capsule contains:
cyclosporine ................................................................ 25 mg
alcohol, USP dehydrated ................ 11.9% v/v (9.5% wt/vol.)
Each 100 mg capsule contains:
cyclosporine .............................................................. 100 mg
alcohol, USP dehydrated ................ 11.9% v/v (9.5% wt/vol.)
Inactive Ingredients: Corn oil-mono-di-triglycerides, polyoxyl 40 hydrogenated castor oil NF, DL-(alpha)-tocopherol USP, gelatin NF, glycerol, iron oxide black, propylene glycol USP, titanium dioxide USP, carmine, and other ingredients.
Neoral® Oral Solution (cyclosporine oral solution, USP) modified is available in 50 mL bottles.
Each mL contains:
cyclosporine ........................................................ 100 mg/mL
alcohol, USP dehydrated ................ 11.9% v/v (9.5% wt/vol.)
Inactive Ingredients: Corn oil-mono-di-triglycerides, polyoxyl 40 hydrogenated castor oil NF, DL-(alpha)-tocopherol USP, propylene glycol USP.
The chemical structure of cyclosporine (also known as cyclosporin A) is:
CLINICAL PHARMACOLOGY
Cyclosporine is a potent immunosuppressive agent that in animals prolongs survival of allogeneic transplants involving skin, kidney, liver, heart, pancreas, bone marrow, small intestine, and lung. Cyclosporine has been demonstrated to suppress some humoral immunity and to a greater extent, cell-mediated immune reactions such as allograft rejection, delayed hypersensitivity, experimental allergic encephalomyelitis, Freund's adjuvant arthritis, and graft vs. host disease in many animal species for a variety of organs.
The effectiveness of cyclosporine results from specific and reversible inhibition of immunocompetent lymphocytes in the G 0 - and G 1 -phase of the cell cycle. T-lymphocytes are preferentially inhibited. The T-helper cell is the main target, although the T-suppressor cell may also be suppressed. Cyclosporine also inhibits lymphokine production and release including interleukin-2.
No effects on phagocytic function (changes in enzyme secretions, chemotactic migration of granulocytes, macrophage migration, carbon clearance in vivo ) have been detected in animals. Cyclosporine does not cause bone marrow suppression in animal models or man.
Pharmacokinetics: The immunosuppressive activity of cyclosporine is primarily due to parent drug. Following oral administration, absorption of cyclosporine is incomplete. The extent of absorption of cyclosporine is dependent on the individual patient, the patient population, and the formulation. Elimination of cyclosporine is primarily biliary with only 6% of the dose (parent drug and metabolites) excreted in urine. The disposition of cyclosporine from blood is generally biphasic, with a terminal half-life of approximately 8.4 hours (range 5-18 hours). Following intravenous administration, the blood clearance of cyclosporine (assay: HPLC) is approximately 5-7 mL/min/kg in adult recipients of renal or liver allografts. Blood cyclosporine clearance appears to be slightly slower in cardiac transplant patients.
The Neoral® Soft Gelatin Capsules (cyclosporine capsules, USP) MODIFIED and Neoral® Oral Solution (cyclosporine oral solution, USP) MODIFIED are bioequivalent. Neoral® Oral Solution diluted with orange juice or apple juice is bioequivalent to Neoral Oral Solution diluted with water. The effect of milk on the bioavailability of cyclosporine when administered as Neoral Oral Solution has not been evaluated.
The relationship between administered dose and exposure (area under the concentration versus time curve, AUC) is linear within the therapeutic dose range. The intersubject variability (total, %CV) of cyclosporine exposure (AUC) when Neoral® or Sandimmune® is administered ranges from approximately 20% to 50% in renal transplant patients. This intersubject variability contributes to the need for individualization of the dosing regimen for optimal therapy (see DOSAGE AND ADMINISTRATION ). Intrasubject variability of AUC in renal transplant recipients (%CV) was 9%-21% for Neoral® and 19%-26% for Sandimmune®. In the same studies, intrasubject variability of trough concentrations (%CV) was 17%-30% for Neoral® and 16%-38% for Sandimmune®.
Absorption: Neoral® has increased bioavailability compared to Sandimmune®. The absolute bioavailability of cyclosporine administered as Sandimmune® is dependent on the patient population, estimated to be less than 10% in liver transplant patients and as great as 89% in some renal transplant patients. The absolute bioavailability of cyclosporine administered as Neoral® has not been determined in adults. In studies of renal transplant, rheumatoid arthritis and psoriasis patients, the mean cyclosporine AUC was approximately 20% to 50% greater and the peak blood cyclosporine concentration (C max ) was approximately 40% to 106% greater following administration of Neoral® compared to following administration of Sandimmune®. The dose normalized AUC in de novo liver transplant patients administered Neoral® 28 days after transplantation was 50% greater and C max was 90% greater than in those patients administered Sandimmune®. AUC and C max are also increased (Neoral® relative to Sandimmune®) in heart transplant patients, but data are very limited. Although the AUC and C max values are higher on Neoral® relative to Sandimmune®, the pre-dose trough concentrations (dose-normalized) are similar for the two formulations.
Following oral administration of Neoral®, the time to peak blood cyclosporine concentrations (T max ) ranged from 1.5-2.0 hours. The administration of food with Neoral® decreases the cyclosporine AUC and C max . A high fat meal (669 kcal, 45 grams fat) consumed within one-half hour before Neoral® administration decreased the AUC by 13% and C max by 33%. The effects of a low fat meal (667 kcal, 15 grams fat) were similar.
The effect of T-tube diversion of bile on the absorption of cyclosporine from Neoral® was investigated in eleven de novo liver transplant patients. When the patients were administered Neoral® with and without T-tube diversion of bile, very little difference in absorption was observed, as measured by the change in maximal cyclosporine blood concentrations from pre-dose values with the T-tube closed relative to when it was open: 6.9±41% (range -55% to 68%).
Pharmacokinetic Parameters (mean±SD) Patient PopulationDose/day 1
(mg/d)Dose/weight
(mg/kg/d)AUC 2
(ng·hr/mL)C max
(ng/mL)Trough 3
(ng/mL)CL/F
(mL/min)CL/F
(mL/min/kg)De novo renal transplant 4
Week 4 (N=37)597±174 7.95±2.81 8772±2089 1802±428 361±129 593±204 7.8±2.9 Stable renal transplant 4
(N=55)344±122 4.10±1.58 6035±2194 1333±469 251±116 492±140 5.9±2.1 De novo liver transplant 5
Week 4 (N=18)458±190 6.89±3.68 7187±2816 1555±740 268±101 577±309 8.6±5.7 De novo rheumatoid arthritis 6 (N=23)182±55.6 2.37±0.36 2641±877 728±263 96.4±37.7 613±196 8.3±2.8 De novo psoriasis 6
Week 4 (N=18)189±69.8 2.48±0.65 2324±1048 655±186 74.9±46.7 723±186 10.2±3.9 1 Total daily dose was divided into two doses administered every 12 hours 2 AUC was measured over one dosing interval 3 Trough concentration was measured just prior to the morning Neoral® dose, approximately 12 hours after the previous dose 4 Assay: TDx specific monoclonal fluorescence polarization immunoassay 5 Assay: Cyclo-trac specific monoclonal radioimmunoassay 6 Assay: INCSTAR specific monoclonal radioimmunoassay Distribution: Cyclosporine is distributed largely outside the blood volume. The steady state volume of distribution during intravenous dosing has been reported as 3-5 L/kg in solid organ transplant recipients. In blood, the distribution is concentration dependent. Approximately 33%-47% is in plasma, 4%-9% in lymphocytes, 5%-12% in granulocytes, and 41%-58% in erythrocytes. At high concentrations, the binding capacity of leukocytes and erythrocytes becomes saturated. In plasma, approximately 90% is bound to proteins, primarily lipoproteins. Cyclosporine is excreted in human milk. (See PRECAUTIONS , Nursing Mothers )
Metabolism: Cyclosporine is extensively metabolized by the cytochrome P-450 3A enzyme system in the liver, and to a lesser degree in the gastrointestinal tract, and the kidney. The metabolism of cyclosporine can be altered by the co-administration of a variety of agents. (See PRECAUTIONS , Drug Interactions ) At least 25 metabolites have been identified from human bile, feces, blood, and urine. The biological activity of the metabolites and their contributions to toxicity are considerably less than those of the parent compound. The major metabolites (M1, M9, and M4N) result from oxidation at the 1-beta, 9-gamma, and 4-N-demethylated positions, respectively. At steady state following the oral administration of Sandimmune®, the mean AUCs for blood concentrations of M1, M9, and M4N are about 70%, 21%, and 7.5% of the AUC for blood cyclosporine concentrations, respectively. Based on blood concentration data from stable renal transplant patients (13 patients administered Neoral® and Sandimmune® in a crossover study), and bile concentration data from de novo liver transplant patients (4 administered Neoral®, 3 administered Sandimmune®), the percentage of dose present as M1, M9, and M4N metabolites is similar when either Neoral® or Sandimmune® is administered.
Excretion: Only 0.1% of a cyclosporine dose is excreted unchanged in the urine. Elimination is primarily biliary with only 6% of the dose (parent drug and metabolites) excreted in the urine. Neither dialysis nor renal failure alter cyclosporine clearance significantly.
Drug Interactions: (See PRECAUTIONS , Drug Interactions ) When diclofenac or methotrexate was co-administered with cyclosporine in rheumatoid arthritis patients, the AUC of diclofenac and methotrexate, each was significantly increased. (See PRECAUTIONS , Drug Interactions ) No clinically significant pharmacokinetic interactions occurred between cyclosporine and aspirin, ketoprofen, piroxicam, or indomethacin.
Special Populations: Pediatric Population: Pharmacokinetic data from pediatric patients administered Neoral® or Sandimmune® are very limited. In 15 renal transplant patients aged 3-16 years, cyclosporine whole blood clearance after IV administration of Sandimmune® was 10.6±3.7 mL/min/kg (assay: Cyclo-trac specific RIA). In a study of 7 renal transplant patients aged 2-16, the cyclosporine clearance ranged from 9.8-15.5 mL/min/kg. In 9 liver transplant patients aged 0.6-5.6 years, clearance was 9.3±5.4 mL/min/kg (assay: HPLC).
In the pediatric population, Neoral® also demonstrates an increased bioavailability as compared to Sandimmune®. In 7 liver de novo transplant patients aged 1.4-10 years, the absolute bioavailability of Neoral® was 43% (range 30%-68%) and for Sandimmune® in the same individuals absolute bioavailability was 28% (range 17%-42%).
Pediatric Pharmacokinetic Parameters (mean±SD) Patient PopulationDose/day
(mg/d)Dose/weight
(mg/kg/d)AUC 1
(ng·hr/mL)C max
(ng/mL)CL/F
(mL/min)CL/F
(mL/min/kg)Stable liver transplant 2Age 2-8, Dosed TID (N=9)101±25 5.95±1.32 2163±801 629±219 285±94 16.6±4.3 Age 8-15, Dosed BID (N=8)188±55 4.96±2.09 4272±1462 975±281 378±80 10.2±4.0 Stable liver transplant 3Age 3, Dosed BID (N=1)120 8.33 5832 1050 171 11.9 Age 8-15, Dosed BID (N=5)158±55 5.51±1.91 4452±2475 1013±635 328±121 11.0±1.9 Stable renal transplant 3Age 7-15, Dosed BID (N=5)328±83 7.37±4.11 6922±1988 1827±487 418±143 8.7±2.9 1 AUC was measured over one dosing interval 2 Assay: Cyclo-trac specific monoclonal radioimmunoassay 3 Assay: TDx specific monoclonal fluorescence polarization immunoassay Geriatric Population: Comparison of single dose data from both normal elderly volunteers (N=18, mean age 69 years) and elderly rheumatoid arthritis patients (N=16, mean age 68 years) to single dose data in young adult volunteers (N=16, mean age 26 years) showed no significant difference in the pharmacokinetic parameters.
CLINICAL TRIALS
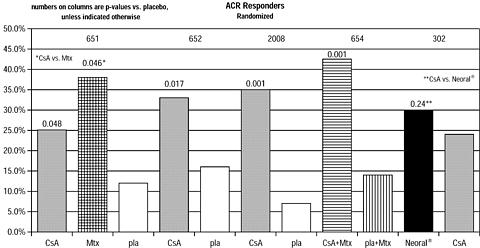
Rheumatoid Arthritis: The effectiveness of Sandimmune® and Neoral® in the treatment of severe rheumatoid arthritis was evaluated in 5 clinical studies involving a total of 728 cyclosporine treated patients and 273 placebo treated patients.
A summary of the results is presented for the "responder" rates per treatment group, with a responder being defined as a patient having completed the trial with a 20% improvement in the tender and the swollen joint count and a 20% improvement in 2 of 4 of investigator global, patient global, disability, and erythrocyte sedimentation rates (ESR) for the Studies 651 and 652 and 3 of 5 of investigator global, patient global, disability, visual analog pain, and ESR for Studies 2008, 654 and 302.
Study 651 enrolled 264 patients with active rheumatoid arthritis with at least 20 involved joints, who had failed at least one major RA drug, using a 3:3:2 randomization to one of the following three groups: (1) cyclosporine dosed at 2.5-5 mg/kg/day, (2) methotrexate at 7.5-15 mg/week, or (3) placebo. Treatment duration was 24 weeks. The mean cyclosporine dose at the last visit was 3.1 mg/kg/day. See Graph below .
Study 652 enrolled 250 patients with active RA with >6 active painful or tender joints who had failed at least one major RA drug. Patients were randomized using a 3:3:2 randomization to 1 of 3 treatment arms: (1) 1.5-5 mg/kg/day of cyclosporine, (2) 2.5-5 mg/kg/day of cyclosporine, and (3) placebo. Treatment duration was 16 weeks. The mean cyclosporine dose for group 2 at the last visit was 2.92 mg/kg/day. See Graph below .
Study 2008 enrolled 144 patients with active RA and >6 active joints who had unsuccessful treatment courses of aspirin and gold or Penicillamine. Patients were randomized to 1 of 2 treatment groups (1) cyclosporine 2.5-5 mg/kg/day with adjustments after the first month to achieve a target trough level and (2) placebo. Treatment duration was 24 weeks. The mean cyclosporine dose at the last visit was 3.63 mg/kg/day. See Graph below .
Study 654 enrolled 148 patients who remained with active joint counts of 6 or more despite treatment with maximally tolerated methotrexate doses for at least three months. Patients continued to take their current dose of methotrexate and were randomized to receive, in addition, one of the following medications: (1) cyclosporine 2.5 mg/kg/day with dose increases of 0.5 mg/kg/day at weeks 2 and 4 if there was no evidence of toxicity and further increases of 0.5 mg/kg/day at weeks 8 and 16 if a <30% decrease in active joint count occurred without any significant toxicity; dose decreases could be made at any time for toxicity or (2) placebo. Treatment duration was 24 weeks. The mean cyclosporine dose at the last visit was 2.8 mg/kg/day (range: 1.3-4.1). See Graph below .
Study 302 enrolled 299 patients with severe active RA, 99% of whom were unresponsive or intolerant to at least one prior major RA drug. Patients were randomized to 1 of 2 treatment groups (1) Neoral® and (2) cyclosporine, both of which were started at 2.5 mg/kg/day and increased after 4 weeks for inefficacy in increments of 0.5 mg/kg/day to a maximum of 5 mg/kg/day and decreased at any time for toxicity. Treatment duration was 24 weeks. The mean cyclosporine dose at the last visit was 2.91 mg/kg/day (range: 0.72-5.17) for Neoral® and 3.27 mg/kg/day (range: 0.73-5.68) for cyclosporine. See Graph below .
INDICATIONS AND USAGE
Kidney, Liver, and Heart Transplantation: Neoral® is indicated for the prophylaxis of organ rejection in kidney, liver, and heart allogeneic transplants. Neoral® has been used in combination with azathioprine and corticosteroids.
Rheumatoid Arthritis: Neoral® is indicated for the treatment of patients with severe active, rheumatoid arthritis where the disease has not adequately responded to methotrexate. Neoral® can be used in combination with methotrexate in rheumatoid arthritis patients who do not respond adequately to methotrexate alone.
Psoriasis: Neoral® is indicated for the treatment of adult, nonimmunocompromised patients with severe (i.e., extensive and/or disabling), recalcitrant, plaque psoriasis who have failed to respond to at least one systemic therapy (e.g., PUVA, retinoids, or methotrexate) or in patients for whom other systemic therapies are contraindicated, or cannot be tolerated.
While rebound rarely occurs, most patients will experience relapse with Neoral® as with other therapies upon cessation of treatment.
CONTRAINDICATIONS
General: Neoral® is contraindicated in patients with a hypersensitivity to cyclosporine or to any of the ingredients of the formulation.
Rheumatoid Arthritis: Rheumatoid arthritis patients with abnormal renal function, uncontrolled hypertension, or malignancies should not receive Neoral®.
Psoriasis: Psoriasis patients who are treated with Neoral® should not receive concomitant PUVA or UVB therapy, methotrexate or other immunosuppressive agents, coal tar or radiation therapy. Psoriasis patients with abnormal renal function, uncontrolled hypertension, or malignancies should not receive Neoral®.
WARNINGS
(See also Boxed WARNING )
All Patients: Cyclosporine, the active ingredient of Neoral® can cause nephrotoxicity and hepatotoxicity. The risk increases with increasing doses of cyclosporine. Renal dysfunction including structural kidney damage is a potential consequence of Neoral ® and therefore renal function must be monitored during therapy. Care should be taken in using cyclosporine with nephrotoxic drugs. (See PRECAUTIONS )
Patients receiving Neoral® require frequent monitoring of serum creatinine. (See Special Monitoring under DOSAGE AND ADMINISTRATION ) Elderly patients should be monitored with particular care, since decreases in renal function also occur with age. If patients are not properly monitored and doses are not properly adjusted, cyclosporine therapy can be associated with the occurrence of structural kidney damage and persistent renal dysfunction.
An increase in serum creatinine and BUN may occur during Neoral® therapy and reflect a reduction in the glomerular filtration rate. Impaired renal function at any time requires close monitoring, and frequent dosage adjustment may be indicated. The frequency and severity of serum creatinine elevations increase with dose and duration of cyclosporine therapy. These elevations are likely to become more pronounced without dose reduction or discontinuation.
Because Neoral® is not bioequivalent to Sandimmune®, conversion from Neoral® to Sandimmune® using a 1:1 ratio (mg/kg/day) may result in lower cyclosporine blood concentrations. Conversion from Neoral® to Sandimmune® should be made with increased monitoring to avoid the potential of underdosing.
Kidney, Liver, and Heart Transplant: Cyclosporine, the active ingredient of Neoral®, can cause nephrotoxicity and hepatotoxicity when used in high doses. It is not unusual for serum creatinine and BUN levels to be elevated during cyclosporine therapy. These elevations in renal transplant patients do not necessarily indicate rejection, and each patient must be fully evaluated before dosage adjustment is initiated.
Based on the historical Sandimmune® experience with oral solution, nephrotoxicity associated with cyclosporine had been noted in 25% of cases of renal transplantation, 38% of cases of cardiac transplantation, and 37% of cases of liver transplantation. Mild nephrotoxicity was generally noted 2-3 months after renal transplant and consisted of an arrest in the fall of the pre-operative elevations of BUN and creatinine at a range of 35-45 mg/dl and 2.0-2.5 mg/dl respectively. These elevations were often responsive to cyclosporine dosage reduction.
More overt nephrotoxicity was seen early after transplantation and was characterized by a rapidly rising BUN and creatinine. Since these events are similar to renal rejection episodes, care must be taken to differentiate between them. This form of nephrotoxicity is usually responsive to cyclosporine dosage reduction.
Although specific diagnostic criteria which reliably differentiate renal graft rejection from drug toxicity have not been found, a number of parameters have been significantly associated with one or the other. It should be noted however, that up to 20% of patients may have simultaneous nephrotoxicity and rejection.
Nephrotoxicity vs. Rejection ParameterNephrotoxicityRejectionHistoryDonor >50 years old or hypotensiveProlonged kidney preservationProlonged anastomosis timeConcomitant nephrotoxic drugsAnti-donor immune responseRetransplant patientClinicalOften >6 weeks postop bProlonged initial nonfunction(acute tubular necrosis)Often <4 weeks postop bFever >37.5°CWeight gain >0.5 kgGraft swelling and tendernessDecrease in daily urine volume
>500 mL (or 50%)LaboratoryCyA serum trough level >200 ng/mLGradual rise in Cr (<0.15 mg/dl/day) aCr plateau <25% above baselineBUN/Cr >/=20CyA serum trough level <150 ng/mLRapid rise in Cr (>0.3 mg/dl/day) aCr >25% above baselineBUN/Cr <20BiopsyArteriolopathy (medial hypertrophy a , hyalinosis, nodular deposits, intimal thickening, endothelial vacuolization, progressive scarring)Endovasculitis c (proliferation a , intimal arteritis b , necrosis, sclerosis)Tubular atrophy, isometric vacuolization, isolated calcificationsTubulitis with RBC b and WBC b casts, some irregular vacuolizationMinimal edemaInterstitial edema c and hemorrhage bMild focal infiltrates cDiffuse moderate to severe mononuclear infiltrates dDiffuse interstitial fibrosis, often striped formGlomerulitis (mononuclear cells) cAspiration CytologyCyA deposits in tubular and endothelial cells Fine isometric vacuolization of tubular cellsInflammatory infiltrate with mononuclear phagocytes, macrophages, lymphoblastoid cells, and activated T-cells
These strongly express HLA-DR antigensUrine CytologyTubular cells with vacuolization and granularizationDegenerative tubular cells, plasma cells, and lymphocyturia >20% of sedimentManometryIntracapsular pressure <40 mm Hg bIntracapsular pressure >40 mm Hg bUltrasonographyUnchanged graft cross sectional areaIncrease in graft cross sectional area
AP diameter >/= Transverse diameterMagnetic Resonance
ImageryNormal appearanceLoss of distinct corticomedullary junction, swelling image intensity of parachyma approaching that of psoas, loss of hilar fatRadionuclide ScanNormal or generally decreased perfusion
Decrease in tubular function
( 131 I-hippuran) > decrease in perfusion
( 99m Tc DTPA)Patchy arterial flow
Decrease in perfusion > decrease in tubular function
Increased uptake of Indium 111 labeled platelets or Tc-99m in colloidTherapyResponds to decreased cyclosporineResponds to increased steroids or antilymphocyte globulina p < 0.05, b p < 0.01, c p < 0.001, d p < 0.0001
A form of a cyclosporine-associated nephropathy is characterized by serial deterioration in renal function and morphologic changes in the kidneys. From 5%-15% of transplant recipients who have received cyclosporine will fail to show a reduction in rising serum creatinine despite a decrease or discontinuation of cyclosporine therapy. Renal biopsies from these patients will demonstrate one or several of the following alterations: tubular vacuolization, tubular microcalcifications, peritubular capillary congestion, arteriolopathy, and a striped form of interstitial fibrosis with tubular atrophy. Though none of these morphologic changes is entirely specific, a diagnosis of cyclosporine-associated structural nephrotoxicity requires evidence of these findings.
When considering the development of cyclosporine-associated nephropathy, it is noteworthy that several authors have reported an association between the appearance of interstitial fibrosis and higher cumulative doses or persistently high circulating trough levels of cyclosporine. This is particularly true during the first 6 post-transplant months when the dosage tends to be highest and when, in kidney recipients, the organ appears to be most vulnerable to the toxic effects of cyclosporine. Among other contributing factors to the development of interstitial fibrosis in these patients are prolonged perfusion time, warm ischemia time, as well as episodes of acute toxicity, and acute and chronic rejection. The reversibility of interstitial fibrosis and its correlation to renal function have not yet been determined. Reversibility of arteriolopathy has been reported after stopping cyclosporine or lowering the dosage.
Impaired renal function at any time requires close monitoring, and frequent dosage adjustment may be indicated.
In the event of severe and unremitting rejection, when rescue therapy with pulse steroids and monoclonal antibodies fail to reverse the rejection episode, it may be preferable to switch to alternative immunosuppressive therapy rather than increase the Neoral® dose to excessive levels.
Occasionally patients have developed a syndrome of thrombocytopenia and microangiopathic hemolytic anemia which may result in graft failure. The vasculopathy can occur in the absence of rejection and is accompanied by avid platelet consumption within the graft as demonstrated by Indium 111 labeled platelet studies. Neither the pathogenesis nor the management of this syndrome is clear. Though resolution has occurred after reduction or discontinuation of cyclosporine and 1) administration of streptokinase and heparin or 2) plasmapheresis, this appears to depend upon early detection with Indium 111 labeled platelet scans. (See ADVERSE REACTIONS )
Significant hyperkalemia (sometimes associated with hyperchloremic metabolic acidosis) and hyperuricemia have been seen occasionally in individual patients.
Hepatotoxicity associated with cyclosporine use had been noted in 4% of cases of renal transplantation, 7% of cases of cardiac transplantation, and 4% of cases of liver transplantation. This was usually noted during the first month of therapy when high doses of cyclosporine were used and consisted of elevations of hepatic enzymes and bilirubin. The chemistry elevations usually decreased with a reduction in dosage.
As in patients receiving other immunosuppressants, those patients receiving cyclosporine are at increased risk for development of lymphomas and other malignancies, particularly those of the skin. The increased risk appears related to the intensity and duration of immunosuppression rather than to the use of specific agents. Because of the danger of oversuppression of the immune system resulting in increased risk of infection or malignancy, a treatment regimen containing multiple immunosuppressants should be used with caution.
There have been reports of convulsions in adult and pediatric patients receiving cyclosporine, particularly in combination with high dose methylprednisolone.
Encephalopathy has been described both in postmarketing reports and in the literature. Manifestations include impaired consciousness, convulsions, visual disturbances (including blindness), loss of motor function, movement disorders and psychiatric disturbances. In many cases, changes in the white matter have been detected using imaging techniques and pathologic specimens. Predisposing factors such as hypertension, hypomagnesemia, hypocholesterolemia, high-dose corticosteroids, high cyclosporine blood concentrations, and graft-versus-host disease have been noted in many but not all of the reported cases. The changes in most cases have been reversible upon discontinuation of cyclosporine, and in some cases improvement was noted after reduction of dose. It appears that patients receiving liver transplant are more susceptible to encephalopathy than those receiving kidney transplant.
Care should be taken in using cyclosporine with nephrotoxic drugs. (See PRECAUTIONS )
Rheumatoid Arthritis: Cyclosporine nephropathy was detected in renal biopsies of 6 out of 60 (10%) rheumatoid arthritis patients after the average treatment duration of 19 months. Only one patient, out of these 6 patients, was treated with a dose </=4 mg/kg/day. Serum creatinine improved in all but one patient after discontinuation of cyclosporine. The "maximal creatinine increase" appears to be a factor in predicting cyclosporine nephropathy.
There is a potential, as with other immunosuppressive agents, for an increase in the occurrence of malignant lymphomas with cyclosporine. It is not clear whether the risk with cyclosporine is greater than that in rheumatoid arthritis patients or in rheumatoid arthritis patients on cytotoxic treatment for this indication. Five cases of lymphoma were detected: four in a survey of approximately 2,300 patients treated with cyclosporine for rheumatoid arthritis, and another case of lymphoma was reported in a clinical trial. Although other tumors (12 skin cancers, 24 solid tumors of diverse types, and 1 multiple myeloma) were also reported in this survey, epidemiologic analyses did not support a relationship to cyclosporine other than for malignant lymphomas.
Patients should be thoroughly evaluated before and during Neoral® treatment for the development of malignancies. Moreover, use of Neoral® therapy with other immunosuppressive agents may induce an excessive immunosuppression which is known to increase the risk of malignancy.
Psoriasis: (See also Boxed WARNINGS for Psoriasis ) Since cyclosporine is a potent immunosuppressive agent with a number of potentially serious side effects, the risks and benefits of using Neoral® should be considered before treatment of patients with psoriasis. Cyclosporine, the active ingredient in Neoral®, can cause nephrotoxicity and hypertension (see PRECAUTIONS ) and the risk increases with increasing dose and duration of therapy. Patients who may be at increased risk such as those with abnormal renal function, uncontrolled hypertension or malignancies, should not receive Neoral®.
Renal dysfunction is a potential consequence of Neoral® therefore renal function must be monitored during therapy.
Patients receiving Neoral® require frequent monitoring of serum creatinine. (See Special Monitoring under DOSAGE AND ADMINISTRATION ) Elderly patients should be monitored with particular care, since decreases in renal function also occur with age. If patients are not properly monitored and doses are not properly adjusted, cyclosporine therapy can cause structural kidney damage and persistent renal dysfunction.
An increase in serum creatinine and BUN may occur during Neoral® therapy and reflects a reduction in the glomerular filtration rate.
Kidney biopsies from 86 psoriasis patients treated for a mean duration of 23 months with 1.2-7.6 mg/kg/day of cyclosporine showed evidence of cyclosporine nephropathy in 18/86 (21%) of the patients. The pathology consisted of renal tubular atrophy and interstitial fibrosis. On repeat biopsy of 13 of these patients maintained on various dosages of cyclosporine for a mean of 2 additional years, the number with cyclosporine induced nephropathy rose to 26/86 (30%). The majority of patients (19/26) were on a dose of >/=5.0 mg/kg/day (the highest recommended dose is 4 mg/kg/day). The patients were also on cyclosporine for greater than 15 months (18/26) and/or had a clinically significant increase in serum creatinine for greater than 1 month (21/26). Creatinine levels returned to normal range in 7 of 11 patients in whom cyclosporine therapy was discontinued.
There is an increased risk for the development of skin and lymphoproliferative malignancies in cyclosporine-treated psoriasis patients. The relative risk of malignancies is comparable to that observed in psoriasis patients treated with other immunosuppressive agents.
Tumors were reported in 32 (2.2%) of 1439 psoriasis patients treated with cyclosporine worldwide from clinical trials. Additional tumors have been reported in 7 patients in cyclosporine postmarketing experience. Skin malignancies were reported in 16 (1.1%) of these patients; all but 2 of them had previously received PUVA therapy. Methotrexate was received by 7 patients. UVB and coal tar had been used by 2 and 3 patients, respectively. Seven patients had either a history of previous skin cancer or a potentially predisposing lesion was present prior to cyclosporine exposure. Of the 16 patients with skin cancer, 11 patients had 18 squamous cell carcinomas and 7 patients had 10 basal cell carcinomas.
There were two lymphoproliferative malignancies; one case of non-Hodgkin's lymphoma which required chemotherapy, and one case of mycosis fungoides which regressed spontaneously upon discontinuation of cyclosporine. There were four cases of benign lymphocytic infiltration: 3 regressed spontaneously upon discontinuation of cyclosporine, while the fourth regressed despite continuation of the drug. The remainder of the malignancies, 13 cases (0.9%), involved various organs.
Patients should not be treated concurrently with cyclosporine and PUVA or UVB, other radiation therapy, or other immunosuppressive agents, because of the possibility of excessive immunosuppression and the subsequent risk of malignancies. (See CONTRAINDICATIONS ) Patients should also be warned to protect themselves appropriately when in the sun, and to avoid excessive sun exposure. Patients should be thoroughly evaluated before and during treatment for the presence of malignancies remembering that malignant lesions may be hidden by psoriatic plaques. Skin lesions not typical of psoriasis should be biopsied before starting treatment. Patients should be treated with Neoral® only after complete resolution of suspicious lesions, and only if there are no other treatment options. (See Special Monitoring for Psoriasis Patients )
PRECAUTIONS
General: Hypertension: Cyclosporine is the active ingredient of Neoral®. Hypertension is a common side effect of cyclosporine therapy which may persist. (See ADVERSE REACTIONS and DOSAGE AND ADMINISTRATION for monitoring recommendations) Mild or moderate hypertension is encountered more frequently than severe hypertension and the incidence decreases over time. In recipients of kidney, liver, and heart allografts treated with cyclosporine, antihypertensive therapy may be required. (See Special Monitoring of Rheumatoid Arthritis and Psoriasis Patients ) However, since cyclosporine may cause hyperkalemia, potassium-sparing diuretics should not be used. While calcium antagonists can be effective agents in treating cyclosporine-associated hypertension, they can interfere with cyclosporine metabolism. (See Drug Interactions )
Vaccination: During treatment with cyclosporine, vaccination may be less effective; and the use of live attenuated vaccines should be avoided.
Special Monitoring of Rheumatoid Arthritis Patients: Before initiating treatment, a careful physical examination, including blood pressure measurements (on at least two occasions) and two creatinine levels to estimate baseline should be performed. Blood pressure and serum creatinine should be evaluated every 2 weeks during the initial 3 months and then monthly if the patient is stable. It is advisable to monitor serum creatinine and blood pressure always after an increase of the dose of nonsteroidal anti-inflammatory drugs and after initiation of new nonsteroidal anti-inflammatory drug therapy during Neoral® treatment. If co-administered with methotrexate, CBC and liver function tests are recommended to be monitored monthly. (See also Precautions , General, Hypertension )
In patients who are receiving cyclosporine, the dose of Neoral® should be decreased by 25%-50% if hypertension occurs. If hypertension persists, the dose of Neoral® should be further reduced or blood pressure should be con-trolled with antihypertensive agents. In most cases, blood pressure has returned to baseline when cyclosporine was discontinued.
In placebo-controlled trials of rheumatoid arthritis patients, systolic hypertension (defined as an occurrence of two systolic blood pressure readings >140 mmHg) and diastolic hypertension (defined as two diastolic blood pressure readings >90 mmHg) occurred in 33% and 19% of patients treated with cyclosporine, respectively. The corresponding placebo rates were 22% and 8%.
Special Monitoring for Psoriasis Patients: Before initiating treatment, a careful dermatological and physical examination, including blood pressure measurements (on at least two occasions) should be performed. Since Neoral® is an immunosuppressive agent, patients should be evaluated for the presence of occult infection on their first physical examination and for the presence of tumors initially, and throughout treatment with Neoral®. Skin lesions not typical for psoriasis should be biopsied before starting Neoral®. Patients with malignant or premalignant changes of the skin should be treated with Neoral® only after appropriate treatment of such lesions and if no other treatment option exists.
Baseline laboratories should include serum creatinine (on two occasions), BUN, CBC, serum magnesium, potassium, uric acid, and lipids.
The risk of cyclosporine nephropathy is reduced when the starting dose is low (2.5 mg/kg/day), the maximum dose does not exceed 4.0 mg/kg/day, serum creatinine is monitored regularly while cyclosporine is administered, and the dose of Neoral® is decreased when the rise in creatinine is greater than or equal to 25% above the patient's pretreatment level. The increase in creatinine is generally reversible upon timely decrease of the dose of Neoral® or its discontinuation.
Serum creatinine and BUN should be evaluated every 2 weeks during the initial 3 months of therapy and then monthly if the patient is stable. If the serum creatinine is greater than or equal to 25% above the patient's pretreatment level, serum creatinine should be repeated within two weeks. If the change in serum creatinine remains greater than or equal to 25% above baseline, Neoral® should be reduced by 25%-50%. If at any time the serum creatinine increases by greater than or equal to 50% above pretreatment level, Neoral® should be reduced by 25%-50%. Neoral® should be discontinued if reversibility (within 25% of baseline) of serum creatinine is not achievable after two dosage modifications. It is advisable to monitor serum creatinine after an increase of the dose of nonsteroidal anti-inflammatory drug and after initiation of new nonsteroidal anti-inflammatory therapy during Neoral® treatment.
Blood pressure should be evaluated every 2 weeks during the initial 3 months of therapy and then monthly if the patient is stable, or more frequently when dosage adjustments are made. Patients without a history of previous hypertension before initiation of treatment with Neoral®, should have the drug reduced by 25%-50% if found to have sustained hypertension. If the patient continues to be hypertensive despite multiple reductions of Neoral®, then Neoral® should be discontinued. For patients with treated hypertension, before the initiation of Neoral® therapy, their medication should be adjusted to control hypertension while on Neoral®. Neoral® should be discontinued if a change in hypertension management is not effective or tolerable.
CBC, uric acid, potassium, lipids, and magnesium should also be monitored every 2 weeks for the first 3 months of therapy, and then monthly if the patient is stable or more frequently when dosage adjustments are made. Neoral® dosage should be reduced by 25%-50% for any abnormality of clinical concern.
In controlled trials of cyclosporine in psoriasis patients, cyclosporine blood concentrations did not correlate well with either improvement or with side effects such as renal dysfunction.
Information for Patients: Patients should be advised that any change of cyclosporine formulation should be made cautiously and only under physician supervision because it may result in the need for a change in dosage.
Patients should be informed of the necessity of repeated laboratory tests while they are receiving cyclosporine. Patients should be advised of the potential risks during pregnancy and informed of the increased risk of neoplasia. Patients should also be informed of the risk of hypertension and renal dysfunction.
Patients should be advised that during treatment with cyclosporine, vaccination may be less effective and the use of live attenuated vaccines should be avoided.
Patients should be given careful dosage instructions. Neoral® Oral Solution (cyclosporine oral solution, USP) MODIFIED should be diluted, preferably with orange or apple juice that is at room temperature. The combination of Neoral® Oral Solution (cyclosporine oral solution, USP) MODIFIED with milk can be unpalatable.
Patients should be advised to take Neoral® on a consistent schedule with regard to time of day and relation to meals. Grapefruit and grapefruit juice affect metabolism, increasing blood concentration of cyclosporine, thus should be avoided.
Laboratory Tests: In all patients treated with cyclosporine, renal and liver functions should be assessed repeatedly by measurement of serum creatinine, BUN, serum bilirubin, and liver enzymes. Serum lipids, magnesium, and potassium should also be monitored. Cyclosporine blood concentrations should be routinely monitored in transplant patients (see DOSAGE AND ADMINISTRATION , Blood Concentration Monitoring in Transplant Patients ) , and periodically monitored in rheumatoid arthritis patients.
Drug Interactions: All of the individual drugs cited below are well substantiated to interact with cyclosporine. In addition, concomitant non-steroidal anti-inflammatory drugs, particularly in the setting of dehydration, may potentiate renal dysfunction.
Drugs That May Potentiate Renal DysfunctionAntibioticsAntineoplasticsAnti-inflammatory DrugsGastrointestinal Agentsgentamycintobramycinvancomycintrimethoprim with
sulfamethoxazolemelphalanazapropazondiclofenacnaproxensulindac
colchicinecimetidineranitidineAntifungalsImmunosuppressivesamphotericin B
ketoconazoletacrolimusDrugs That Alter Cyclosporine Concentrations: Compounds that decrease cyclosporine absorption such as orlistat should be avoided. Cyclosporine is extensively metabolized by cytochrome P-450 3A. Substances that inhibit this enzyme could decrease metabolism and increase cyclosporine concentrations. Substances that are inducers of cytochrome P-450 activity could increase metabolism and decrease cyclosporine concentrations. Monitoring of circulating cyclosporine concentrations and appropriate Neoral® dosage adjustment are essential when these drugs are used concomitantly. (See Blood Concentration Monitoring )
Drugs That Increase Cyclosporine ConcentrationsCalcium Channel BlockersAntifungalsAntibioticsGlucocorticoidsOther Drugs _____diltiazemnicardipineverapamilfluconazoleitraconazoleketoconazoleclarithromycinerythromycinquinupristin/
dalfopristinmethylprednisoloneallopurinolbromocriptinedanazolmetoclopramidecolchicineamiodarone
The HIV protease inhibitors (e.g., indinavir, nelfinavir, ritonavir, and saquinavir) are known to inhibit cytochrome P-450 3A and thus could potentially increase the concentrations of cyclosporine, however no formal studies of the interaction are available. Care should be exercised when these drugs are administered concomitantly.
Grapefruit and grapefruit juice affect metabolism, increasing blood concentrations of cyclosporine, thus should be avoided.
Drugs/Dietary Supplements That Decrease Cyclosporine ConcentrationsAntibioticsAnticonvulsantsOther Drugs/
Dietary SupplementsnafcillinrifampincarbamazepinephenobarbitalphenytoinoctreotideticlopidineorlistatSt. John's Wort
There have been reports of a serious drug interaction between cyclosporine and the herbal dietary supplement, St. John's Wort. This interaction has been reported to produce a marked reduction in the blood concentrations of cyclosporine, resulting in subtherapeutic levels, rejection of transplanted organs, and graft loss.
Rifabutin is known to increase the metabolism of other drugs metabolized by the cytochrome P-450 system. The interaction between rifabutin and cyclosporine has not been studied. Care should be exercised when these two drugs are administered concomitantly.
Nonsteroidal Anti-inflammatory Drug (NSAID) Interactions: Clinical status and serum creatinine should be closely monitored when cyclosporine is used with nonsteroidal anti-inflammatory agents in rheumatoid arthritis patients. (See WARNINGS )
Pharmacodynamic interactions have been reported to occur between cyclosporine and both naproxen and sulindac, in that concomitant use is associated with additive decreases in renal function, as determined by 99m Tc-diethylenetriaminepentaacetic acid (DTPA) and ( p -aminohippuric acid) PAH clearances. Although oncomitant administration of diclofenac does not affect blood levels of cyclosporine, it has been associated with approximate doubling of diclofenac blood levels and occasional reports of reversible decreases in renal function. Consequently, the dose of diclofenac should be in the lower end of the therapeutic range.
Methotrexate Interaction: Preliminary data indicate that when methotrexate and cyclosporine were co-administered to rheumatoid arthritis patients (N=20), methotrexate concentrations (AUCs) were increased approximately 30% and the concentrations (AUCs) of its metabolite, 7-hydroxy methotrexate, were decreased by approximately 80%. The clinical significance of this interaction is not known. Cyclosporine concentrations do not appear to have been altered (N=6).
Other Drug Interactions: Cyclosporine may reduce the clearance of digoxin, colchicine, prednisolone and HMG-CoA inhibitors (statins). Severe digitalis toxicity has been seen within days of starting cyclosporine in several patients taking digoxin. There are also reports on the potential of cyclosporine to enhance the toxic effects of colchicine such as myopathy and neuropathy, especially patients with renal dysfunction. If digoxin or colchicine are used concurrently with cyclosporine, close clinical observation is required in order to enable early detection of toxic manifestations of digoxin or colchicine, followed by reduction of dosage or its withdrawal.
Literature and postmarketing cases of myotoxicity, including muscle pain and weakness, myositis, and rhabdomyolysis, have been reported with concomitant administration of cyclosporine with lovastatin, simvastatin, atorvastatin, pravastatin and, rarely, fluvastatin. When concurrently administered with cyclosporine, the dosage of these statins should be reduced according to label recommendations. Statin therapy needs to be temporarily withheld or discontinued in patients with signs and symptoms myopathy or those with risk factors predisposing to severe renal injury, including renal failure, secondary to rhabdomyolysis.
Cyclosporine should not be used with potassium-sparing diuretics because hyperkalemia can occur.
During treatment with cyclosporine, vaccination may be less effective. The use of live vaccines should be avoided. Frequent gingival hyperplasia with nifedipine, and convulsions with high dose methylprednisolone have been reported.
Psoriasis patients receiving other immunosuppressive agents or radiation therapy (including PUVA and UVB) should not receive concurrent cyclosporine because of the possibility of excessive immunosuppression.
For additional information on Cyclosporine Drug Interactions please contact Novartis Medical Affairs Department at 888-NOW-NOVA [888-669-6682].
Carcinogenesis, Mutagenesis, and Impairment of Fertility: Carcinogenicity studies were carried out in male and female rats and mice. In the 78-week mouse study, evidence of a statistically significant trend was found for lymphomas in females, and the incidence of hepatocellular carcinomas in mid-dose males significantly exceeded the control value. In the 24-month rat study, pancreatic islet cell adenomas significantly exceeded the control rate in the low dose level. Doses used in the mouse and rat studies were 0.01 to 0.16 times the clinical maintenance dose (6 mg/kg). The hepatocellular carcinomas and pancreatic islet cell adenomas were not dose related. Published reports indicate that co-treatment of hairless mice with UV irradiation and cyclosporine or other immunosuppressive agents shorten the time to skin tumor formation compared to UV irradiation alone.
Cyclosporine was not mutagenic in appropriate test systems. Cyclosporine has not been found to be mutagenic/ genotoxic in the Ames Test, the V79-HGPRT Test, the micronucleus test in mice and Chinese hamsters, the chromosome-aberration tests in Chinese hamster bone marrow, the mouse dominant lethal assay, and the DNA-repair test in sperm from treated mice. A recent study analyzing sister chromatid exchange (SCE) induction by cyclosporine using human lymphocytes in vitro gave indication of a positive effect (i.e., induction of SCE), at high concentrations in this system.
No impairment in fertility was demonstrated in studies in male and female rats.
Widely distributed papillomatosis of the skin was observed after chronic treatment of dogs with cyclosporine at 9 times the human initial psoriasis treatment dose of 2.5 mg/kg, where doses are expressed on a body surface area basis. This papillomatosis showed a spontaneous regression upon discontinuation of cyclosporine.
An increased incidence of malignancy is a recognized complication of immunosuppression in recipients of organ transplants and patients with rheumatoid arthritis and psoriasis. The most common forms of neoplasms are non-Hodgkin's lymphoma and carcinomas of the skin. The risk of malignancies in cyclosporine recipients is higher than in the normal, healthy population but similar to that in patients receiving other immunosuppressive therapies. Reduction or discontinuance of immunosuppression may cause the lesions to regress.
In psoriasis patients on cyclosporine, development of malignancies, especially those of the skin has been reported. (See WARNINGS ) Skin lesions not typical for psoriasis should be biopsied before starting cyclosporine treatment. Patients with malignant or premalignant changes of the skin should be treated with cyclosporine only after appropriate treatment of such lesions and if no other treatment option exists.
Pregnancy: Pregnancy Category C. Cyclosporine was not teratogenic in appropriate test systems. Only at dose levels toxic to dams, were adverse effects seen in reproduction studies in rats. Cyclosporine has been shown to be embryo- and fetotoxic in rats and rabbits following oral administration at maternally toxic doses. Fetal toxicity was noted in rats at 0.8 and rabbits at 5.4 times the transplant doses in humans of 6.0 mg/kg, where dose corrections are based on body surface area. Cyclosporine was embryo- and fetotoxic as indicated by increased pre- and post-natal mortality and reduced fetal weight together with related skeletal retardation.
There are no adequate and well-controlled studies in pregnant women. Neoral® should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
The following data represent the reported outcomes of 116 pregnancies in women receiving cyclosporine during pregnancy, 90% of whom were transplant patients, and most of whom received cyclosporine throughout the entire gestational period. The only consistent patterns of abnormality were premature birth (gestational period of 28 to 36 weeks) and low birth weight for gestational age. Sixteen fetal losses occurred. Most of the pregnancies (85 of 100) were complicated by disorders; including, pre-eclampsia, eclampsia, premature labor, abruptio placentae, oligohydramnios, Rh incompatibility, and fetoplacental dysfunction. Pre-term delivery occurred in 47%. Seven malformations were reported in 5 viable infants and in 2 cases of fetal loss. Twenty-eight percent of the infants were small for gestational age. Neonatal complications occurred in 27%. Therefore, the risks and benefits of using Neoral® during pregnancy should be carefully weighed.
Because of the possible disruption of maternal-fetal interaction, the risk/benefit ratio of using Neoral® in psoriasis patients during pregnancy should carefully be weighed with serious consideration for discontinuation of Neoral®.
Nursing Mothers: Since cyclosporine is excreted in human milk, breast-feeding should be avoided.
Pediatric Use: Although no adequate and well-controlled studies have been completed in children, transplant recipients as young as one year of age have received Neoral® with no unusual adverse effects. The safety and efficacy of Neoral® treatment in children with juvenile rheumatoid arthritis or psoriasis below the age of 18 have not been established.
Geriatric Use: In rheumatoid arthritis clinical trials with cyclosporine, 17.5% of patients were age 65 or older. These patients were more likely to develop systolic hypertension on therapy, and more likely to show serum creatinine rises >/=50% above the baseline after 3-4 months of therapy.
Clinical studies of Neoral® in transplant and psoriasis patients did not include a sufficient number of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experiences have not identified differences in response between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
ADVERSE REACTIONS
Kidney, Liver, and Heart Transplantation: The principal adverse reactions of cyclosporine therapy are renal dysfunction, tremor, hirsutism, hypertension, and gum hyperplasia.
Hypertension, which is usually mild to moderate, may occur in approximately 50% of patients following renal transplantation and in most cardiac transplant patients.
Glomerular capillary thrombosis has been found in patients treated with cyclosporine and may progress to graft failure. The pathologic changes resembled those seen in the hemolytic-uremic syndrome and included thrombosis of the renal microvasculature, with platelet-fibrin thrombi occluding glomerular capillaries and afferent arterioles, microangiopathic hemolytic anemia, thrombocytopenia, and decreased renal function. Similar findings have been observed when other immunosuppressives have been employed post-transplantation.
Hypomagnesemia has been reported in some, but not all, patients exhibiting convulsions while on cyclosporine therapy. Although magnesium-depletion studies in normal subjects suggest that hypomagnesemia is associated with neurologic disorders, multiple factors, including hypertension, high dose methylprednisolone, hypocholesterolemia, and nephrotoxicity associated with high plasma concentrations of cyclosporine appear to be related to the neurological manifestations of cyclosporine toxicity.
In controlled studies, the nature, severity, and incidence of the adverse events that were observed in 493 transplanted patients treated with Neoral® were comparable with those observed in 208 transplanted patients who received Sandimmune® in these same studies when the dosage of the two drugs was adjusted to achieve the same cyclosporine blood trough concentrations.
Based on the historical experience with Sandimmune®, the following reactions occurred in 3% or greater of 892 patients involved in clinical trials of kidney, heart, and liver transplants.
Body SystemAdverse ReactionsRandomized Kidney
PatientsCyclosporine Patients
(Sandimmune®)Sandimmune®
(N=227) %Azathioprine
(N=228) %Kidney
(N=705) %Heart
(N=112) %Liver
(N=75) %GenitourinaryRenal Dysfunction32 6 25 38 37 CardiovascularHyertension26 18 13 53 27 Cramps4 <1 2 <1 0 SkinHirsutism21 <1 21 28 45 Acne6 8 2 2 1 Central Nervous SystemTremor12 0 21 31 55 Convulsions3 1 1 4 5 Headache2 <1 2 15 4 GastrointestinalGum Hyperplasia4 0 9 5 16 Diarrhea3 <1 3 4 8 Nausea/Vomiting2 <1 4 10 4 Hepatotoxicity<1 <1 4 7 4 Abdominal Discomfort<1 0 <1 7 0 Autonomic Nervous SystemParesthesia3 0 1 2 1 Flushing<1 0 4 0 4 HematopoieticLeukopenia2 19 <1 6 0 Lymphoma<1 0 1 6 1 RespiratorySinusitis<1 0 4 3 7 MiscellaneousGynecomastia<1 0 <1 4 3
Among 705 kidney transplant patients treated with cyclosporine oral solution (Sandimmune®) in clinical trials, the reason for treatment discontinuation was renal toxicity in 5.4%, infection in 0.9%, lack of efficacy in 1.4%, acute tubular necrosis in 1.0%, lymphoproliferative disorders in 0.3%, hypertension in 0.3%, and other reasons in 0.7% of the patients.
The following reactions occurred in 2% or less of Sandimmune®-treated patients: allergic reactions, anemia, anorexia, confusion, conjunctivitis, edema, fever, brittle fingernails, gastritis, hearing loss, hiccups, hyperglycemia, muscle pain, peptic ulcer, thrombocytopenia, tinnitus.
The following reactions occurred rarely: anxiety, chest pain, constipation, depression, hair breaking, hematuria, joint pain, lethargy, mouth sores, myocardial infarction, night sweats, pancreatitis, pruritus, swallowing difficulty, tingling, upper GI bleeding, visual disturbance, weakness, weight loss.
Infectious Complications in Historical Randomized Studies
in Renal Transplant Patients Using Sandimmune®ComplicationCyclosporine Treatment
(N=227)
% of ComplicationsAzathioprine with Steroids *
(N=228)
% of ComplicationsSepticemia5.3 4.8 Abscesses4.4 5.3 Systemic Fungal Infection2.2 3.9 Local Fungal Infection7.5 9.6 Cytomegalovirus4.8 12.3 Other Viral Infections15.9 18.4 Urinary Tract Infections21.1 20.2 Wound and Skin Infections7.0 10.1 Pneumonia6.2 9.2 *Some patients also received ALG. Rheumatoid Arthritis: The principal adverse reactions associated with the use of cyclosporine in rheumatoid arthritis are renal dysfunction (see WARNINGS ) , hypertension (see PRECAUTIONS ), headache, gastrointestinal disturbances, and hirsutism/hypertrichosis.
In rheumatoid arthritis patients treated in clinical trials within the recommended dose range, cyclosporine therapy was discontinued in 5.3% of the patients because of hypertension and in 7% of the patients because of increased creatinine. These changes are usually reversible with timely dose decrease or drug discontinuation. The frequency and severity of serum creatinine elevations increase with dose and duration of cyclosporine therapy. These elevations are likely to become more pronounced without dose reduction or discontinuation.
The following adverse events occurred in controlled clinical trials:
Neoral®/Sandimmune® Rheumatoid Arthritis
Percentage of Patients with Adverse Events >/=3% in any Cyclosporine Treated GroupStudies
651+652+2008Study
302Study
654Study
654Study
302Studies
651+652+2008Body
SystemPreferred
TermSandimmune® †
(N=269)Sandimmune®
(N=155)Methotrexate &
Sandimmune®
(N=74)Methotrexate
& Placebo
(N=73)Neoral®
(N=143)Placebo
(N=201)Autonomic Nervous System DisordersFlushing2% 2% 3% 0% 5% 2% Body As A Whole--General DisordersAccidental Trauma0% 1% 10% 4% 4% 0% Edema NOS *5% 14% 12% 4% 10% <1% Fatigue6% 3% 8% 12% 3% 7% Fever2% 3% 0% 0% 2% 4% Influenza-like symptoms<1% 6% 1% 0% 3% 2% Pain6% 9% 10% 15% 13% 4% Rigors1% 1% 4% 0% 3% 1% Cardiovascular DisordersArrhythmia2% 5% 5% 6% 2% 1% Chest Pain4% 5% 1% 1% 6% 1% Hypertension8% 26% 16% 12% 25% 2% Central and Peripheral Nervous System DisordersDizziness8% 6% 7% 3% 8% 3% Headache17% 23% 22% 11% 25% 9% Migraine2% 3% 0% 0% 3% 1% Paresthesia8% 7% 8% 4% 11% 1% Tremor8% 7% 7% 3% 13% 4% Gastrointestinal System DisordersAbdominal Pain15% 15% 15% 7% 15% 10% Anorexia3% 3% 1% 0% 3% 3% Diarrhea12% 12% 18% 15% 13% 8% Dyspepsia12% 12% 10% 8% 8% 4% Flatulence5% 5% 5% 4% 4% 1% Gastrointestinal
Disorder NOS *0% 2% 1% 4% 4% 0% Gingivitis4% 3% 0% 0% 0% 1% Gum Hyperplasia2% 4% 1% 3% 4% 1% Nausea23% 14% 24% 15% 18% 14% Rectal Hemorrhage0% 3% 0% 0% 1% 1% Stomatitis7% 5% 16% 12% 6% 8% Vomiting9% 8% 14% 7% 6% 5% Hearing and Vestibular DisordersEar Disorder NOS *0% 5% 0% 0% 1% 0% Metabolic and Nutritional DisordersHypomagnesemia0% 4% 0% 0% 6% 0% Musculoskeletal System DisordersArthropathy0% 5% 0% 1% 4% 0% Leg Cramps/Involuntary Muscle Contractions2% 11% 11% 3% 12% 1% Psychiatric DisordersDepression3% 6% 3% 1% 1% 2% Insomnia4% 1% 1% 0% 3% 2% RenalCreatinine elevations
>/=30%43% 39% 55% 19% 48% 13% Creatinine elevations
>/=50%24% 18% 26% 8% 18% 3% Reproductive Disorders, FemaleLeukorrhea1% 0% 4% 0% 1% 0% Menstrual Disorder3% 2% 1% 0% 1% 1% Respiratory System DisordersBronchitis1% 3% 1% 0% 1% 3% Coughing5% 3% 5% 7% 4% 4% Dyspnea5% 1% 3% 3% 1% 2% Infection NOS *9% 5% 0% 7% 3% 10% Pharyngitis3% 5% 5% 6% 4% 4% Pneumonia1% 0% 4% 0% 1% 1% Rhinitis0% 3% 11% 10% 1% 0% Sinusitis4% 4% 8% 4% 3% 3% Upper Respiratory Tract0% 14% 23% 15% 13% 0% Skin and Appendages DisordersAlopecia3% 0% 1% 1% 4% 4% Bullous Eruption1% 0% 4% 1% 1% 1% Hypertrichosis19% 17% 12% 0% 15% 3% Rash7% 12% 10% 7% 8% 10% Skin Ulceration1% 1% 3% 4% 0% 2% Urinary System DisordersDysuria0% 0% 11% 3% 1% 2% Micturition Frequency2% 4% 3% 1% 2% 2% NPN, Increased0% 19% 12% 0% 18% 0% Urinary Tract Infection0% 3% 5% 4% 3% 0% Vascular (Extracardiac) DisordersPurpura3% 4% 1% 1% 2% 0% *NOS = Not Otherwise Specified.
In addition, the following adverse events have been reported in 1% to <3% of the rheumatoid arthritis patients in the cyclosporine treatment group in controlled clinical trials.
Autonomic Nervous System: dry mouth, increased sweating;
Body as a Whole: allergy, asthenia, hot flushes, malaise, overdose, procedure NOS * , tumor NOS * , weight decrease, weight increase;
Cardiovascular: abnormal heart sounds, cardiac failure, myocardial infarction, peripheral ischemia;
Central and Peripheral Nervous System: hypoesthesia, neuropathy, vertigo;
Endocrine: goiter;
Gastrointestinal: constipation, dysphagia, enanthema, eructation, esophagitis, gastric ulcer, gastritis, gastroenteritis, gingival bleeding, glossitis, peptic ulcer, salivary gland enlargement, tongue disorder, tooth disorder;
Infection: abscess, bacterial infection, cellulitis, folliculitis, fungal infection, herpes simplex, herpes zoster, renal abscess, moniliasis, tonsillitis, viral infection;
Hematologic: anemia, epistaxis, leukopenia, lymphadenopathy;
Liver and Biliary System: bilirubinemia;
Metabolic and Nutritional: diabetes mellitus, hyperkalemia, hyperuricemia, hypoglycemia;
Musculoskeletal System: arthralgia, bone fracture, bursitis, joint dislocation, myalgia, stiffness, synovial cyst, tendon disorder;
Neoplasms: fibroadenosis, carcinoma;
Psychiatric: anxiety, confusion, decreased libido, emotional lability, impaired concentration, increased libido, nervousness, paroniria, somnolence;
Reproductive (Female): breast pain, uterine hemorrhage;
Respiratory System: abnormal chest sounds, bronchospasm;
Skin and Appendages: abnormal pigmentation, angioedema, dermatitis, dry skin, eczema, nail disorder, pruritus, skin disorder, urticaria;
Special Senses: abnormal vision, cataract, conjunctivitis, deafness, eye pain, taste perversion, tinnitus, vestibular disorder;
Urinary System: abnormal urine, hematuria, increased BUN, micturition urgency, nocturia, polyuria, pyelonephritis, urinary incontinence.
*NOS = Not Otherwise Specified.
Psoriasis: The principal adverse reactions associated with the use of cyclosporine in patients with psoriasis are renal dysfunction, headache, hypertension, hypertriglyceridemia, hirsutism/hypertrichosis, paresthesia or hyperesthesia, influenza-like symptoms, nausea/vomiting, diarrhea, abdominal discomfort, lethargy, and musculoskeletal or joint pain.
In psoriasis patients treated in US controlled clinical studies within the recommended dose range, cyclosporine therapy was discontinued in 1.0% of the patients because of hypertension and in 5.4% of the patients because of increased creatinine. In the majority of cases, these changes were reversible after dose reduction or discontinuation of cyclosporine.
There has been one reported death associated with the use of cyclosporine in psoriasis. A 27-year-old male developed renal deterioration and was continued on cyclosporine. He had progressive renal failure leading to death.
Frequency and severity of serum creatinine increases with dose and duration of cyclosporine therapy. These elevations are likely to become more pronounced and may result in irreversible renal damage without dose reduction or discontinuation.
Adverse Events Occurring in 3% or More of Psoriasis Patients in Controlled Clinical Trials Body System *Preferred TermNeoral® (N=182) Sandimmune® (N=185) Infection or Potential Infection24.7% 24.3% Influenza-like Symptoms9.9% 8.1% Upper Respiratory Tract Infections7.7% 11.3% Cardiovascular System28.0% 25.4% Hypertension **27.5% 25.4% Urinary System24.2% 16.2% Increased Creatinine19.8% 15.7% Central and Peripheral Nervous System26.4% 20.5% Headache15.9% 14.0% Paresthesia7.1% 4.8% Musculoskeletal System13.2% 8.7% Arthralgia6.0% 1.1% Body As A Whole-General29.1% 22.2% Pain4.4% 3.2% Metabolic and Nutritional9.3% 9.7% Reproductive, Female8.5% (4 of 47 females) 11.5% (6 of 52 females) Resistance Mechanism18.7% 21.1% Skin and Appendages17.6% 15.1% Hypertrichosis6.6% 5.4% Respiratory System5.0% 6.5% Bronchospasm, coughing, dyspnea, rhinitis5.0% 4.9% Psychiatric5.0% 3.8% Gastrointestinal System19.8% 28.7% Abdominal pain2.7% 6.0% Diarrhea5.0% 5.9% Dyspepsia2.2% 3.2% Gum hyperplasia3.8% 6.0% Nausea5.5% 5.9% White cell and RES4.4% 2.7% *Total percentage of events within the system**Newly occurring hypertension = SBP>/=160 mm Hg and/or DBP>/=90 mm Hg
The following events occurred in 1% to less than 3% of psoriasis patients treated with cyclosporine:
Body as a Whole: fever, flushes, hot flushes; Cardiovascular: chest pain; Central and Peripheral Nervous System: appetite increased, insomnia, dizziness, nervousness, vertigo; Gastrointestinal: abdominal distention, constipation, gingival bleeding; Liver and Biliary System: hyperbilirubinemia; Neoplasms: skin malignancies [squamous cell (0.9%) and basal cell (0.4%) carcinomas]; Reticuloendothelial: platelet, bleeding, and clotting disorders, red blood cell disorder; Respiratory: infection, viral and other infection; Skin and Appendages: acne, folliculitis, keratosis, pruritus, rash, dry skin; Urinary System: micturition frequency; Vision: abnormal vision.
Mild hypomagnesemia and hyperkalemia may occur but are asymptomatic. Increases in uric acid may occur and attacks of gout have been rarely reported. A minor and dose related hyperbilirubinemia has been observed in the absence of hepatocellular damage. Cyclosporine therapy may be associated with a modest increase of serum triglycerides or cholesterol. Elevations of triglycerides (>750 mg/dL) occur in about 15% of psoriasis patients; elevations of cholesterol (>300 mg/dL) are observed in less than 3% of psoriasis patients. Generally these laboratory abnormalities are reversible upon dose reduction or discontinuation of cyclosporine.
OVERDOSAGE
There is a minimal experience with cyclosporine overdosage. Forced emesis can be of value up to 2 hours after administration of Neoral®. Transient hepatotoxicity and nephrotoxicity may occur which should resolve following drug withdrawal. General supportive measures and symptomatic treatment should be followed in all cases of overdosage. Cyclosporine is not dialyzable to any great extent, nor is it cleared well by charcoal hemoperfusion. The oral dosage at which half of experimental animals are estimated to die is 31 times, 39 times, and >54 times the human maintenance dose for transplant patients (6 mg/kg; corrections based on body surface area) in mice, rats, and rabbits.
DOSAGE AND ADMINISTRATION
Neoral® Soft Gelatin Capsules (cyclosporine capsules, USP) MODIFIED and Neoral® Oral Solution (cyclosporine oral solution, USP) MODIFIED
Neoral® has increased bioavailability in comparison to Sandimmune®. Neoral® and Sandimmune® are not bioequivalent and cannot be used interchangeably without physician supervision.
The daily dose of Neoral® should always be given in two divided doses (BID). It is recommended that Neoral® be administered on a consistent schedule with regard to time of day and relation to meals. Grapefruit and grapefruit juice affect metabolism, increasing blood concentration of cyclosporine, thus should be avoided.
Newly Transplanted Patients: The initial oral dose of Neoral® can be given 4-12 hours prior to transplantation or be given postoperatively. The initial dose of Neoral® varies depending on the transplanted organ and the other immunosuppressive agents included in the immunosuppressive protocol. In newly transplanted patients, the initial oral dose of Neoral® is the same as the initial oral dose of Sandimmune®. Suggested initial doses are available from the results of a 1994 survey of the use of Sandimmune® in US transplant centers. The mean ± SD initial doses were 9±3 mg/kg/day for renal transplant patients (75 centers), 8±4 mg/kg/day for liver transplant patients (30 centers), and 7±3 mg/kg/day for heart transplant patients (24 centers). Total daily doses were divided into two equal daily doses. The Neoral® dose is subsequently adjusted to achieve a pre-defined cyclosporine blood concentration. (See Blood Concentration Monitoring in Transplant Patients , below) If cyclosporine trough blood concentrations are used, the target range is the same for Neoral® as for Sandimmune®. Using the same trough concentration target range for Neoral® as for Sandimmune® results in greater cyclosporine exposure when Neoral® is administered. (See Pharmacokinetics , Absorption ) Dosing should be titrated based on clinical assessments of rejection and tolerability. Lower Neoral® doses may be sufficient as maintenance therapy.
Adjunct therapy with adrenal corticosteroids is recommended initially. Different tapering dosage schedules of prednisone appear to achieve similar results. A representative dosage schedule based on the patient's weight started with 2.0 mg/kg/day for the first 4 days tapered to 1.0 mg/kg/day by 1 week, 0.6 mg/kg/day by 2 weeks, 0.3 mg/kg/day by 1 month, and 0.15 mg/kg/day by 2 months and thereafter as a maintenance dose. Steroid doses may be further tapered on an individualized basis depending on status of patient and function of graft. Adjustments in dosage of prednisone must be made according to the clinical situation.
Conversion from Sandimmune® to Neoral® in Transplant Patients: In transplanted patients who are considered for conversion to Neoral® from Sandimmune®, Neoral® should be started with the same daily dose as was previously used with Sandimmune® (1:1 dose conversion). The Neoral® dose should subsequently be adjusted to attain the pre-conversion cyclosporine blood trough concentration. Using the same trough concentration target range for Neoral® as for Sandimmune® results in greater cyclosporine exposure when Neoral® is administered. (See Pharmacokinetics , Absorption ) Patients with suspected poor absorption of Sandimmune® require different dosing strategies. (See Transplant Patients with Poor Absorption of Sandimmune® , below) In some patients, the increase in blood trough concentration is more pronounced and may be of clinical significance.
Until the blood trough concentration attains the pre-conversion value, it is strongly recommended that the cyclosporine blood trough concentration be monitored every 4 to 7 days after conversion to Neoral®. In addition, clinical safety parameters such as serum creatinine and blood pressure should be monitored every two weeks during the first two months after conversion. If the blood trough concentrations are outside the desired range and/or if the clinical safety parameters worsen, the dosage of Neoral® must be adjusted accordingly.
Transplant Patients with Poor Absorption of Sandimmune®: Patients with lower than expected cyclosporine blood trough concentrations in relation to the oral dose of Sandimmune® may have poor or inconsistent absorption of cyclosporine from Sandimmune®. After conversion to Neoral®, patients tend to have higher cyclosporine concentrations. Due to the increase in bioavailability of cyclosporine following conversion to Neoral®, the cyclosporine blood trough concentration may exceed the target range. Particular caution should be exercised when converting patients to Neoral® at doses greater than 10 mg/kg/day. The dose of Neoral® should be titrated individually based on cyclosporine trough concentrations, tolerability, and clinical response. In this population the cyclosporine blood trough concentration should be measured more frequently, at least twice a week (daily, if initial dose exceeds 10 mg/kg/day) until the concentration stabilizes within the desired range.
Rheumatoid Arthritis: The initial dose of Neoral® is 2.5 mg/kg/day, taken twice daily as a divided (BID) oral dose. Salicylates, nonsteroidal anti-inflammatory agents, and oral corticosteroids may be continued. (See WARNINGS and PRECAUTIONS , Drug Interactions ) Onset of action generally occurs between 4 and 8 weeks. If insufficient clinical benefit is seen and tolerability is good (including serum creatinine less than 30% above baseline), the dose may be increased by 0.5-0.75 mg/kg/day after 8 weeks and again after 12 weeks to a maximum of 4 mg/kg/day. If no benefit is seen by 16 weeks of therapy, Neoral® therapy should be discontinued.
Dose decreases by 25%-50% should be made at any time to control adverse events, e.g., hypertension elevations in serum creatinine (30% above patient's pretreatment level) or clinically significant laboratory abnormalities. (See WARNINGS and PRECAUTIONS )
If dose reduction is not effective in controlling abnormalities or if the adverse event or abnormality is severe, Neoral® should be discontinued. The same initial dose and dosage range should be used if Neoral® is combined with the recommended dose of methotrexate. Most patients can be treated with Neoral® doses of 3 mg/kg/day or below when combined with methotrexate doses of up to 15 mg/week. (See CLINICAL PHARMACOLOGY , Clinical Trials )
There is limited long-term treatment data. Recurrence of rheumatoid arthritis disease activity is generally apparent within 4 weeks after stopping cyclosporine.
Psoriasis: The initial dose of Neoral® should be 2.5 mg/kg/day. Neoral® should be taken twice daily, as a divided (1.25 mg/kg BID) oral dose. Patients should be kept at that dose for at least 4 weeks, barring adverse events. If significant clinical improvement has not occurred in patients by that time, the patient's dosage should be increased at 2-week intervals. Based on patient response, dose increases of approximately 0.5 mg/kg/day should be made to a maximum of 4.0 mg/kg/day.
Dose decreases by 25%-50% should be made at any time to control adverse events, e.g., hypertension, elevations in serum creatinine (>/=25% above the patient's pretreatment level), or clinically significant laboratory abnormalities. If dose reduction is not effective in controlling abnormalities, or if the adverse event or abnormality is severe, Neoral® should be discontinued. (See Special Monitoring of Psoriasis Patients )
Patients generally show some improvement in the clinical manifestations of psoriasis in 2 weeks. Satisfactory control and stabilization of the disease may take 12-16 weeks to achieve. Results of a dose-titration clinical trial with Neoral® indicate that an improvement of psoriasis by 75% or more (based on PASI) was achieved in 51% of the patients after 8 weeks and in 79% of the patients after 16 weeks. Treatment should be discontinued if satisfactory response cannot be achieved after 6 weeks at 4 mg/kg/day or the patient's maximum tolerated dose. Once a patient is adequately controlled and appears stable the dose of Neoral® should be lowered, and the patient treated with the lowest dose that maintains an adequate response (this should not necessarily be total clearing of the patient). In clinical trials, cyclosporine doses at the lower end of the recommended dosage range were effective in maintaining a satisfactory response in 60% of the patients. Doses below 2.5 mg/kg/day may also be equally effective.
Upon stopping treatment with cyclosporine, relapse will occur in approximately 6 weeks (50% of the patients) to 16 weeks (75% of the patients). In the majority of patients rebound does not occur after cessation of treatment with cyclosporine. Thirteen cases of transformation of chronic plaque psoriasis to more severe forms of psoriasis have been reported. There were 9 cases of pustular and 4 cases of erythrodermic psoriasis. Long term experience with Neoral® in psoriasis patients is limited and continuous treatment for extended periods greater than one year is not recommended. Alternation with other forms of treatment should be considered in the long term management of patients with this life long disease.
Neoral® Oral Solution (cyclosporine oral solution, USP) MODIFIED-Recommendations for Administration:
To make Neoral® Oral Solution (cyclosporine oral solution, USP) MODIFIED more palatable, it should be diluted with orange or apple juice that is at room temperature. Patients should avoid switching diluents frequently. Grapefruit juice affects metabolism of cyclosporine and should be avoided. The combination of Neoral® solution with milk can be unpalatable. The effect of milk on the bioavailability of cyclosorine when adminstered as Neoral® Oral Solution has not been evaluated.
Take the prescribed amount of Neoral® Oral Solution (cyclosporine oral solution, USP) MODIFIED from the container using the dosing syringe supplied, after removal of the protective cover, and transfer the solution to a glass of orange or apple juice. Stir well and drink at once. Do not allow diluted oral solution to stand before drinking. Use a glass container (not plastic). Rinse the glass with more diluent to ensure that the total dose is consumed. After use, dry the outside of the dosing syringe with a clean towel and replace the protective cover. Do not rinse the dosing syringe with water or other cleaning agents. If the syringe requires cleaning, it must be completely dry before resuming use.
Blood Concentration Monitoring in Transplant Patients: Transplant centers have found blood concentration of cyclosporine to be an essential component of patient management. Of importance to blood concentration analysis are the type of assay used, the transplanted organ, and other immunosuppressant agents being administered. While no fixed relationship has been established, blood concentration monitoring may assist in the clinical evaluation of rejection and toxicity, dose adjustments, and the assessment of compliance.
Various assays have been used to measure blood concentrations of cyclosporine. Older studies using a nonspecific assay often cited concentrations that were roughly twice those of the specific assays. Therefore, comparison between concentrations in the published literature and an individual patient concentration using current assays must be made with detailed knowledge of the assay methods employed. Current assay results are also not interchangeable and their use should be guided by their approved labeling. A discussion of the different assay methods is contained in Annals of Clinical Biochemistry 1994;31:420-446. While several assays and assay matrices are available, there is a consensus that parent-compound-specific assays correlate best with clinical events. Of these, HPLC is the standard reference, but the monoclonal antibody RIAs and the monoclonal antibody FPIA offer sensitivity, reproducibility, and convenience. Most clinicians base their monitoring on trough cyclosporine concentrations. Applied Pharmacokinetics, Principles of Therapeutic Drug Monitoring (1992) contains a broad discussion of cyclosporine pharmacokinetics and drug monitoring techniques. Blood concentration monitoring is not a replacement for renal function monitoring or tissue biopsies.
HOW SUPPLIED
Neoral® Soft Gelatin Capsules (cyclosporine capsules, USP) MODIFIED
25 mg
Oval, blue-gray imprinted in red, "Neoral" over "25 mg."
Packages of 30 unit-dose blisters (NDC 0078-0246-15).
100 mg
Oblong, blue-gray imprinted in red, "Neoral" over "100 mg."
Packages of 30 unit-dose blisters (NDC 0078-0248-15).
Store and Dispense: In the original unit-dose container at controlled room temperature 68°-77°F (20°-25°C).
Neoral® Oral Solution (cyclosporine oral solution, USP) MODIFIED: A clear, yellow liquid supplied in 50 mL bottles containing 100 mg/mL (NDC 0078-0274-22).
Store and Dispense: In the original container at controlled room temperature 68°-77°F (20°-25°C). Do not store in the refrigerator. Once opened, the contents must be used within two months. At temperatures below 68°F (20°C) the solution may gel; light flocculation or the formation of a light sediment may also occur. There is no impact on product performance or dosing using the syringe provided. Allow to warm to room temperature 77°F (25°C) to reverse these changes.
Neoral® Soft Gelatin Capsules (cyclosporine capsules, USP) MODIFIED
Manufactured by R.P. Scherer GmbH, EBERBACH/BADEN, GERMANY
Manufactured for Novartis Pharmaceuticals Corporation, East Hanover, NJ 07936
Neoral® Oral Solution (cyclosporine oral solution, USP) MODIFIED
Manufactured by Novartis Pharma S.A.S, F-68330 Huningue, France
Manufactured for Novartis Pharmaceuticals Corporation, East Hanover, NJ 07936
Distributed by:
Novartis Pharmaceuticals Corporation
East Hanover, New Jersey 07936
T2004-19REV: MARCH 2004 PRINTED IN USA 89005007©Novartis
Subscribe to the "News" RSS Feed 
TOP ۞
