-
Primaxin I.V. (Merck)
To reduce the development of drug-resistant bacteria and maintain the effectiveness of PRIMAXIN I.V. † and other antibacterial drugs, PRIMAXIN I.V. should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria.
For Intravenous Injection Only
DESCRIPTION
PRIMAXIN † I.V. (Imipenem and Cilastatin for Injection) is a sterile formulation of imipenem (a thienamycin antibiotic) and cilastatin sodium (the inhibitor of the renal dipeptidase, dehydropeptidase I), with sodium bicarbonate added as a buffer. PRIMAXIN I.V. is a potent broad spectrum antibacterial agent for intravenous administration.
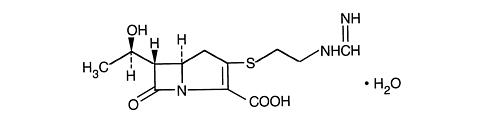
Imipenem (N-formimidoylthienamycin monohydrate) is a crystalline derivative of thienamycin, which is produced by Streptomyces cattleya. Its chemical name is (5 R ,6 S )-3-[[2-(formimidoylamino)ethyl]thio]-6-[( R )-1-hydroxyethyl ]-7-oxo-1-azabicyclo[3.2.0]hept-2-ene-2-carboxylic acid monohydrate. It is an off-white, nonhygroscopic crystalline compound with a molecular weight of 317.37. It is sparingly soluble in water and slightly soluble in methanol. Its empirical formula is C 12 H 17 N 3 O 4 S · H 2 O, and its structural formula is:
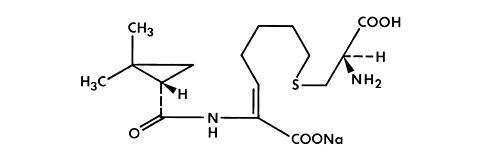
Cilastatin sodium is the sodium salt of a derivatized heptenoic acid. Its chemical name is sodium ( Z )-7-[[( R )-2-amino-2-carboxyethyl]thio] -2- [( S ) - 2,2- dimethylcyclopropanecarboxamido]-2-heptenoate. It is an off-white to yellowish-white, hygroscopic, amorphous compound with a molecular weight of 380.43. It is very soluble in water and in methanol. Its empirical formula is C 16 H 25 N 2 O 5 S Na, and its structural formula is:
PRIMAXIN I.V. is buffered to provide solutions in the pH range of 6.5 to 8.5. There is no significant change in pH when solutions are prepared and used as directed. (See COMPATIBILITY AND STABILITY .) PRIMAXIN I.V. 250 contains 18.8 mg of sodium (0.8 mEq) and PRIMAXIN I.V. 500 contains 37.5 mg of sodium (1.6 mEq). Solutions of PRIMAXIN I.V. range from colorless to yellow. Variations of color within this range do not affect the potency of the product.
† Registered trademark of Merck & CO., Inc.
CLINICAL PHARMACOLOGY
Adults
Intravenous Administration
Intravenous infusion of PRIMAXIN I.V. over 20 minutes results in peak plasma levels of imipenem antimicrobial activity that range from 14 to 24 µg/mL for the 250 mg dose, from 21 to 58 µg/mL for the 500 mg dose, and from 41 to 83 µg/mL for the 1000 mg dose. At these doses, plasma levels of imipenem antimicrobial activity decline to below 1 µg/mL or less in 4 to 6 hours. Peak plasma levels of cilastatin following a 20-minute intravenous infusion of PRIMAXIN I.V., range from 15 to 25 µg/mL for the 250 mg dose, from 31 to 49 µg/mL for the 500 mg dose, and from 56 to 88 µg/mL for the 1000 mg dose.
The plasma half-life of each component is approximately 1 hour. The binding of imipenem to human serum proteins is approximately 20% and that of cilastatin is approximately 40%. Approximately, 70% of the administered imipenem is recovered in the urine within 10 hours after which no further urinary excretion is detectable. Urine concentrations of imipenem in excess of 10 µg/mL can be maintained for up to 8 hours with PRIMAXIN I.V. at the 500-mg dose. Approximately, 70% of the cilastatin sodium dose is recovered in the urine within 10 hours of administration of PRIMAXIN I.V.
No accumulation of imipenem/cilastastin in plasma or urine is observed with regimens administered as frequently as every 6 hours in patients with normal renal function.
In healthy elderly volunteers (65 to 75 years of age with normal renal function for their age), the pharmacokinetics of a single dose of imipenem 500 mg and cilastatin 500 mg administered intravenously over 20 minutes are consistent with those expected in subjects with slight renal impairment for which no dosage alteration is considered necessary. The mean plasma half-lives of imipenem and cilastatin are 91 ± 7.0 minutes and 69 ± 15 minutes, respectively. Multiple dosing has no effect on the pharmacokinetics of either imipenem or cilastatin, and no accumulation of imipenem/cilastatin is observed.
Imipenem, when administered alone, is metabolized in the kidneys by dehydropeptidase I resulting in relatively low levels in urine. Cilastatin sodium, an inhibitor of this enzyme, effectively prevents renal metabolism of imipenem so that when imipenem and cilastatin sodium are given concomitantly, fully adequate antibacterial levels of imipenem are achieved in the urine.
After a 1 gram dose of PRIMAXIN I.V., the following average levels of imipenem were measured (usually at 1 hour post-dose except where indicated) in the tissues and fluids listed:
Tissue or Fluidn Imipenem Level
µg/mL or µg/gRange Vitreous Humor3 3.4 (3.5 hours post dose)2.88-3.6 Aqueous Humor5 2.99 (2 hours post dose)2.4-3.9 Lung Tissue8 5.6 (median)3.5-15.5 Sputum1 2.1-- Pleural1 22.0-- Peritoneal12 23.9 S.D. ±5.3 (2 hours post dose)-- Bile2 5.3 (2.25 hours post dose)4.6 to 6.0 CSF (uninflamed)5 1.0 (4 hours post dose)0.26-2.0 CSF (inflamed)7 2.6 (2 hours post dose)0.5-5.5 Fallopian Tubes1 13.6-- Endometrium1 11.1-- Myometrium1 5.0-- Bone10 2.60.4-5.4 Interstitial Fluid12 16.410.0-22.6 Skin12 4.4NA Fascia12 4.4NA
Imipenem-cilastatin sodium is hemodialyzable. However, usefulness of this procedure in the overdosage setting is questionable. (See OVERDOSAGE .)
Microbiology
The bactericidal activity of imipenem results from the inhibition of cell wall synthesis. Its greatest affinity is for penicillin binding proteins (PBPs) 1A, 1B, 2, 4, 5 and 6 of Escherichia coli, and 1A, 1B, 2, 4 and 5 of Pseudomonas aeruginosa. The lethal effect is related to binding to PBP 2 and PBP 1B.
Imipenem has a high degree of stability in the presence of beta-lactamases, both penicillinases and cephalosporinases produced by gram-negative and gram-positive bacteria. It is a potent inhibitor of beta-lactamases from certain gram-negative bacteria which are inherently resistant to most beta-lactam antibiotics, e.g., Pseudomonas aeruginosa, Serratia spp., and Enterobacter spp.
Imipenem has in vitro activity against a wide range of gram-positive and gram-negative organisms. Imipenem has been shown to be active against most strains of the following microorganisms, both in vitro and in clinical infections treated with the intravenous formulation of imipenem-cilastatin sodium as described in the INDICATIONS AND USAGE section.
Gram-positive aerobes:
Enterococcus faecalis (formerly S. faecalis )
(NOTE: Imipenem is inactive in vitro against Enterococcus faecium [formerly S. faecium ].)
Staphylococcus aureus including penicillinase-producing strains
Staphylococcus epidermidis including penicillinase-producing strains
(NOTE: Methicillin-resistant staphylococci should be reported as resistant to imipenem.)
Streptococcus agalactiae (Group B streptococci)
Streptococcus pneumoniae
Streptococcus pyogenes
Gram-negative aerobes:
Acinetobacter spp.
Citrobacter spp.
Enterobacter spp.
Escherichia coli
Gardnerella vaginalis
Haemophilus influenzae
Haemophilus parainfluenzae
Klebsiella spp.
Morganella morganii
Proteus vulgaris
Providencia rettgeri
Pseudomonas aeruginosa
(NOTE: Imipenem is inactive in vitro against Xanthomonas (Pseudomonas) maltophilia and some strains of P. cepacia. )
Serratia spp., including S. marcescens
Gram-positive anaerobes:
Bifidobacterium spp.
Clostridium spp.
Eubacterium spp.
Peptococcus spp.
Peptostreptococcus spp.
Propionibacterium spp.
Gram-negative anaerobes:
Bacteroides spp., including B. fragilis
Fusobacterium spp.
The following in vitro data are available, but their clinical significance is unknown.
Imipenem exhibits in vitro minimum inhibitory concentrations (MICs) of 4 µg/mL or less against most (>/=90%) strains of the following microorganisms; however, the safety and effectiveness of imipenem in treating clinical infections due to these microorganisms have not been established in adequate and well-controlled clinical trials.
Gram-positive aerobes:
Bacillus spp.
Listeria monocytogenes
Nocardia spp.
Staphylococcus saprophyticus
Group C streptococci
Group G streptococci
Viridans group streptococci
Gram-negative aerobes:
Aeromonas hydrophila
Alcaligenes spp.
Capnocytophaga spp.
Haemophilus ducreyi
Neisseria gonorrhoeae including penicillinase-producing strains
Pasteurella spp.
Providencia stuartii
Gram-negative anaerobes:
Prevotella bivia
Prevotella disiens
Prevotella melaninogenica
Veillonella spp.
In vitro tests show imipenem to act synergistically with aminoglycoside antibiotics against some isolates of Pseudomonas aeruginosa.
Susceptibility Tests:
Measurement of MIC or minimum bactericidal concentration (MBC) and achieved antimicrobial compound concentrations may be appropriate to guide therapy in some infections. (See CLINICAL PHARMACOLOGY section for further information on drug concentrations achieved in infected body sites and other pharmacokinetic properties of this antimicrobial drug product.)
Dilution Techniques:
Quantitative methods that are used to determine MICs provide reproducible estimates of the susceptibility of bacteria to antimicrobial compounds. One such procedure uses a standardized dilution method 1 (broth, agar, or microdilution) or equivalent with imipenem powder.
The MIC values obtained should be interpreted according to the following criteria:
MIC (µg/mL) Interpretation</=4 Susceptible (S)8 Intermediate (I)>/=16 Resistant (R)
A report of "Susceptible" indicates that the pathogen is likely to be inhibited by usually achievable concentrations of the antimicrobial compound in blood. A report of "Intermediate" indicates that the result should be considered equivocal, and, if the microorganism is not fully susceptible to alternative, clinically feasible drugs, the test should be repeated. This category implies possible clinical applicability in body sites where the drug is physiologically concentrated or in situations where high dosage of drug can be used. This category also provides a buffer zone that prevents small uncontrolled technical factors from causing major discrepancies in interpretation. A report of "Resistant" indicates that usually achievable concentrations of the antimicrobial compound in the blood are unlikely to be inhibitory and that other therapy should be selected.
Standardized susceptibility test procedures require the use of laboratory control microorganisms. Standard imipenem powder should provide the following MIC values:
Microorganism MIC (µg/mL)E. coli ATCC 259220.06-0.25S. aureus ATCC 292130.015-0.06E. faecalis ATCC 292120.5-2.0P. aeruginosa ATCC 278531.0-4.0
Diffusion Techniques:
Quantitative methods that require measurement of zone diameters provide reproducible estimates of the susceptibility of bacteria to antimicrobial compounds. One such standardized procedure 2 that has been recommended for use with disks to test the susceptibility of microorganisms to imipenem uses the 10-µg imipenem disk. Interpretation involves correlation of the diameter obtained in the disk test with the MIC for imipenem.
Reports from the laboratory providing results of the standard single-disk susceptibility test with a 10-µg imipenem disk should be interpreted according to the following criteria:
Zone Diameter (mm) Interpretation >/=16 Susceptible (S) 14-15 Intermediate (I) </=13 Resistant (R)
Interpretation should be as stated above for results using dilution techniques.
Standardized susceptibility test procedures require the use of laboratory control microorganisms. The 10-µg imipenem disk should provide the following diameters in these laboratory test quality control strains:
Microorganism Zone Diameter (mm) E. coli ATCC 2592226-32 P. aeruginosa ATCC 2785320-28
Anaerobic techniques:
For anaerobic bacteria, the susceptibility to imipenem can be determined by the reference agar dilution method or by alternate standardized test methods. 3
The MIC values obtained should be interpreted according to the following criteria:
MIC (µg/mL) Interpretation</=4 Susceptible (S)8 Intermediate (I)>/=16 Resistant (R)
As with other susceptibility techniques, the use of laboratory control microorganisms is required. Standard imipenem powder should provide the following MIC values:
Reference Agar Dilution Testing:
MicroorganismMIC (µg/mL) B. fragilis ATCC 252850.03-0.12 B. thetaiotaomicron ATCC 297410.06-0.25 E. lentum ATCC 430550.25-1.0
Broth Microdilution Testing:
MicroorganismMIC (µg/mL) B. thetaiotaomicron ATCC 297410.06-0.25 E. lentum ATCC 430550.12-0.5
INDICATIONS AND USAGE
PRIMAXIN I.V. is indicated for the treatment of serious infections caused by susceptible strains of the designated microorganisms in the conditions listed below:
- Lower respiratory tract infections. Staphylococcus aureus (penicillinase-producing strains), Acinetobacter species, Enterobacter species, Escherichia coli, Haemophilus influenzae, Haemophilus parainfluenzae * , Klebsiella species, Serratia marcescens
- Urinary tract infections (complicated and uncomplicated). Enterococcus faecalis, Staphylococcus aureus (penicillinase-producing strains) * , Enterobacter species, Escherichia coli, Klebsiella species, Morganella morganii * , Proteus vulgaris * , Providencia rettgeri * , Pseudomonas aeruginosa
- Intra-abdominal infections. Enterococcus faecalis, Staphylococcus aureus (penicillinase-producing strains) * , Staphylococcus epidermidis, Citrobacter species, Enterobacter species, Escherichia coli, Klebsiella species, Morganella morganii*, Proteus species, Pseudomonas aeruginosa, Bifidobacterium species, Clostridium species, Eubacterium species, Peptococcus species, Peptostreptococcus species, Propionibacterium species * , Bacteroides species including B. fragilis, Fusobacterium species
- Gynecologic infections. Enterococcus faecalis, Staphylococcus aureus (penicillinase-producing strains)*, Staphylococcus epidermidis, Streptococcus agalactiae (Group B streptococci), Enterobacter species * , Escherichia coli, Gardnerella vaginalis, Klebsiella species * , Proteus species, Bifidobacterium species * , Peptococcus species * , Peptostreptococcus species, Propionibacterium species * , Bacteroides species including B. fragilis *
- Bacterial septicemia. Enterococcus faecalis, Staphylococcus aureus (penicillinase-producing strains), Enterobacter species, Escherichia coli, Klebsiella species, Pseudomonas aeruginosa, Serratia species * , Bacteroides species including B. fragilis *
- Bone and joint infections. Enterococcus faecalis, Staphylococcus aureus (penicillinase-producing strains), Staphylococcus epidermidis, Enterobacter species, Pseudomonas aeruginosa
- Skin and skin structure infections. Enterococcus faecalis, Staphylococcus aureus (penicillinase-producing strains), Staphylococcus epidermidis, Acinetobacter species, Citrobacter species, Enterobacter species, Escherichia coli, Klebsiella species, Morganella morganii, Proteus vulgaris, Providencia rettgeri * , Pseudomonas aeruginosa, Serratia species, Peptococcus species, Peptostreptococcus species, Bacteroides species including B. fragilis, Fusobacterium species *
- Endocarditis. Staphylococcus aureus (penicillinase-producing strains)
- Polymicrobic infections. PRIMAXIN I.V. is indicated for polymicrobic infections including those in which S. pneumoniae (pneumonia, septicemia), S. pyogenes (skin and skin structure), or nonpenicillinase-producing S. aureus is one of the causative organisms. However, monobacterial infections due to these organisms are usually treated with narrower spectrum antibiotics, such as penicillin G.
PRIMAXIN I.V. is not indicated in patients with meningitis because safety and efficacy have not been established.
For Pediatric Use information, See PRECAUTIONS , Pediatric Use , and DOSAGE AND ADMINISTRATION sections.
Because of its broad spectrum of bactericidal activity against gram-positive and gram-negative aerobic and anaerobic bacteria, PRIMAXIN I.V. is useful for the treatment of mixed infections and as presumptive therapy prior to the identification of the causative organisms.
Although clinical improvement has been observed in patients with cystic fibrosis, chronic pulmonary disease, and lower respiratory tract infections caused by Pseudomonas aeruginosa, bacterial eradication may not necessarily be achieved.
As with other beta-lactam antibiotics, some strains of Pseudomonas aeruginosa may develop resistance fairly rapidly during treatment with PRIMAXIN I.V. During therapy of Pseudomonas aeruginosa infections, periodic susceptibility testing should be done when clinically appropriate.
Infections resistant to other antibiotics, for example, cephalosporins, penicillin, and aminoglycosides, have been shown to respond to treatment with PRIMAXIN I.V.
To reduce the development of drug-resistant bacteria and maintain the effectiveness of PRIMAXIN I.V. and other antibacterial drugs, PRIMAXIN I.V. should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
*Efficacy for this organism in this organ system was studied in fewer than 10 infections.
CONTRAINDICATIONS
PRIMAXIN I.V. is contraindicated in patients who have shown hypersensitivity to any component of this product.
WARNINGS
SERIOUS AND OCCASIONALLY FATAL HYPERSENSITIVITY (ANAPHYLACTIC) REACTIONS HAVE BEEN REPORTED IN PATIENTS RECEIVING THERAPY WITH BETA-LACTAMS. THESE REACTIONS ARE MORE APT TO OCCUR IN PERSONS WITH A HISTORY OF SENSITIVITY TO MULTIPLE ALLERGENS.
THERE HAVE BEEN REPORTS OF PATIENTS WITH A HISTORY OF PENICILLIN HYPERSENSITIVITY WHO HAVE EXPERIENCED SEVERE HYPERSENSITIVITY REACTIONS WHEN TREATED WITH ANOTHER BETA-LACTAM. BEFORE INITIATING THERAPY WITH PRIMAXIN I.V., CAREFUL INQUIRY SHOULD BE MADE CONCERNING PREVIOUS HYPERSENSITIVITY REACTIONS TO PENICILLINS, CEPHALOSPORINS, OTHER BETA-LACTAMS, AND OTHER ALLERGENS. IF AN ALLERGIC REACTION OCCURS, PRIMAXIN SHOULD BE DISCONTINUED.
SERIOUS ANAPHYLACTIC REACTIONS REQUIRE IMMEDIATE EMERGENCY TREATMENT WITH EPINEPHRINE. OXYGEN, INTRAVENOUS STEROIDS, AND AIRWAY MANAGEMENT, INCLUDING INTUBATION, MAY ALSO BE ADMINISTERED AS INDICATED.
Seizures and other CNS adverse experiences, such as confusional states and myoclonic activity, have been reported during treatment with PRIMAXIN I.V. (See PRECAUTIONS .)
Pseudomembranous colitis has been reported with nearly all antibacterial agents, including imipenem-cilastatin sodium, and may range in severity from mild to life threatening. Therefore, it is important to consider this diagnosis in patients who present with diarrhea subsequent to the administration of antibacterial agents.
Treatment with antibacterial agents alters the normal flora of the colon and may permit overgrowth of clostridia. Studies indicate that a toxin produced by Clostridium difficile is one primary cause of "antibiotic-associated colitis".
After the diagnosis of pseudomembranous colitis has been established, therapeutic measures should be initiated. Mild cases of pseudomembranous colitis usually respond to drug discontinuation alone. In moderate to severe cases, consideration should be given to management with fluids and electrolytes, protein supplementation and treatment with an antibacterial drug clinically effective against C. difficile colitis.
PRECAUTIONS
General
CNS adverse experiences such as confusional states, myoclonic activity, and seizures have been reported during treatment with PRIMAXIN I.V., especially when recommended dosages were exceeded. These experiences have occurred most commonly in patients with CNS disorders (e.g., brain lesions or history of seizures) and/or compromised renal function. However, there have been reports of CNS adverse experiences in patients who had no recognized or documented underlying CNS disorder or compromised renal function.
When recommended doses were exceeded, adult patients with creatinine clearances of </=20 mL/min/1.73 m 2 , whether or not undergoing hemodialysis, had a higher risk of seizure activity than those without impairment of renal function. Therefore, close adherence to the dosing guidelines for these patients is recommended. (See DOSAGE AND ADMINISTRATION .)
Patients with creatinine clearances of </=5 mL/min/1.73 m 2 should not receive PRIMAXIN I.V. unless hemodialysis is instituted within 48 hours.
For patients on hemodialysis, PRIMAXIN I.V. is recommended only when the benefit outweighs the potential risk of seizures.
Close adherence to the recommended dosage and dosage schedules is urged, especially in patients with known factors that predispose to convulsive activity. Anticonvulsant therapy should be continued in patients with known seizure disorders. If focal tremors, myoclonus, or seizures occur, patients should be evaluated neurologically, placed on anticonvulsant therapy if not already instituted, and the dosage of PRIMAXIN I.V. re-examined to determine whether it should be decreased or the antibiotic discontinued.
As with other antibiotics, prolonged use of PRIMAXIN I.V. may result in overgrowth of nonsusceptible organisms. Repeated evaluation of the patient's condition is essential. If superinfection occurs during therapy, appropriate measures should be taken.
Prescribing PRIMAXIN I.V. in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
Information for Patients
Patients should be counseled that antibacterial drugs including PRIMAXIN I.V. should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When PRIMAXIN I.V. is prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by PRIMAXIN I.V. or other antibacterial drugs in the future.
Laboratory Tests
While PRIMAXIN I.V. possesses the characteristic low toxicity of the beta-lactam group of antibiotics, periodic assessment of organ system functions, including renal, hepatic, and hematopoietic, is advisable during prolonged therapy.
Drug Interactions
Generalized seizures have been reported in patients who received ganciclovir and PRIMAXIN. These drugs should not be used concomitantly unless the potential benefits outweigh the risks.
Since concomitant administration of PRIMAXIN and probenecid results in only minimal increases in plasma levels of imipenem and plasma half-life, it is not recommended that probenecid be given with PRIMAXIN.
PRIMAXIN should not be mixed with or physically added to other antibiotics. However, PRIMAXIN may be administered concomitantly with other antibiotics, such as aminoglycosides.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Long term studies in animals have not been performed to evaluate carcinogenic potential of imipenem-cilastatin. Genetic toxicity studies were performed in a variety of bacterial and mammalian tests in in vivo and in vitro. The tests used were: V79 mammalian cell mutagenesis assay (imipenem-cilastatin sodium alone and imipenem alone), Ames test (cilastatin sodium alone and imipenem alone), unscheduled DNA synthesis assay (imipenem-cilastatin sodium) and in vivo mouse cytogenetics test (imipenem-cilastatin sodium). None of these tests showed any evidence of genetic alterations.
Reproductive tests in male and female rats were performed with imipenem-cilastatin sodium at intravenous doses up to 80 mg/kg/day and at a subcutaneous dose of 320 mg/kg/day, approximately equal to the highest recommended human dose of the intravenous formulation (on a mg/m 2 body surface area basis). Slight decreases in live fetal body weight were restricted to the highest dosage level. No other adverse effects were observed on fertility, reproductive performance, fetal viability, growth or postnatal development of pups.
Pregnancy: Teratogenic Effects
Pregnancy Category C: Teratology studies with cilastatin sodium at doses of 30, 100, and 300 mg/kg/day administered intravenously to rabbits and 40, 200, and 1000 mg/kg/day administered subcutaneously to rats, up to approximately 1.9 and 3.2 times †† the maximum recommended daily human dose (on a mg/m 2 body surface area basis) of the intravenous formulation of imipenem-cilastatin sodium (50 mg/kg/day) in the two species, respectively, showed no evidence of adverse effect on the fetus. No evidence of teratogenicity was observed in rabbits given imipenem at intravenous doses of 15, 30 or 60 mg/kg/day and rats given imipenem at intravenous doses of 225, 450, or 900 mg/kg/day, up to approximately 0.4 and 2.9 times †† the maximum recommended daily human dose (on a mg/m 2 body surface area basis) in the two species, respectively.
Teratology studies with imipenem-cilastatin sodium at intravenous doses of 20 and 80, and a subcutaneous dose of 320 mg/kg/day, up to 0.5 times †† (mice) to approximately equal to (rats) the highest recommended daily intravenous human dose (on a mg/m 2 body surface area basis) in pregnant rodents during the period of major organogenesis, revealed no evidence of teratogenicity.
Imipenem-cilastatin sodium, when administered subcutaneously to pregnant rabbits at dosages equivalent to the usual human dose of the intravenous formulation and higher, (1000-4000 mg/day) caused body weight loss, diarrhea, and maternal deaths. When comparable doses of imipenem-cilastatin sodium were given to non-pregnant rabbits, body weight loss, diarrhea, and deaths were also observed. This intolerance is not unlike that seen with other beta-lactam antibiotics in this species and is probably due to alteration of gut flora.
A teratology study in pregnant cynomolgus monkeys given imipenem-cilastatin sodium at doses of 40 mg/kg/day (bolus intravenous injection) or 160 mg/kg/day (subcutaneous injection) resulted in maternal toxicity including emesis, inappetence, body weight loss, diarrhea, abortion, and death in some cases. In contrast, no significant toxicity was observed when non-pregnant cynomolgus monkeys were given doses of imipenem-cilastatin sodium up to 180 mg/kg/day (subcutaneous injection). When doses of imipenem-cilastatin sodium (approximately 100 mg/kg/day or approximately 0.6 times †† the maximum recommended daily human dose of the intravenous formulation) were administered to pregnant cynomolgus monkeys at an intravenous infusion rate which mimics human clinical use, there was minimal maternal intolerance (occasional emesis), no maternal deaths, no evidence of teratogenicity, but an increase in embryonic loss relative to control groups.
No adverse effects on the fetus or on lactation were observed when imipenem-cilastatin sodium was administered subcutaneously to rats late in gestation at dosages up to 320 mg/kg/day, approximately equal to the highest recommended human dose (on a mg/m 2 body surface area basis).
There are, however, no adequate and well-controlled studies in pregnant women. PRIMAXIN I.V. should be used during pregnancy only if the potential benefit justifies the potential risk to the mother and fetus.
Nursing Mothers
It is not known whether imipenem-cilastatin sodium is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when PRIMAXIN I.V. is administered to a nursing woman.
Pediatric Use
Use of PRIMAXIN I.V. in pediatric patients, neonates to 16 years of age, is supported by evidence from adequate and well-controlled studies of PRIMAXIN I.V. in adults and by the following clinical studies and published literature in pediatric patients: Based on published studies of 178 ** pediatric patients >/=3 months of age (with non-CNS infections), the recommended dose of PRIMAXIN I.V. is 15-25 mg/kg/dose administered every six hours. Doses of 25 mg/kg/dose in patients 3 months to <3 years of age, and 15 mg/kg/dose in patients 3-12 years of age were associated with mean trough plasma concentrations of imipenem of 1.1±0.4 µg/mL and 0.6±0.2 µg/mL following multiple 60-minute infusions, respectively; trough urinary concentrations of imipenem were in excess of 10 µg/mL for both doses. These doses have provided adequate plasma and urine concentrations for the treatment of non-CNS infections. Based on studies in adults, the maximum daily dose for treatment of infections with fully susceptible organisms is 2.0 g per day, and of infections with moderately susceptible organisms (primarily some strains of P. aeruginosa ) is 4.0 g/day. (See Table 1 , DOSAGE AND ADMINISTRATION .) Higher doses (up to 90 mg/kg/day in older children) have been used in patients with cystic fibrosis. (See DOSAGE AND ADMINISTRATION .)
Based on studies of 135 *** pediatric patients </=3 months of age (weighing >/=1,500 gms), the following dosage schedule is recommended for non-CNS infections:
<1 wk of age: 25 mg/kg every 12 hrs
1-4 wks of age: 25 mg/kg every 8 hrs
4 wks-3 mos. of age: 25 mg/kg every 6 hrs.
In a published dose-ranging study of smaller premature infants (670-1,890 gms) in the first week of life, a dose of 20 mg/kg q12h by 15-30 minutes infusion was associated with mean peak and trough plasma imipenem concentrations of 43 µg/mL and 1.7 µg/mL after multiple doses, respectively. However, moderate accumulation of cilastatin in neonates may occur following multiple doses of PRIMAXIN I.V. The safety of this accumulation is unknown.
PRIMAXIN I.V. is not recommended in pediatric patients with CNS infections because of the risk of seizures.
PRIMAXIN I.V. is not recommended in pediatric patients <30 kg with impaired renal function, as no data are available.
Geriatric Use
Of the approximately 3600 subjects >/=18 years of age in clinical studies of PRIMAXIN I.V., including postmarketing studies, approximately 2800 received PRIMAXIN I.V. Of the subjects who received PRIMAXIN I.V., data are available on approximately 800 subjects who were 65 and over, including approximately 300 subjects who were 75 and over. No overall differences in safety or effectiveness were observed between these subjects and younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
This drug is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
No dosage adjustment is required based on age (see CLINICAL PHARMACOLOGY , Adults ). Dosage adjustment in the case of renal impairment is necessary (see DOSAGE AND ADMINISTRATION , Reduced Intravenous Schedule for Adults with Impaired Renal Function and/or Body Weight < 70 kg ).
†† Based on patient body surface area of 1.6 m 2 (weight of 60 kg).
** Two patients were less than 3 months of age.
*** One patient was greater than 3 months of age.
ADVERSE REACTIONS
Adults
PRIMAXIN I.V. is generally well tolerated. Many of the 1,723 patients treated in clinical trials were severely ill and had multiple background diseases and physiological impairments, making it difficult to determine causal relationship of adverse experiences to therapy with PRIMAXIN I.V.
Local Adverse Reactions
Adverse local clinical reactions that were reported as possibly, probably or definitely related to therapy with PRIMAXIN I.V. were:
Phlebitis/thrombophlebitis--3.1%
Pain at the injection site--0.7%
Erythema at the injection site--0.4%
Vein induration--0.2%
Infused vein infection--0.1%
Systemic Adverse Reactions
The most frequently reported systemic adverse clinical reactions that were reported as possibly, probably, or definitely related to PRIMAXIN I.V. were nausea (2.0%), diarrhea (1.8%), vomiting (1.5%), rash (0.9%), fever (0.5%), hypotension (0.4%), seizures (0.4%) (see PRECAUTIONS ), dizziness (0.3%), pruritus (0.3%), urticaria (0.2%), somnolence (0.2%).
Additional adverse systemic clinical reactions reported as possibly, probably or definitely drug related occurring in less than 0.2% of the patients or reported since the drug was marketed are listed within each body system in order of decreasing severity: Gastrointestinal -- pseudomembranous colitis (the onset of pseudomembranous colitis symptoms may occur during or after antibacterial treatment, see WARNINGS ), hemorrhagic colitis, hepatitis, jaundice, gastroenteritis, abdominal pain, glossitis, tongue papillar hypertrophy, staining of the teeth and/or tongue, heartburn, pharyngeal pain, increased salivation; Hematologic -- pancytopenia, bone marrow depression, thrombocytopenia, neutropenia, leukopenia, hemolytic anemia; CNS -- encephalopathy, tremor, confusion, myoclonus, paresthesia, vertigo, headache, psychic disturbances including hallucinations; Special Senses -- hearing loss, tinnitus, taste perversion; Respiratory -- chest discomfort, dyspnea, hyperventilation, thoracic spine pain; Cardiovascular -- palpitations, tachycardia; Skin -- Stevens-Johnson syndrome, toxic epidermal necrolysis, erythema multiforme, angioneurotic edema, flushing, cyanosis, hyperhidrosis, skin texture changes, candidiasis, pruritus vulvae; Body as a whole -- polyarthralgia, asthenia/weakness, drug fever; Renal --acute renal failure, oliguria/anuria, polyuria, urine discoloration. The role of PRIMAXIN I.V. in changes in renal function is difficult to assess, since factors predisposing to pre-renal azotemia or to impaired renal function usually have been present.
Adverse Laboratory Changes
Adverse laboratory changes without regard to drug relationship that were reported during clinical trials or reported since the drug was marketed were:
Hepatic: Increased ALT (SGPT), AST (SGOT), alkaline phosphatase, bilirubin and LDH
Hemic: Increased eosinophils, positive Coombs test, increased WBC, increased platelets, decreased hemoglobin and hematocrit, agranulocytosis, increased monocytes, abnormal prothrombin time, increased lymphocytes, increased basophils
Electrolytes: Decreased serum sodium, increased potassium, increased chloride
Renal: Increased BUN, creatinine
Urinalysis: Presence of urine protein, urine red blood cells, urine white blood cells, urine casts, urine bilirubin, and urine urobilinogen
Pediatric Patients
In studies of 178 pediatric patients >/=3 months of age, the following adverse events were noted:
The Most Common Clinical Adverse Experiences Without Regard to Drug Relationship
(Patient Incidence >1%)Adverse Experience No. of Patients (%) Digestive SystemDiarrhea7 * (3.9) Gastroenteritis2 (1.1) Vomiting2 * (1.1) SkinRash4 (2.2) Irritation, I.V. site2 (1.1) Urogenital SystemUrine discoloration2 (1.1) Cardiovascular SystemPhlebitis4 (2.2) * One patient had both vomiting and diarrhea and is counted in each category.
In studies of 135 patients (newborn to 3 months of age), the following adverse events were noted:
The Most Common Clinical Adverse Experiences Without Regard to Drug Relationship
(Patient Incidence >1%)Adverse Experience No. of Patients (%) Digestive SystemDiarrhea4 (3.0%) Oral Candidiasis2 (1.5%) SkinRash2 (1.5%) Urogenital SystemOliguria/anuria3 (2.2%) Cardiovascular SystemTachycardia2 (1.5%) Nervous SystemConvulsions8 (5.9%)
Patients >/=3 Months of Age With Normal Pretherapy but Abnormal During Therapy Laboratory Values Laboratory ParameterAbnormality No. of Patients With
Abnormalities/
No. of Patients With Lab Done
(%)HemoglobinAge <5 mos.:<10 gm %19/129 (14.7) 6 mos.-12 yrs.:<11.5 gm %HematocritAge <5 mos.:<30 vol %23/129 (17.8) 6 mos.-12 yrs.:<34.5 vol %Neutrophils</=1000/mm 3 (absolute)4/123 (3.3) Eosinophils>/=7%15/117 (12.8) Platelet Count>/=500 ths/mm 316/119 (13.4) Urine Protein>/=18/97 (8.2) Serum Creatinine>1.2 mg/dL0/105 (0) BUN>22 mg/dL0/108 (0) AST (SGOT)>36 IU/L14/78 (17.9) ALT (SGPT)>30 IU/L10/93 (10.8)
Patients (<3 Months of Age) With Normal Pretherapy but Abnormal During Therapy Laboratory Values Laboratory Parameter No. of Patients With
Abnormalities * (%)Eosinophil Countup11 (9.0%) Hematocritdown3 (2.0%) Hematocritup1 (1.0%) Platelet Countup5 (4.0%) Platelet Countdown2 (2.0%) Serum Creatinineup5 (5.0%) Bilirubinup3 (3.0%) Bilirubindown1 (1.0%) AST (SGOT)up5 (6.0%) ALT (SGPT)up3 (3.0%) Serum Alkaline Phosphateup2 (3.0%) * The denominator used for percentages was the number of patients for whom the test was performed during or post-treatment and, therefore, varies by test.
Examination of published literature and spontaneous adverse event reports suggested a similar spectrum of adverse events in adult and pediatric patients.
OVERDOSAGE
The acute intravenous toxicity of imipenem-cilastatin sodium in a ratio of 1:1 was studied in mice at doses of 751 to 1359 mg/kg. Following drug administration, ataxia was rapidly produced and clonic convulsions were noted in about 45 minutes. Deaths occurred within 4-56 minutes at all doses.
The acute intravenous toxicity of imipenem-cilastatin sodium was produced within 5-10 minutes in rats at doses of 771 to 1583 mg/kg. In all dosage groups, females had decreased activity, bradypnea, and ptosis with clonic convulsions preceding death; in males, ptosis was seen at all dose levels while tremors and clonic convulsions were seen at all but the lowest dose (771 mg/kg). In another rat study, female rats showed ataxia, bradypnea, and decreased activity in all but the lowest dose (550 mg/kg); deaths were preceded by clonic convulsions. Male rats showed tremors at all doses and clonic convulsions, and ptosis were seen at the two highest doses (1130 and 1734 mg/kg). Deaths occurred between 6 and 88 minutes with doses of 771 to 1734 mg/kg.
In the case of overdosage, discontinue PRIMAXIN I.V., treat symptomatically, and institute supportive measures as required. Imipenem-cilastatin sodium is hemodialyzable. However, usefulness of this procedure in the overdosage setting is questionable.
DOSAGE AND ADMINISTRATION
Adults
The dosage recommendations for PRIMAXIN I.V. represent the quantity of imipenem to be administered. An equivalent amount of cilastatin is also present in the solution. Each 125 mg, 250 mg, or 500 mg dose should be given by intravenous administration over 20 to 30 minutes. Each 750 mg or 1000 mg dose should be infused over 40 to 60 minutes. In patients who develop nausea during the infusion, the rate of infusion may be slowed.
The total daily dosage for PRIMAXIN I.V. should be based on the type or severity of infection and given in equally divided doses based on consideration of degree of susceptibility of the pathogen(s), renal function, and body weight. Adult patients with impaired renal function, as judged by creatinine clearance </= 70 mL/min/1.73 m 2 , require adjustment of dosage as described in the succeeding section of these guidelines.
Intravenous Dosage Schedule for Adults with Normal Renal Function and Body Weight >/=70 kg
Doses cited in Table I are based on a patient with normal renal function and a body weight of 70 kg. These doses should be used for a patient with a creatinine clearance of >/=71 mL/min/1.73 m 2 and a body weight of >/=70 kg. A reduction in dose must be made for a patient with a creatinine clearance </=70 mL/min/1.73 m 2 and/or a body weight less than 70 kg. (See Tables II and III.)
Dosage regimens in column A of Table I are recommended for infections caused by fully susceptible organisms which represent the majority of pathogenic species. Dosage regimens in column B of Table I are recommended for infections caused by organisms with moderate susceptibility to imipenem, primarily some strains of P. aeruginosa.
TABLE I
INTRAVENOUS DOSAGE SCHEDULE
FOR ADULTS WITH
NORMAL RENAL FUNCTION
AND BODY WEIGHT >/= 70 kgType or Severity
of InfectionA B Fully susceptible organisms including gram-positive and gram-negative aerobes and anaerobes Moderately susceptible organisms, primarily some strains of
P. aeruginosaMild250 mg q6h
(TOTAL DAILY
DOSE=1.0g)500 mg q6h
(TOTAL DAILY
DOSE=2.0g)Moderate500 mg q8h
(TOTAL DAILY
DOSE =1.5g)
or
500 mg q6h
(TOTAL DAILY
DOSE=2.0g)500 mg q6h
(TOTAL DAILY
DOSE=2.0g)
or
1 g q8h
(TOTAL DAILY
DOSE=3.0g)Severe, life
threatening
only500 mg q6h
(TOTAL DAILY
DOSE=2.0g)1 g q8h
(TOTAL DAILY
DOSE=3.0g)
or
1 g q6h
(TOTAL DAILY
DOSE=4.0g)Uncomplicated
urinary tract
infection250 mg q6h
(TOTAL DAILY
DOSE=1.0g)250 mg q6h
(TOTAL DAILY
DOSE=1.0g)Complicated
urinary tract
infection500 mg q6h
(TOTAL DAILY
DOSE=2.0g)500 mg q6h
(TOTAL DAILY
DOSE=2.0g)
Due to the high antimicrobial activity of PRIMAXIN I.V., it is recommended that the maximum total daily dosage not exceed 50 mg/kg/day or 4.0 g/day, whichever is lower . There is no evidence that higher doses provide greater efficacy. However, patients over twelve years of age with cystic fibrosis and normal renal function have been treated with PRIMAXIN I.V. at doses up to 90 mg/kg/day in divided doses, not exceeding 4.0 g/day.
Reduced Intravenous Dosage Schedule for Adults with Impaired Renal Function and/or Body Weight <70 kg
Patients with creatinine clearance of </= 70 mL/min/1.73 m 2 and/or body weight less than 70 kg require dosage reduction of PRIMAXIN I.V. as indicated in the tables below. Creatinine clearance may be calculated from serum creatinine concentration by the following equation:
T cc (Males)= __(wt. in kg) (140 - age)__ (72) (creatinine in mg/dL) T cc (Females)= 0.85 × above value
To determine the dose for adults with impaired renal function and/or reduced body weight:
- Choose a total daily dose from Table I based on infection characteristics.
-
a) If the total daily dose is 1.0 g, 1.5 g, or 2.0 g, use the appropriate subsection of Table II and continue with step 3.
b) If the total daily dose is 3.0 g or 4.0 g, use the appropriate subsection of Table III and continue with step 3. -
From Table II or III:
a) Select the body weight on the far left which is closest to the patient's body weight (kg).
b) Select the patient's creatinine clearance category.
c) Where the row and column intersect is the reduced dosage regimen.
TABLE II
REDUCED INTRAVENOUS DOSAGE OF PRIMAXIN I.V. IN ADULT PATIENTS WITH
IMPAIRED RENAL FUNCTION AND/OR BODY WEIGHT<70 kgand
Body
Weight
(kg)
is:If TOTAL DAILY DOSE from TABLE I is: 1.0 g/day 1.5 g/day 2.0 g/day and creatinine clearance
(mL/min/1.73m 2 ) is:and creatinine clearance
(mL/min/1.73m 2 ) is:and creatinine clearance
(mL/min/1.73m 2 ) is:>/=71 41-70 21-40 6-20 >/=71 41-70 21-40 6-20 >/=71 41-70 21-40 6-20 then the reduced
dosage regimen (mg) is:then the reduced
dosage regimen (mg) is:then the reduced
dosage regimen (mg) is:>/=70 250 250 250 250 500 250 250 250 500 500 250 250 q6h q8h q12h q12h q8h q6h q8h q12h q6h q8h q6h q12h 60 250 125 250 125 250 250 250 250 500 250 250 250 q8h q6h q12h q12h q6h q8h q8h q12h q8h q6h q8h q12h 50 125 125 125 125 250 250 250 250 250 250 250 250 q6h q6h q8h q12h q6h q8h q12h q12h q6h q6h q8h q12h 40 125 125 125 125 250 125 125 125 250 250 250 250 q6h q8h q12h q12h q8h q6h q8h q12h q6h q8h q12h q12h 30 125 125 125 125 125 125 125 125 250 125 125 125 q8h q8h q12h q12h q6h q8h q8h q12h q8h q6h q8h q12h TABLE III
REDUCED INTRAVENOUS DOSAGE OF PRIMAXIN I.V. IN ADULT PATIENTS WITH
IMPAIRED RENAL FUNCTION AND/OR BODY WEIGHT<70 kgand
Body
Weight
(kg)
is:If TOTAL DAILY DOSE from TABLE I is: 3.0 g/day 4.0 g/day and creatinine clearance
(mL/min/1.73m 2 ) is:and creatinine clearance
(mL/min/1.73m 2 ) is:>/=71 41-70 21-40 6-20 >/=71 41-70 21-40 6-20 then the reduced dosage regimen (mg) is: then the reduced dosage regimen (mg) is: >/=70 1000 500 500 500 1000 750 500 500 q8h q6h q8h q12h q6h q8h q6h q12h 60 750 500 500 500 1000 750 500 500 q8h q8h q8h q12h q8h q8h q8h q12h 50 500 500 250 250 750 500 500 500 q6h q8h q6h q12h q8h q6h q8h q12h 40 500 250 250 250 500 500 250 250 q8h q6h q8h q12h q6h q8h q6h q12h 30 250 250 250 250 500 250 250 250 q6h q8h q8h q12h q8h q6h q8h q12h
Patients with creatinine clearances of 6 to 20 mL/min/1.73 m 2 should be treated with PRIMAXIN I.V. 125 mg or 250 mg every 12 hours for most pathogens. There may be an increased risk of seizures when doses of 500 mg every 12 hours are administered to these patients.
Patients with creatinine clearance </=5 mL/min/1.73 m 2 should not receive PRIMAXIN I.V. unless hemodialysis is instituted within 48 hours. There is inadequate information to recommend usage of PRIMAXIN I.V. for patients undergoing peritoneal dialysis.
Hemodialysis
When treating patients with creatinine clearances of </=5 mL/min/1.73 m 2 who are undergoing hemodialysis , use the dosage recommendations for patients with creatinine clearances of 6-20 mL/min/1.73 m 2 . (See Reduced Intravenous Dosage Schedule for Adults with Impaired Renal Function and/or Body Weight <70 kg.) Both imipenem and cilastatin are cleared from the circulation during hemodialysis. The patient should receive PRIMAXIN I.V. after hemodialysis and at 12 hour intervals timed from the end of that hemodialysis session. Dialysis patients, especially those with background CNS disease, should be carefully monitored; for patients on hemodialysis, PRIMAXIN I.V. is recommended only when the benefit outweighs the potential risk of seizures. (See PRECAUTIONS .)
Pediatric Patients
See PRECAUTIONS , Pediatric Patients .
For pediatric patients >/=3 months of age, the recommended dose for non-CNS infections is 15-25 mg/kg/dose administered every six hours. Based on studies in adults, the maximum daily dose for treatment of infections with fully susceptible organisms is 2.0 g per day, and of infections with moderately susceptible organisms (primarily some strains of P. aeruginosa ) is 4.0 g/day. Higher doses (up to 90 mg/kg/day in older children) have been used in patients with cystic fibrosis.
For pediatric patients </=3 months of age (weighing >/=1,500 gms), the following dosage schedule is recommended for non-CNS infections:
<1 wk of age: 25 mg/kg every 12 hrs
1-4 wks of age: 25 mg/kg every 8 hrs
4 wks-3 mos. of age: 25 mg/kg every 6 hrs.
Doses less than or equal to 500 mg should be given by intravenous infusion over 15 to 30 minutes. Doses greater than 500 mg should be given by intravenous infusion over 40 to 60 minutes.
PRIMAXIN I.V. is not recommended in pediatric patients with CNS infections because of the risk of seizures.
PRIMAXIN I.V. is not recommended in pediatric patients <30 kg with impaired renal function, as no data are available.
PREPARATION OF SOLUTION
Infusion Bottles
Contents of the infusion bottles of PRIMAXIN I.V. Powder should be restored with 100 mL of diluent (see list of diluents under COMPATIBILITY AND STABILITY ) and shaken until a clear solution is obtained.
Vials
Contents of the vials must be suspended and transferred to 100 mL of an appropriate infusion solution.
A suggested procedure is to add approximately 10 mL from the appropriate infusion solution (see list of diluents under COMPATIBILITY AND STABILITY ) to the vial. Shake well and transfer the resulting suspension to the infusion solution container.
Benzyl alcohol as a preservative has been associated with toxicity in neonates. While toxicity has not been demonstrated in pediatric patients greater than three months of age, small pediatric patients in this age range may also be at risk for benzyl alcohol toxicity. Therefore, diluents containing benzyl alcohol should not be used when PRIMAXIN I.V. is constituted for administration to pediatric patients in this age range.
CAUTION: THE SUSPENSION IS NOT FOR DIRECT INFUSION.
Repeat with an additional 10 mL of infusion solution to ensure complete transfer of vial contents to the infusion solution. The resulting mixture should be agitated until clear.
ADD-Vantage ® ††† Vials
See separate INSTRUCTIONS FOR USE OF `PRIMAXIN I.V.' IN ADD-Vantage® VIALS. PRIMAXIN I.V. in ADD-Vantage® vials should be reconstituted with ADD-Vantage® diluent containers containing 100 mL of either 0.9% Sodium Chloride Injection or 100 mL 5% Dextrose Injection.
MONOVIAL ® ‡ Vials
See separate INSTRUCTIONS FOR USE OF `PRIMAXIN I.V.' IN MONOVIAL® VIALS. PRIMAXIN I.V. in MONOVIAL® vials should be reconstituted using an appropriate diluent in an infusion bag, with a maximum port length of 14 mm.
The MONOVIAL vial is not compatible with the ADD-Vantage® diluent bags.
††† Registered trademark of Abbott Laboratories, Inc.
‡ Registered trademark of Becton Dickinson and Company.
COMPATIBILITY AND STABILITY
Before reconstitution:
The dry powder should be stored at a temperature below 25°C (77°F).
Reconstituted solutions:
Solutions of PRIMAXIN I.V. range from colorless to yellow. Variations of color within this range do not affect the potency of the product.
PRIMAXIN I.V., as supplied in single use infusion bottles, vials and MONOVIAL® vials and reconstituted with the following diluents (see PREPARATION OF SOLUTION ), maintains satisfactory potency for 4 hours at room temperature or for 24 hours under refrigeration (5°C). Solutions of PRIMAXIN I.V. should not be frozen.
0.9% Sodium Chloride Injection
5% or 10% Dextrose Injection
5% Dextrose and 0.9% Sodium Chloride Injection
5% Dextrose Injection with 0.225% or 0.45% saline solution
5% Dextrose Injection with 0.15% potassium chloride solution
Mannitol 5% and 10%
PRIMAXIN I.V., as supplied in single dose ADD-Vantage® vials and reconstituted with the following diluents (see PREPARATION OF SOLUTION ), maintains satisfactory potency for 4 hours at room temperature.
0.9% Sodium Chloride Injection
5% Dextrose Injection
PRIMAXIN I.V. should not be mixed with or physically added to other antibiotics. However, PRIMAXIN I.V. may be administered concomitantly with other antibiotics, such as aminoglycosides.
HOW SUPPLIED
PRIMAXIN I.V. is supplied as a sterile powder mixture in single dose containers including vials, infusion bottles, ADD-Vantage® vials, and MONOVIAL® vials containing imipenem (anhydrous equivalent) and cilastatin sodium as follows:
No. 3514--250 mg imipenem equivalent and 250 mg cilastatin equivalent and 10 mg sodium bicarbonate as a buffer
NDC 0006-3514-58 in trays of 25 vials.
No. 3516--500 mg imipenem equivalent and 500 mg cilastatin equivalent and 20 mg sodium bicarbonate as a buffer
NDC 0006-3516-59 in trays of 25 vials.
No. 3517--500 mg imipenem equivalent and 500 mg cilastatin equivalent and 20 mg sodium bicarbonate as a buffer
NDC 0006-3517-75 in trays of 10 infusion bottles.
No. 3551 --250 mg imipenem equivalent and 250 mg cilastatin equivalent and 10 mg sodium bicarbonate as a buffer
NDC 0006-3551-58 in trays of 25 ADD-Vantage® vials.
No. 3552 --500 mg imipenem equivalent and 500 mg cilastatin equivalent and 20 mg sodium bicarbonate as a buffer
NDC 0006-3552-59 in trays of 25 ADD-Vantage® vials.
No. 3666 --500 mg imipenem equivalent and 500 mg cilastatin equivalent and 20 mg sodium bicarbonate as a buffer
NDC 0006-3666-59 in trays of 25 MONOVIAL® vials.
REFERENCES
- National Committee for Clinical Laboratory Standards, Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria that Grow Aerobically--Fourth Edition. Approved Standard NCCLS Document M7-A4, Vol. 17, No. 2 NCCLS, Villanova, PA, 1997.
- National Committee for Clinical Laboratory Standards, Performance Standards for Antimicrobial Disk Susceptibility Tests--Sixth Edition. Approved Standard NCCLS Document M2-A6, Vol. 17, No. 1 NCCLS, Villanova, PA, 1997.
- National Committee for Clinical Laboratory Standards, Method for Antimicrobial Susceptibility Testing of Anaerobic Bacteria--Third Edition. Approved Standard NCCLS Document M11-A3, Vol. 13, No. 26 NCCLS, Villanova, PA, 1993.
7882128 Issued August 2003
COPYRIGHT© Merck & CO., Inc., 1987, 1994, 1998
All rights reserved
Subscribe to the "News" RSS Feed 
TOP ۞
