-
Sanctura Tablets (Esprit)
PRESCRIBING INFORMATION
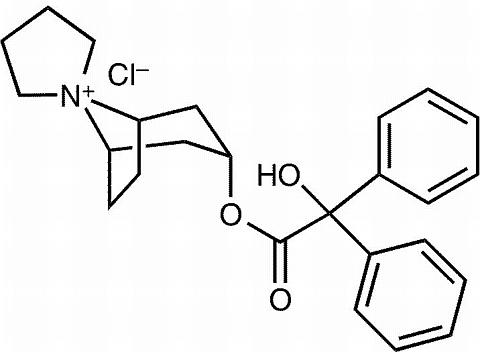
DESCRIPTION
Sanctura® (trospium chloride) is a quaternary ammonium compound with the chemical name of spiro[8-azoniabicyclo[3,2,1]octane-8,1'-pyrrolidinium]-3-[(hydroxydiphenyl-acetyl)-oxy]chloride(1(alpha), 3(beta), 5(beta))-(9CI). The empirical formula of trospium chloride is C 25 H 30 ClNO 3 ; and its molecular weight is 427.97. The structural formula of trospium chloride is represented below:
Trospium chloride is a fine, colorless to slightly yellow, crystalline solid. The compound's solubility in water is approximately 1 g/2 mL.
Each Sanctura tablet contains 20 mg of trospium chloride and is to be given orally. Each tablet also contains the following inactive ingredients: sucrose, wheat starch, microcrystalline cellulose, talc, lactose monohydrate, calcium carbonate, titanium dioxide, stearic acid, croscarmellose sodium, povidone, polyethylene glycol 8000, colloidal silicon dioxide, ferric oxide, carboxymethylcellulose sodium, white wax, magnesium stearate, and carnauba wax.
CLINICAL PHARMACOLOGY
Sanctura is an antispasmodic, antimuscarinic agent.
Trospium chloride antagonizes the effect of acetylcholine on muscarinic receptors in cholinergically innervated organs. Its parasympatholytic action reduces the tonus of smooth muscle in the bladder. Receptor assays showed that trospium chloride has negligible affinity for nicotinic receptors as compared to muscarinic receptors at concentrations obtained from therapeutic doses.
Pharmacodynamics
Placebo-controlled studies employing urodynamic variables were conducted in patients with conditions characterized by involuntary detrusor contractions. The results demonstrate that Sanctura increases maximum cystometric bladder capacity and volume at first detrusor contraction.
Pharmacokinetics
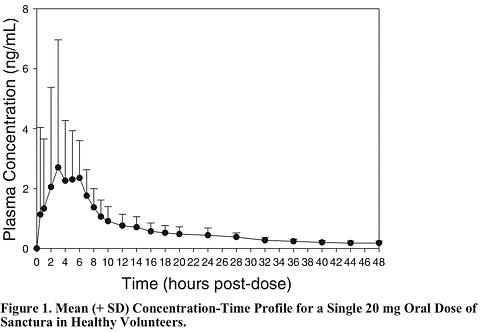
Absorption: After oral administration, less than 10% of the dose is absorbed. Mean absolute bioavailability of a 20 mg dose is 9.6% (range: 4.0-16.1%). Peak plasma concentrations (C max ) occur between 5 to 6 hours post-dose. Mean C max increases greater than dose-proportionally; a 3-fold and 4-fold increase in C max was observed for dose increases from 20 mg to 40 mg and from 20 mg to 60 mg, respectively. AUC exhibits dose linearity for single doses up to 60 mg. Sanctura exhibits diurnal variability in exposure with a decrease in C max and AUC of up to 59% and 33%, respectively, for evening relative to morning doses.
Effect of Food: Administration with a high fat meal resulted in reduced absorption, with AUC and C max values 70-80% lower than those obtained when Sanctura was administered while fasting. Therefore, it is recommended that Sanctura should be taken at least one hour prior to meals or on an empty stomach. (See DOSAGE AND ADMINISTRATION and PRECAUTIONS : Information for Patients ).
Distribution: Protein binding ranged from 50 to 85% when therapeutic concentration levels (0.5 - 50 ng/mL) were incubated with human serum in vitro .
The 3 H-trospium chloride ratio of plasma to whole blood was 1.6:1. This ratio indicates that the majority of 3 H-trospium chloride is distributed in plasma. The apparent volume of distribution for a 20 mg oral dose is 395 (± 140) liters.
Metabolism: The metabolic pathway of trospium in humans has not been fully defined. Of the 10% of the dose absorbed, metabolites account for approximately 40% of the excreted dose following oral administration. The major metabolic pathway is hypothesized as ester hydrolysis with subsequent conjugation of benzylic acid to form azoniaspironortropanol with glucuronic acid. Cytochrome P450 is not expected to contribute significantly to the elimination of trospium. In vitro data from human liver microsomes investigating the inhibitory effect of trospium on seven cytochrome P450 isoenzyme substrates (CYP1A2, 2A6, 2C9, 2C19, 2D6, 2E1, and 3A4) suggest a lack of inhibition at clinically relevant concentrations of trospium.
Excretion: The plasma half-life for Sanctura following oral administration is approximately 20 hours. After administration of oral 14 C-trospium chloride, the majority of the dose (85.2%) was recovered in feces and a smaller amount (5.8% of the dose) was recovered in urine; 60% of the radioactivity excreted in urine was unchanged trospium.
The mean renal clearance for trospium (29.07 L/hour) is 4-fold higher than average glomerular filtration rate, indicating that active tubular secretion is a major route of elimination for trospium. There may be competition for elimination with other compounds that are also renally eliminated (See PRECAUTIONS : Drug Interactions ).
A summary of mean (± standard deviation) pharmacokinetic parameters for a single 20 mg dose of Sanctura is provided in Table 1.
Table 1. Mean (± SD) Pharmacokinetic Parameter Estimates for a Single 20 mg Sanctura Dose in Healthy Volunteers.C max
(ng/mL)AUC 0-(infinity)
(ng/mL·hr)T max
(hr)t ½
(hr)3.5 ± 4.0 36.4 ± 21.8 5.3 ± 1.2 18.3 ± 3.2
The mean plasma concentration-time (+ SD) profile for Sanctura is shown in Figure 1.
Pharmacokinetics in Special Populations
Age: Age did not appear to significantly affect the pharmacokinetics of Sanctura, however, increased anticholinergic side effects unrelated to drug exposure were observed in patients >/=75 years of age. (See PRECAUTIONS : Geriatric Use and DOSAGE AND ADMINISTRATION ).
Pediatric:
Gender: Studies comparing the pharmacokinetics in different genders had conflicting results. When a single 40 mg Sanctura dose was administered to 16 elderly subjects, exposure was 45% lower in elderly females compared to elderly males. When 20 mg Sanctura was dosed BID for 4 days to 6 elderly males and 6 elderly females (60 to 75 years), AUC and C max were 26% and 68% higher, respectively, in females without hormone replacement therapy than in males.
Race: Pharmacokinetic differences due to race have not been studied.
Renal Insufficiency: Severe renal impairment significantly altered the disposition of Sanctura. A 4.5-fold and 2-fold increase in mean AUC 0-(infinity) and C max , respectively, and the appearance of an additional elimination phase with a long half-life (~33 hr) was detected in patients with severe renal insufficiency (CLcr < 30 mL/min) compared with healthy, nearly age-matched subjects. The different pharmacokinetic behavior of Sanctura in patients with severe renal insufficiency necessitates adjustment of dosage frequency. The pharmacokinetics of Sanctura have not been studied in people with moderate or mild renal impairment (CLcr ranging from 30-80 mL/min).(See PRECAUTIONS : General and DOSAGE AND ADMINISTRATION ).
Hepatic Insufficiency: There is no information regarding the effect of severe hepatic impairment on exposure to Sanctura. Maximum trospium concentration (C max ) increased 12% and 63% in subjects with mild and moderate hepatic impairment, respectively, compared to healthy subjects. Mean area under the plasma concentration-time curve (AUC) was similar. Caution should be used when administering Sanctura to patients with moderate and severe hepatic dysfunction. (See PRECAUTIONS : General ).
Drug-Drug Interactions
No in vivo drug-drug interaction studies have been performed to assess the effect of concomitant medications on the pharmacokinetics of Sanctura or to assess the effect of Sanctura on the pharmacokinetics of other drugs. Sanctura is metabolized by esterases and excreted by the kidneys by a combination of tubular secretion and glomerular filtration. Based on in vitro data, no clinically relevant interactions with the metabolism of trospium are expected. However, drugs which are actively secreted may interact with trospium by competing for renal tubular secretion. (See PRECAUTIONS : Drug Interactions ).
Electrophysiology
The effect of 20 mg BID and up to 100 mg BID Sanctura on QT interval was evaluated in a single-blind, randomized, placebo and active (moxifloxacin 400 mg QD) controlled 5 day parallel trial in 170 male and female healthy volunteer subjects aged 18 to 45 years. The QT interval was measured over a 24 hour period at steady state. The 100 mg BID dose of Sanctura was chosen because this achieves the C max expected in severe renal impairment. Sanctura was not associated with an increase in individual corrected (QTcI) or Fridericia corrected (QTcF) QT interval at any time during steady state measurement, while moxifloxacin was associated with a 6.4 msec increase in QTcF.
In this study, asymptomatic, non-specific T wave inversions were observed more often in subjects receiving Sanctura than in subjects receiving moxifloxacin or placebo following five days of treatment. This finding was not observed during routine safety monitoring in 2 other placebo-controlled clinical trials in 591 Sanctura-treated overactive bladder patients (See CLINICAL STUDIES ). The clinical significance of T wave inversion in this study is unknown. Sanctura is associated with an increase in heart rate that correlates with increasing plasma concentrations. In the study described above, Sanctura demonstrated a mean increase in heart rate compared to placebo of 9.1 bpm for the 20 mg dose and of 18.0 bpm for the 100 mg dose. In the two U.S. placebo-controlled trials in patients with overactive bladder, the mean increase in heart rate compared to placebo in Study 1 was observed to be 3.0 bpm and in Study 2 was 4.0 bpm.
CLINICAL STUDIES
Sanctura was evaluated for the treatment of patients with overactive bladder who had symptoms of urinary frequency, urgency, and urge incontinence in two U.S. 12-week, placebo-controlled studies and one 9-month open label extension.
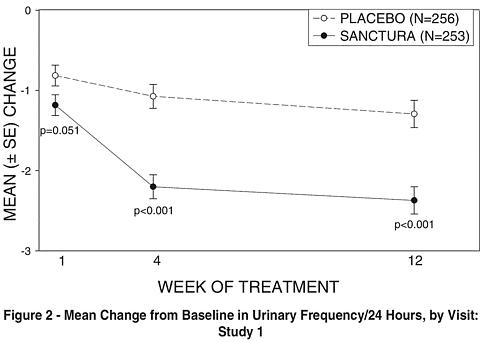
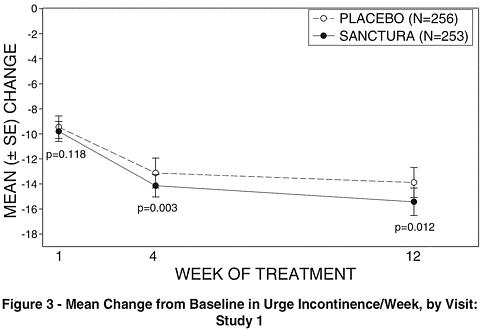
Study 1 was a randomized, double-blind, placebo-controlled, parallel-group study in 523 patients. A total of 262 patients received Sanctura 20 mg twice daily and 261 patients received placebo. The majority of patients were Caucasian (85%) and female (74%) with a mean age of 61 years (range 21 to 90 years). Entry criteria required that patients have urge or mixed incontinence (with a predominance of urge), urge incontinence episodes of at least 7 per week, and greater than 70 micturitions per week. The patient's medical history and urinary diary during the treatment-free baseline confirmed the diagnosis. Reductions in urinary frequency, urge incontinence episodes and urinary void volume for placebo and Sanctura treatment groups are summarized in Table 2 and Figures 2 and 3.
Table 2. Mean (SE) change from baseline to end of treatment (Week 12 or last observation carried forward) for urinary frequency, urge incontinence episodes, and void volume in Study 1.Efficacy endpoint Placebo
N=256Sanctura
N=253P-value Urinary frequency/24 hours a , *Mean baseline12.9 12.7 Mean change from baseline-1.3 (0.2) -2.4 (0.2) <0.001 Urge incontinence episodes/week b , *Mean baseline30.1 27.3 Mean change from baseline-13.9 (1.2) -15.4 (1.1) 0.012 Urinary void volume/toilet void (mL) a , cMean baseline156.6 155.1 Mean change from baseline7.7 (3.1) 32.1 (3.1) <0.001 a Treatment differences assessed by analysis of variance for ITT:LOCF data set. b Treatment differences assessed by ranked analysis of variance for ITT:LOCF data set. c Placebo N=253, Sanctura N=248. * Denotes co-primary endpoint
ITT=intent-to-treat, LOCF=last observation carried forward.
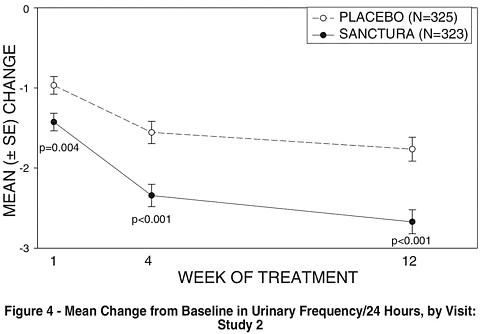
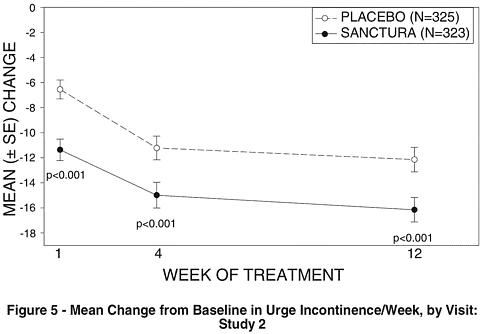
Study 2 was nearly identical in design to Study 1. A total of 329 patients received Sanctura 20 mg twice daily and 329 patients received placebo. The majority of patients were Caucasian (88%) and female (82%) with a mean age of 61 years (range 19 to 94 years). Entry criteria were identical to Study 1. Reductions in urinary frequency, urge incontinence episodes, and urinary void volume for placebo and Sanctura treatment groups are summarized in Table 3 and Figures 4 and 5.
Table 3. Mean (SE) change from baseline to end of treatment (Week 12 or last observation carried forward) for urinary frequency, urge incontinence episodes, and void volume in Study 2.Efficacy endpoint Placebo
N=325Sanctura
N=323P-value Urinary frequency/24 hours a , *Mean baseline13.2 12.9 Mean change from baseline-1.8 (0.2) -2.7 (0.2) <0.001 Urge incontinence episodes/week bMean baseline27.3 26.9 Mean change from baseline-12.1 (1.0) -16.1 (1.0) <0.001 Urinary void volume/toilet void (mL) a , cMean baseline154.6 154.8 Mean change from baseline9.4 (2.8) 35.6 (2.8) <0.001 a Treatment differences assessed by analysis of variance for ITT:LOCF data set. b Treatment differences assessed by ranked analysis of variance for ITT:LOCF data set. c Placebo N=320, Sanctura N=319. * Denotes primary endpoint
ITT=intent-to-treat, LOCF=last observation carried forward.
INDICATIONS AND USAGE
Sanctura is indicated for the treatment of overactive bladder with symptoms of urge urinary incontinence, urgency, and urinary frequency.
CONTRAINDICATIONS
Sanctura is contraindicated in patients with urinary retention, gastric retention, or uncontrolled narrow-angle glaucoma and in patients who are at risk for these conditions. Sanctura is also contraindicated in patients who have demonstrated hypersensitivity to the drug or its ingredients.
PRECAUTIONS
General
Risk of Urinary Retention: Sanctura should be administered with caution to patients with clinically significant bladder outflow obstruction because of the risk of urinary retention.
Decreased Gastrointestinal Motility: Sanctura should be administered with caution to patients with gastrointestinal obstructive disorders because of the risk of gastric retention (See CONTRAINDICATIONS ). Sanctura, like other anticholinergic drugs, may decrease gastrointestinal motility and should be used with caution in patients with conditions such as ulcerative colitis, intestinal atony and myasthenia gravis.
Controlled Narrow-angle Glaucoma: In patients being treated for narrow-angle glaucoma, Sanctura should only be used if the potential benefits outweigh the risks and in that circumstance only with careful monitoring.
Patients with Renal Insufficiency: Dose modification is recommended in patients with severe renal insufficiency (CLcr < 30mL/min). In such patients, Sanctura should be administered as 20 mg once a day at bedtime (See DOSAGE AND ADMINISTRATION ).
Patients with Hepatic Impairment: Caution should be used when administering Sanctura in patients with moderate or severe hepatic dysfunction (See CLINICAL PHARMACOLOGY : Pharmacokinetics in Special Populations ).
Information for Patients
Patients should be informed that anticholinergic agents, such as Sanctura, may produce clinically significant adverse effects related to anticholinergic pharmacological activity. For example, heat prostration (fever and heat stroke due to decreased sweating) can occur when anticholinergics such as Sanctura are used in a hot environment. Because anticholinergics such as Sanctura may also produce dizziness or blurred vision, patients should be advised to exercise caution. Patients should be informed that alcohol may enhance the drowsiness caused by anticholinergic agents.
Sanctura should be taken 1 hour prior to meals or on an empty stomach. If a dose is skipped, patients are advised to take their next dose 1 hour prior to their next meal.
Drug Interactions
The concomitant use of Sanctura with other anticholinergic agents that produce dry mouth, constipation, and other anticholinergic pharmacological effects may increase the frequency and/or severity of such effects. Anticholinergic agents may potentially alter the absorption of some concomitantly administered drugs due to anticholinergic effects on gastrointestinal motility.
Drugs Eliminated by Active Tubular Secretion: Although studies to assess drug-drug interactions with Sanctura have not been conducted, Sanctura has the potential for pharmacokinetic interactions with other drugs that are eliminated by active tubular secretion (e.g. digoxin, procainamide, pancuronium, morphine, vancomycin, metformin and tenofovir). Coadministration of Sanctura with drugs that are eliminated by active renal tubular secretion may increase the serum concentration of Sanctura and/or the coadministered drug due to competition for this elimination pathway. Careful patient monitoring is recommended in patients receiving such drugs (See CLINICAL PHARMACOLOGY : Excretion , and CLINICAL PHARMACOLOGY : Drug-Drug Interactions ).
Drug-Laboratory-Test Interactions
Interactions between Sanctura and laboratory tests have not been studied.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity studies with trospium chloride were conducted in mice and rats. A 78-week carcinogenicity study in mice and a 104-week carcinogenicity study in rats were conducted at doses of 2, 20, and 200 mg/kg/day. No evidence of a carcinogenic effect was found in either mice or rats. The 200 mg/kg/day dose in the mouse and rat represents approximately 25 and 60 times, respectively, the human dose based on body surface area. At 200 mg/kg/day in the mouse and rat after 4 weeks the AUC was 34 and 753 ng·h/mL, respectively. The exposure in the rat is 8.6-fold higher than the AUC following 40 mg daily exposure in healthy young or elderly subjects (88 ng·h/mL).
Trospium chloride was not mutagenic in tests for detection of gene mutations in bacteria (Ames test) and mammalian cells (L5178Y mouse lymphoma and CHO cells) or in vivo in the rat micronucleus test.
No evidence of impaired fertility was observed in rats administered doses up to 200 mg/kg/day (about 10 multiples of the expected clinical exposure via AUC).
Pregnancy: Teratogenic Effects
Pregnancy Category C: Trospium chloride has been shown to cause maternal toxicity in rats and a decrease in fetal survival in rats administered approximately 10 times the expected clinical exposure (AUC). The no effect levels for maternal and fetal toxicity were approximately equivalent to the expected clinical exposure in rats, and about 5-6 times the expected clinical exposure in rabbits. No malformations or developmental delays were observed. There are no adequate and well controlled studies in pregnant women. Sanctura should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Nursing Mothers
Trospium chloride (2 mg/kg PO and 50 µg/kg IV) was excreted, to a limited extent (<1%), into the milk of lactating rats. The activity observed in the milk was primarily from the parent compound. It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when Sanctura is administered to a nursing woman. Sanctura should be used during lactation only if the potential benefit justifies the potential risk to the newborn.
Pediatric Use
The safety and effectiveness of Sanctura in pediatric patients have not been established.
Geriatric Use
Of the 591 patients with overactive bladder who received treatment with Sanctura in the two U.S., placebo-controlled, efficacy and safety studies, 249 patients (42%) were 65 years of age and older. Eighty-eight Sanctura-treated patients (15%) were >/= 75 years of age.
In these 2 studies, the incidence of commonly reported anticholinergic adverse events in patients treated with Sanctura (including dry mouth, constipation, dyspepsia, UTI, and urinary retention) was higher in patients 75 years of age and older as compared to younger patients. This effect may be related to an enhanced sensitivity to anticholinergic agents in this patient population (See CLINICAL PHARMACOLOGY : Pharmacokinetics in Special Populations and DOSAGE AND ADMINISTRATION ). Therefore, based upon tolerability, the dose frequency of Sanctura may be reduced to 20 mg once daily in patients 75 years of age and older.
ADVERSE REACTIONS
The safety of Sanctura was evaluated in Phase 2 and 3 controlled clinical trials in a total of 2975 patients, who were treated with Sanctura (N=1673), placebo (N=1056) or active control medications (N=246). Of this total, 1181 patients participated in two, twelve-week, Phase 3, U.S., efficacy and safety studies and a 9-month open-label extension. Of this total, 591 patients received Sanctura 20 mg twice daily. In all controlled trials combined, 232 and 208 patients received treatment with Sanctura for at least 24 and 52 weeks, respectively.
In all placebo-controlled trials combined, the incidence of serious adverse events was 2.9% among patients receiving Sanctura 20 mg BID and 1.5% among patients receiving placebo. Of these, 0.2% and 0.3% were judged to be at least possibly related to treatment with Sanctura or placebo, respectively, by the investigator.
Table 4 lists treatment emergent adverse events from the combined 12-week U.S. safety and efficacy trials that were judged to be at least possibly related to treatment with Sanctura by the investigator, were reported by at least 1% of patients, and were reported more frequently in the Sanctura group than in the placebo group.
The 2 most common adverse events reported by patients receiving Sanctura 20 mg BID were dry mouth and constipation. The single most frequently reported adverse event for Sanctura, dry mouth, occurred in 20.1% of Sanctura treated patients and 5.8% of patients receiving placebo. In the two Phase 3 U.S. studies, dry mouth led to discontinuation in 1.9% of patients treated with Sanctura 20 mg BID. For the patients who reported dry mouth, most had their first occurrence of the event within the first month of treatment.
Table 4. Incidence (%) of adverse events judged at
least possibly related to treatment with Sanctura,
reported in >/= 1% of all patients treated with Sanctura
and more frequent with Sanctura (20 mg BID) than
placebo in Studies 1 and 2 combined.Adverse EventPlacebo
(N=590)Sanctura
20 mg BID
(N=591)Gastrointestinal disordersDry mouth34 (5.8) 119 (20.1) Constipation27 (4.6) 57 (9.6) Abdominal pain upper7 (1.2) 9 (1.5) Constipation aggravated5 (0.8) 8 (1.4) Dyspepsia2 (0.3) 7 (1.2) Flatulence5 (0.8) 7 (1.2) Nervous system disordersHeadache12 (2.0) 25 (4.2) General DisordersFatigue8 (1.4) 11 (1.9) Renal and Urinary
Disorders8 (1.4) 11 (1.9) Urinary retention2 (0.3) 7 (1.2) Eye DisordersDry eyes NOS2 (0.3) 7 (1.2) Abbreviations: BID=twice daily, NOS=not otherwise specified.
Other adverse events from the Phase 3, U.S., placebo-controlled trials judged possibly related to treatment with Sanctura by the investigator, occurring in >/=0.5% of Sanctura-treated patients, and more common with Sanctura than placebo are: tachycardia NOS, vision blurred, abdominal distension, vomiting NOS, dysgeusia, dry throat, and dry skin.
During controlled clinical studies, one event of angioneurotic edema was reported.
Postmarketing Surveillance
Additional spontaneous adverse events, regardless of relationship to drug, reported from marketing experience with trospium chloride include: gastritis, palpitations, supraventricular tachycardia, chest pain, Stevens-Johnson syndrome, anaphylactic reaction, syncope, rhabdomyolysis, vision abnormal, hallucinations and delirium, and "hypertensive crisis".
OVERDOSAGE
Management of Overdosage
Overdosage with Sanctura may result in severe anticholinergic effects. Treatment should be provided according to symptoms and supportive. In the event of overdosage, ECG monitoring is recommended.
A 7-month-old baby experienced tachycardia and mydriasis after administration of a single dose of trospium 10 mg given by a sibling. The baby's weight was reported as 5 kg. Following admission into the hospital and about 1 hour after ingestion of the trospium, medicinal charcoal was administered for detoxification. While hospitalized, the baby experienced mydriasis and tachycardia up to 230 beats/minute. Therapeutic intervention was not deemed necessary. The baby was discharged as completely recovered the following day.
DOSAGE AND ADMINISTRATION
The recommended dose is 20 mg twice daily. Sanctura should be dosed at least one hour before meals or given on an empty stomach.
Dosage modification is recommended in the following patient populations:
For patients with severe renal impairment (CLcr < 30 mL/min), the recommended dose is 20 mg once daily at bedtime (See PRECAUTIONS : General ).
In geriatric patients >/= 75 years of age, dose may be titrated down to 20 mg once daily based upon tolerability (See PRECAUTIONS : Geriatric Use ).
HOW SUPPLIED
Sanctura® tablets 20 mg (brownish yellow, biconvex, glossy coated tablets printed with black ink) are supplied as follows:
60 count HDPE bottle- NDC 65473-980-04
500 count HDPE bottle- NDC 65473-980-02
14 count blister (PVC/Paper backed foil) - NDC 65473-980-70
14 count blister (PVC-Aclar/Paper backed foil) - NDC 65473-980-71
Store at controlled room temperature 20° to 25°C (68° to 77°F) (see USP).
Rx only
Manufactured for:
Esprit Pharma, Inc.
East Brunswick, NJ 08816 USA
and
Indevus Pharmaceuticals, Inc.
Lexington, MA 02421 USA
Manufactured by:
Madaus AG
Troisdorf, Germany
Address Medical Inquiries to:
(866) 230-0375
Subscribe to the "News" RSS Feed 
TOP ۞
