-
Novolin 70/30 InnoLet, Novolin N InnoLet, Novolin R InnoLet (Novo Nordisk)
Novolin® InnoLet®
Novolin® InnoLet® directions for use
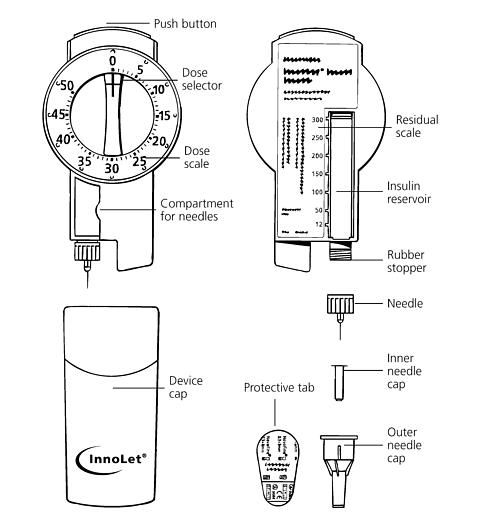
Novolin® InnoLet® is a disposable dial-a-dose insulin delivery system able to deliver 1-50 units in increments of 1 unit. Novolin InnoLet is designed for use with NovoFine® single-use needles or other products specifically recommended by Novo Nordisk®. Novolin InnoLet is not recommended for the blind or severely visually impaired patients without the assistance of a sighted individual trained in the proper use of this product.
Please read these instructions completely before using this device.
-
Preparing the Novolin® InnoLet®:
Pull off the device cap.
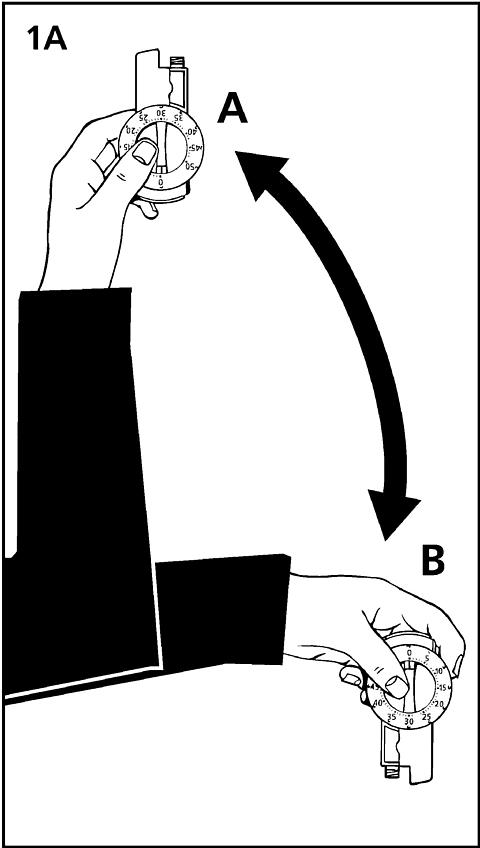
1A. Turn the Novolin InnoLet up and down between positions A and B so the glass ball is moved from one end of the insulin reservoir to the other. Do this at least 10 times, until the liquid appears uniformly white and cloudy.
To ensure even mixing of the remaining insulin there must be at least 12 units of insulin left in the reservoir. If there are less than 12 units left, do not use the Novolin InnoLet. This step is not necessary for Novolin R InnoLet.
Wipe rubber stopper with an alcohol swab.
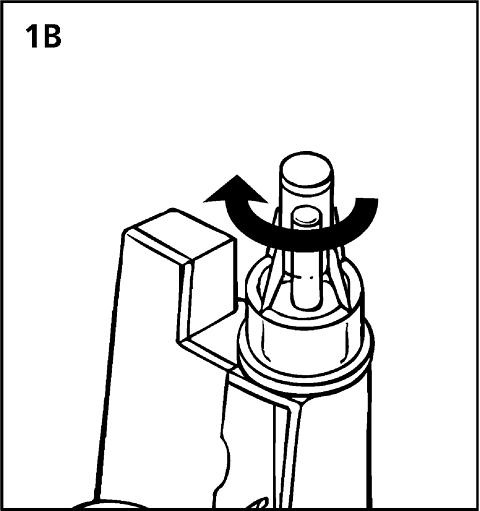
1B. Remove the protective tab from the disposable needle and screw the needle onto the Novolin InnoLet. Never place a disposable needle on your Novolin InnoLet until you are ready to give an injection. Remove the needle immediately after use. If the needle is not removed, some liquid may be expelled from the Novolin InnoLet causing a change in insulin concentration (strength) for Novolin 70/30 InnoLet and Novolin N InnoLet.
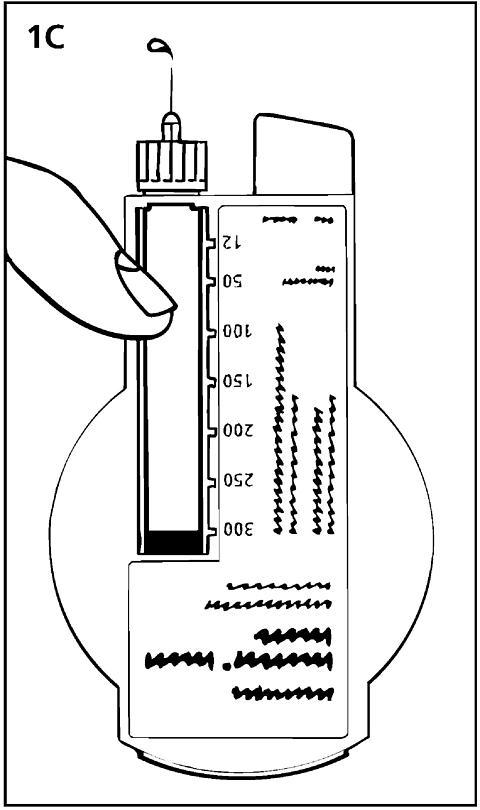
1C. Giving the air shot prior to each injection:
Small amounts of air may collect in the needle and insulin reservoir during normal use. To avoid the injection of air and ensure proper dosing, dial 2 units by turning the dose selector clockwise. Hold the Novolin InnoLet with the needle up and tap the Novolin InnoLet gently with your finger so any air bubbles collect in the top of the reservoir. Remove both the plastic outer and inner needle caps.
With the needle pointing up, press the push button as far as it will go and the dose selector returns to zero. See if a drop of insulin appears at the needle tip (see fig. 1C). If not, repeat the procedure until insulin appears. Before the first use of Novolin InnoLet you may need to perform up to 6 air shots to get a drop of insulin at the needle tip. If you need to make more than 6 air shots, do not use, and return the product to Novo Nordisk. A small air bubble may remain but it will not be injected because the operating mechanism prevents the reservoir from being completely emptied.
-
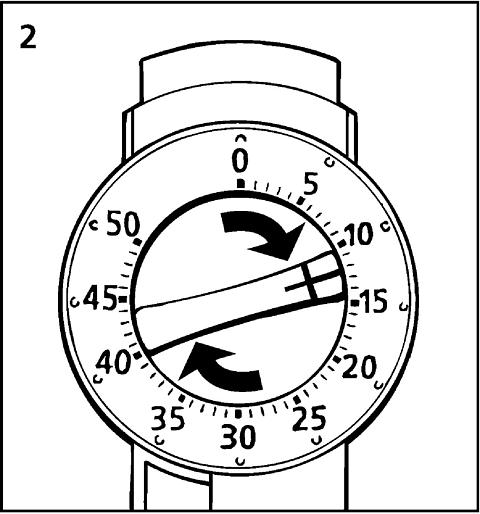
Setting the dose
Always check that the push button is fully depressed and the dose selector is set to zero. Hold the Novolin InnoLet in front of you and dial the dose selector clockwise to set the required dose. Do not put your hand over the push button when dialing the dose. If the button is not allowed to rise freely, insulin will be pushed out of the needle. When setting your dose, you will hear a click for every single unit dialed. Do not rely on this clicking sound as a means of determining your dose. If you have set a wrong dose, simply dial the dose selector forward or backwards until the right number of units has been set.
50 units is the maximum dose.
-
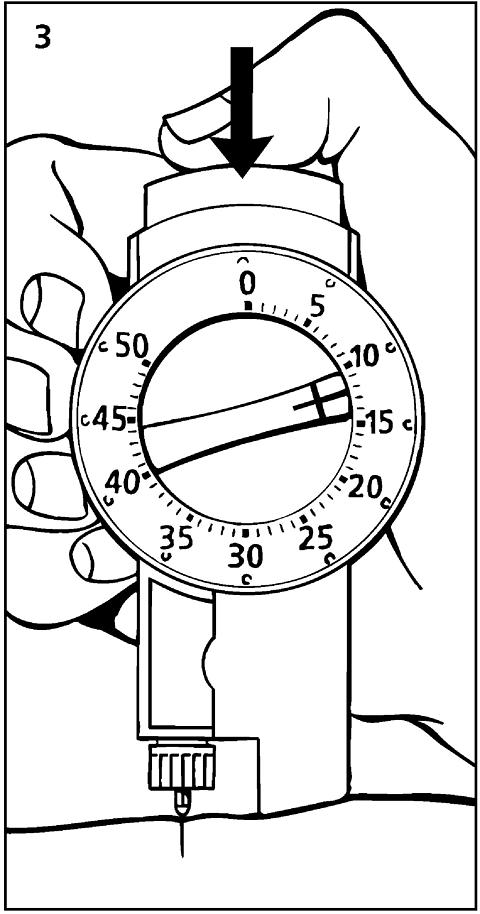
Giving the injection
Use the injection technique recommended by your doctor. Check that you have set the proper dose and depress the push button as far as it will go. Make sure not to block the dose selector while injecting as the dose selector must be allowed to return to zero when you press the push button. When depressing the push button you may hear a clicking sound. Do not rely on this clicking sound as a means of confirming delivery of your dose.
After making the injection, unscrew the needle and discard appropriately. Replace the device cap. Health care professionals, relatives, and other care-givers should follow general precautionary measures for removal and disposal of needles to eliminate the risk of unintended needle penetration.
For additional information see Giving the injection in the drug section of this insert.
Subsequent injections
Always check that the push button is fully depressed before using the Novolin InnoLet again. If not, turn the dose selector until the push button is completely down. Then proceed as stated under steps 1-3. The numbers on the insulin reservoir can be used to estimate the amount of insulin left in the Novolin InnoLet. These numbers are not used for measuring the insulin dose.
You cannot set a dose greater than the number of units remaining in the reservoir.
-
Function check
If you think that your Novolin InnoLet is not working properly, follow this procedure:
- Screw on a new NovoFine needle.
- Perform air shot as described in section 1C.
- Put the outer needle cap onto the needle.
- Dispense 20 units into the needle cap.
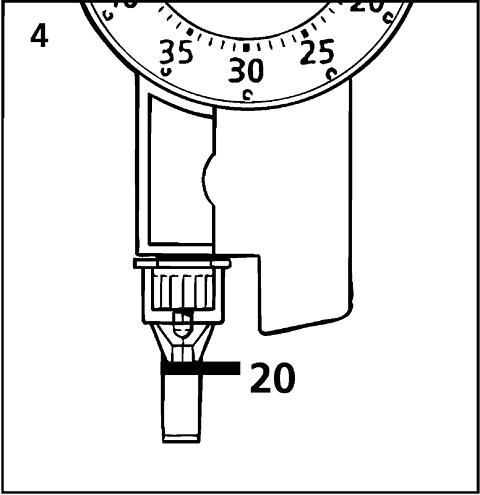
The insulin will fill the lower part of the cap (as shown in fig. 4). If the Novolin InnoLet has released too much or too little insulin, repeat the test. If it happens again, contact Novo Nordisk and do not use your Novolin InnoLet. -
Important notes
- If you need to perform more than 6 air shots before the first use of Novolin InnoLet to get a drop of insulin at the needle tip, do not use.
- Remember to perform an air shot before each injection (see fig. 1C).
- Care should be taken not to drop the Novolin InnoLet or subject it to impact.
- Remember to keep the Novolin InnoLet that you are currently using with you; don't leave it in a car or other location where extremes of temperature can occur.
- Novolin InnoLet is designed for use with NovoFine disposable needles or other products specifically recommended by Novo Nordisk.
- Never place a disposable needle on the Novolin InnoLet until you are ready to use it. Remove the needle immediately after use.
- Discard the used Novolin InnoLet carefully, without the needle attached.
- Always carry a spare Novolin InnoLet with you in case your Novolin InnoLet is damaged or lost.
- Novo Nordisk cannot be held responsible for adverse reactions occurring as a consequence of using the insulin delivery system with products that are not recommended by Novo Nordisk.
- Keep Novolin InnoLet out of the reach of children.
© 2003 Novo Nordisk A/S
Call 800-727-6500 for additional information.
Novo Nordisk Pharmaceuticals, Inc.
Princeton, NJ 08540
Manufactured by
Novo Nordisk A/S
DK-2880 Bagsvaerd, Denmark
www.novonordisk-us.com
Novo Nordisk®, Novolin®,
Lente®, NovoFine® and InnoLet®
are trademarks owned by
Novo Nordisk A / S
U.S. Patents Nos. 5,947,934, 6,074,372, 6,110,149, 6,302,869, 5,462,535, 5,599,323, 5,951,530, 5,968,021, 5,971,966, 5,980,491, 5,984,906, and other U.S. patents pending.
Restricted to use with Novo Nordisk pen needles.
Insulin information for the patient
Novolin® 70/30 InnoLet®
70% NPH, Human Insulin Isophane Suspension and 30% Regular, Human Insulin Injection (recombinant DNA origin) is a 3 mL disposable prefilled insulin syringe
100 units/mL (U-100)
Novolin® N InnoLet®
NPH, Human Insulin Isophane Suspension (recombinant DNA origin) is a 3 mL disposable prefilled insulin syringe
100 units/mL (U-100)
Novolin® R InnoLet®
Regular, Human Insulin Injection (recombinant DNA origin) USP is a 3mL disposable prefilled insulin syringe
100 units/mL (U-100)
Please read both sides of this insert carefully before using this product.
Novolin® InnoLet® is for single-person use only.
See Important notes section.
WARNINGANY CHANGE OF INSULIN SHOULD BE MADE CAUTIOUSLY AND ONLY UNDER MEDICAL SUPERVISION. CHANGES IN PURITY, STRENGTH, BRAND (MANUFACTURER), TYPE (REGULAR, NPH, LENTE®, ETC.), SPECIES (BEEF, PORK, BEEF-PORK, HUMAN), AND/OR METHOD OF MANUFACTURE (RECOMBINANT DNA VERSUS ANIMAL-SOURCE INSULIN) MAY RESULT IN THE NEED FOR A CHANGE IN DOSAGE.
SPECIAL CARE SHOULD BE TAKEN WHEN THE TRANSFER IS FROM A STANDARD BEEF OR MIXED SPECIES INSULIN TO A PURIFIED PORK OR HUMAN INSULIN. IF A DOSAGE ADJUSTMENT IS NEEDED, IT WILL USUALLY BECOME APPARENT EITHER IN THE FIRST FEW DAYS OR OVER A PERIOD OF SEVERAL WEEKS. ANY CHANGE IN TREATMENT SHOULD BE CAREFULLY MONITORED.
PLEASE READ THE SECTIONS " INSULIN REACTION AND SHOCK " AND " DIABETIC KETOACIDOSIS AND COMA " FOR SYMPTOMS OF HYPOGLYCEMIA (LOW BLOOD GLUCOSE) AND HYPERGLYCEMIA (HIGH BLOOD GLUCOSE).
Insulin use in diabetes
Your physician has explained that you have diabetes and that your treatment involves injections of insulin or insulin therapy combined with an oral antidiabetic medicine. Insulin is normally produced by the pancreas, a gland that lies behind the stomach. Without insulin, glucose (a simple sugar made from digested food) is trapped in the bloodstream and cannot enter the cells of the body. Some patients who don't make enough of their own insulin, or who cannot use the insulin they do make properly, must take insulin by injection in order to control their blood glucose levels. Each case of diabetes is different and requires direct and continued medical supervision.
Your physician has told you the type, strength and amount of insulin you should use and the time(s) at which you should inject it, and has also discussed with you a diet and exercise schedule. You should contact your physician if you experience any difficulties or if you have questions.
Types of insulins
Standard and purified animal insulins as well as human insulins are available. Standard and purified insulins differ in their degree of purification and content of noninsulin material. Standard and purified insulins also vary in species source; they may be of beef, pork, or mixed beef and pork origin. Human insulin is identical in structure to the insulin produced by the human pancreas, and thus differs from animal insulins. Insulins vary in time of action; see Product description for additional information.
Your physician has prescribed the insulin that is right for you; be sure you have purchased the correct insulin and check it carefully before you use it.
Product description
A package contains five (5) Novolin® InnoLet®. Novolin human insulin (recombinant DNA origin) is structurally identical to the insulin produced by the human pancreas. This human insulin is produced by recombinant DNA technology utilizing Saccharomyces cerevisiae (bakers' yeast) as the production organism.
Novolin 70/30 InnoLet contains a mixture of 70% NPH, Human Insulin Isophane Suspension and 30% Regular, Human Insulin Injection (recombinant DNA origin). The concentration of this product is 100 units of insulin per milliliter. It is a cloudy or milky suspension of human insulin with protamine and zinc. The insulin substance (the cloudy material) settles at the bottom of the insulin reservoir, therefore, the Novolin 70/30 InnoLet must be rotated up and down so that the contents are uniformly mixed before a dose is given. Novolin 70/30 InnoLet has an intermediate duration of action. The effect of Novolin 70/30 InnoLet begins approximately 1/2 hour after injection. The effect is maximal between 2 and approximately 12 hours. The full duration of action may last up to 24 hours after injection.
Novolin N InnoLet contains Novolin N , commonly known as NPH, Human Insulin Isophane Suspension (recombinant DNA origin). The concentration of this product is 100 units of insulin per milliliter. It is a cloudy or milky suspension of human insulin with protamine and zinc. The insulin substance (the cloudy material) settles at the bottom of the insulin reservoir, therefore, the Novolin N InnoLet must be rotated up and down so that the contents are uniformly mixed before a dose is given. Novolin N has an intermediate duration of action. The effect of Novolin N begins approximately 1 ½ hour after injection. The effect is maximal between 4 and 12 hours. The full duration of action may last up to 24 hours after injection.
Novolin R InnoLet contains Novolin R , commonly known as Regular, Human Insulin Injection (recombinant DNA origin) USP. The concentration of this product is 100 units of insulin per milliliter. It is a clear, colorless solution which has a short duration of action. The effect of Novolin R begins approximately ½ hour after injection. The effect is maximal between 2 ½ and 5 hours and ends approximately 8 hours after injection.
The time course of action of any insulin may vary considerably in different individuals, or at different times in the same individual. Because of this variation, the time periods listed here should be considered as general guidance only.
Storage
Novolin InnoLet should be stored in a cold (36°-46°F [2°-8°C]) place, preferably in a refrigerator, but not in the freezing compartment. Do not let it freeze . Keep Novolin InnoLet in the carton so that it will stay clean and protected from light. The Novolin InnoLet that you are currently using should not be refrigerated but should be kept as cool as possible (below 86°F [30°C]) and away from direct heat and light. Unrefrigerated Novolin 70/30 InnoLet must be discarded after 10 days even if they still contain Novolin 70/30 . Unrefrigerated Novolin N InnoLet must be discarded after 14 days, even if they still contain Novolin N . Unrefrigerated Novolin R InnoLet must be discarded after 28 days, even if they still contain Novolin R .
Never use Novolin InnoLet after the expiration date printed on the label and carton.
Never use any Novolin 70/30 InnoLet or Novolin N InnoLet if the precipitate (the white deposit) has become lumpy or granular in appearance or has formed a deposit of solid particles on the wall of the insulin reservoir. This insulin should not be used if the liquid in the insulin reservoir remains clear after it has been mixed. Never use any Novolin R InnoLet if the insulin in the device becomes viscous (thickened) or cloudy; use it only if it is clear and colorless.
Important
Failure to comply with the following antiseptic measures may lead to infections at the injection site.
- Disposable needles are for single use; they should be used only once and destroyed.
- Clean your hands and the injection site with soap and water or with alcohol.
- Wipe the rubber stopper on the insulin cartridge with an alcohol swab.
Preparing the injection
Never place a single-use disposable needle on your Novolin InnoLet until you are ready to give an injection, and remove the needle immediately after each injection. Follow the directions for use of the Novolin InnoLet in the device section of this insert.
Novolin InnoLet may contain a small amount of air. To prevent an injection of air and make certain insulin is delivered, an air shot must be done before each injection. Directions for performing an air shot are provided in the device section of this insert.
Giving the injection
- The following areas are suitable for subcutaneous insulin injection: thighs, upper arms, buttocks, abdomen. Do not change areas without consulting your physician. The actual point of injection should be changed each time; injection sites should be about an inch apart.
- The injection site should be clean and dry. Pinch up skin area to be injected and hold it firmly.
- Hold the device upright and push the needle quickly and firmly into the pinched-up area. Release the skin and push the push-button all the way in to inject insulin beneath the skin. After the injection, the needle should remain under the skin for at least 6 seconds. Keep the push button fully depressed until the needle is withdrawn from the skin. This will ensure that the full dose has been delivered.
- Do not inject into a muscle unless your physician has advised it. You should never inject insulin into a vein.
-
Remove the needle. If slight bleeding occurs, press lightly with a dry cotton swab for a few seconds -
do not rub
.
For additional information see Giving the injection in the device section of this insert.
Usage in pregnancy
It is particularly important to maintain good control of your diabetes during pregnancy and special attention must be paid to your diet, exercise and insulin regimens. If you are pregnant or nursing a baby, consult your physician or nurse educator.
Insulin reaction and shock
Insulin reaction (hypoglycemia) occurs when the blood glucose falls very low. This can happen if you take too much insulin, miss or delay a meal, exercise more than usual or work too hard without eating, or become ill (especially with vomiting or fever). Hypoglycemia can also happen if you combine insulin therapy and other medications that lower blood glucose, such as oral antidiabetic agents or other prescription and over-the-counter drugs. The first symptoms of an insulin reaction usually come on suddenly. They may include a cold sweat, fatigue, nervousness or shakiness, rapid heartbeat, or nausea. Personality change or confusion may also occur. If you drink or eat something right away (a glass of milk or orange juice, or several sugar candies), you can often stop the progression of symptoms. If symptoms persist, call your physician - an insulin reaction can lead to unconsciousness. If a reaction results in loss of consciousness, emergency medical care should be obtained immediately. If you have had repeated reactions or if an insulin reaction has led to a loss of consciousness, contact your physician. Severe hypoglycemia can result in temporary or permanent impairment of brain function and death.
In certain cases, the nature and intensity of the warning symptoms of hypoglycemia may change. A few patients have reported that after being transferred to human insulin, the early warning symptoms of hypoglycemia were less pronounced than they had been with animal-source insulin.
Diabetic ketoacidosis and coma
Diabetic ketoacidosis may develop if your body has too little insulin. The most common causes are acute illness or infection or failure to take enough insulin by injection. If you are ill you should check your urine for ketones. The symptoms of diabetic ketoacidosis usually come on gradually, over a period of hours or days, and include a drowsy feeling, flushed face, thirst and loss of appetite. Notify your physician right away if the urine test is positive for ketones (acetone) or if you have any of these symptoms. Fast, heavy breathing and rapid pulse are more severe symptoms and you should have medical attention right away. Severe, sustained hyperglycemia may result in diabetic coma and death.
ADVERSE REACTIONS
A few people with diabetes develop red, swollen and itchy skin where the insulin has been injected. This is called a "local reaction" and it may occur if the injection is not properly made, if the skin is sensitive to the cleansing solution, or if you are allergic to the insulin being used. If you have a local reaction, tell your physician.
Generalized insulin allergy occurs rarely, but when it does it may cause a serious reaction, including skin rash over the body, shortness of breath, fast pulse, sweating, and a drop in blood pressure. If any of these symptoms develop, you should seek emergency medical care.
If severe allergic reactions to insulin have occurred (i.e., generalized rash, swelling or breathing difficulties) you should be skin-tested with each new insulin preparation before it is used.
Important notes
- A change in the type, strength, species or purity of insulin could require a dosage adjustment. Any change in insulin should be made under medical supervision.
- To avoid possible transmission of disease, Novolin InnoLet is for single-person use only.
- You may have learned how to test your urine or your blood for glucose. It is important to do these tests regularly and to record the results for review with your physician or nurse educator.
- If you have an acute illness, especially with vomiting or fever, continue taking your insulin. If possible, stay on your regular diet. If you have trouble eating, drink fruit juices, regular soft drinks, or clear soups; if you can, eat small amounts of bland foods. Test your urine for glucose and ketones and, if possible, test your blood glucose. Note the results and contact your physician for possible insulin dose adjustment. If you have severe and prolonged vomiting, seek emergency medical care.
- You should always carry identification which states that you have diabetes.
- Always ask your physician or pharmacist before taking any drug.
Always consult your physician if you have any questions about your condition or the use of insulin.
Helpful information for people with diabetes is published by American Diabetes Association, 1660 Duke Street, Alexandria, VA 22314
Date of Issue: May 2003
© 2002/2003 Novo Nordisk A/S
Call 800-727-6500 for additional information.
Pharmaceuticals, Inc.
Princeton, NJ 08540
Manufactured by
Novo Nordisk A/S
DK-2880 Bagsvaerd, Denmark
www.novonordisk-us.com
Novo Nordisk®, Novolin®,
Lente®, NovoFine® and
InnoLet® are trademarks
owned by
Novo Nordisk A / S
-
Preparing the Novolin® InnoLet®:
Subscribe to the "News" RSS Feed 
TOP ۞
