-
Suprane Liquid for Inhalation (Baxter Anesthesia)
DESCRIPTION
SUPRANE® (desflurane, USP), a nonflammable liquid administered via vaporizer, is a general inhalation anesthetic. It is (±)1,2,2,2-tetrafluoroethyl difluoromethyl ether:
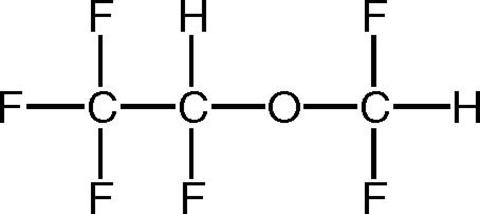 Some physical constants are:Molecular weight168.04Specific gravity (at 20°C/4°C)1.465Vapor pressure in mm Hg669 mm Hg @ 20°C731 mm Hg @ 22°C757 mm Hg @ 22.8°C(boiling point; 1atm)764 mm Hg @ 23°C798 mm Hg @ 24°C869 mm Hg @ 26°CPartition coefficients at 37°C:Blood/Gas0.424Olive Oil/Gas18.7Brain/Gas0.54Mean Component/Gas Partition Coefficients:Polypropylene (Y piece)6.7Polyethylene (circuit tube)16.2Latex rubber (bag)19.3Latex rubber (bellows)10.4Polyvinylchloride (endotracheal tube)34.7
Some physical constants are:Molecular weight168.04Specific gravity (at 20°C/4°C)1.465Vapor pressure in mm Hg669 mm Hg @ 20°C731 mm Hg @ 22°C757 mm Hg @ 22.8°C(boiling point; 1atm)764 mm Hg @ 23°C798 mm Hg @ 24°C869 mm Hg @ 26°CPartition coefficients at 37°C:Blood/Gas0.424Olive Oil/Gas18.7Brain/Gas0.54Mean Component/Gas Partition Coefficients:Polypropylene (Y piece)6.7Polyethylene (circuit tube)16.2Latex rubber (bag)19.3Latex rubber (bellows)10.4Polyvinylchloride (endotracheal tube)34.7Desflurane is nonflammable as defined by the requirements of International Electrotechnical Commission 601-2-13.
Desflurane is a colorless, volatile liquid below 22.8°C. Data indicate that desflurane is stable when stored under normal room lighting conditions according to instructions.
Desflurane is chemically stable. The only known degradation reaction is through prolonged direct contact with soda lime producing low levels of fluoroform (CHF 3 ). The amount of CHF 3 obtained is similar to that produced with MAC-equivalent doses of isoflurane. No discernible degradation occurs in the presence of strong acids.
Desflurane does not corrode stainless steel, brass, aluminum, anodized aluminum, nickel plated brass, copper, or beryllium.
CLINICAL PHARMACOLOGY
SUPRANE® (desflurane, USP) is a volatile liquid inhalation anesthetic minimally biotransformed in the liver in humans. Less than 0.02% of the SUPRANE® absorbed can be recovered as urinary metabolites (compared to 0.2% for isoflurane).
Minimum alveolar concentration (MAC) of desflurane in oxygen for a 25 year-old adult is 7.3%. The MAC of SUPRANE® (desflurane, USP) decreases with increasing age and with addition of depressants such as opioids or benzodiazepines. (See DOSAGE AND ADMINISTRATION for details).
Pharmacokinetics
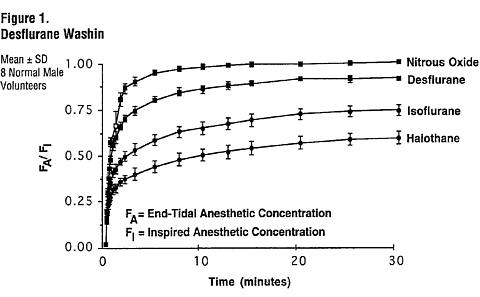
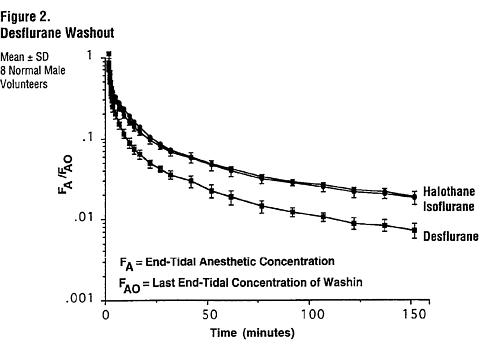
Due to the volatile nature of desflurane in plasma samples, the washin-washout profile of desflurane was used as a surrogate of plasma pharmacokinetics. Eight healthy male volunteers first breathed 70% N 2 O/30% O 2 for 30 minutes and then a mixture of SUPRANE® (desflurane, USP) 2.0%, isoflurane 0.4%, and halothane 0.2% for another 30 minutes. During this time, inspired and end-tidal concentrations (F I and F A ) were measured. The F A /F I (washin) value at 30 minutes for desflurane was 0.91, compared to 1.00 for N 2 O, 0.74 for isoflurane, and 0.58 for halothane (See Figure 1 ). The washin rates for halothane and isoflurane were similar to literature values. The washin was faster for desflurane than for isoflurane and halothane at all time points. The F A /F AO (washout) value at 5 minutes was 0.12 for desflurane, 0.22 for isoflurane, and 0.25 for halothane (See Figure 2 ). The washout for SUPRANE® was more rapid than that for isoflurane and halothane at all elimination time points. By 5 days, the F A /F AO for desflurane is 1/20th of that for halothane or isoflurane.
Pharmacodynamics
Changes in the clinical effects of SUPRANE® (desflurane, USP) rapidly follow changes in the inspired concentration. The duration of anesthesia and selected recovery measures for SUPRANE® are given in the following tables:
In 178 female outpatients undergoing laparoscopy, premedicated with fentanyl (1.5-2.0 µg/kg), anesthesia was initiated with propofol 2.5 mg/kg, desflurane/N 2 O 60% in O 2 or desflurane/O 2 alone. Anesthesia was maintained with either propofol 1.5-9.0 mg/kg/hr, desflurane 2.6-8.4% in N 2 O 60% in O 2 , or desflurane 3.1-8.9% in O 2 .
EMERGENCE AND RECOVERY AFTER OUTPATIENT LAPAROSCOPY
178 FEMALES, AGES 20-47
TIMES IN MINUTES: MEAN ± SD (RANGE)Induction:Propofol Propofol Desflurane/N 2 O Desflurane/O 2 Maintenance:Propofol/N 2 O Desflurane/N 2 O Desflurane/N 2 O Desflurane/O 2 Number of Pts:N = 48 N = 44 N = 43 N = 43 Median age30
(20-43)26
(21-47)29
(21-42)30
(20-40)Anesthetic
Time49 ± 53
(8-336)45 ± 35
(11-178)44 ± 29
(14-149)41 ± 26
(19-126)Time to open
eyes7 ± 3
(2-19)5 ± 2 *
(2-10)5 ± 2 *
(2-12)4 ± 2 *
(1-11)Time to state
name9 ± 4
(4-22)8 ± 3
(3-18)7 ± 3 *
(3-16)7 ± 3 *
(2-15)Time to stand80 ± 34
(40-200)86 ± 55
(30-320)81 ± 38
(35-190)77 ± 38
(35-200)Time to walk110 ± 6
(47-285)122 ± 85
(37-375)108 ± 59
(48-220)108 ± 66
(49-250)Time to fit for
discharge152 ± 75
(66-375)157 ± 80
(73-385)150 ± 66
(68-310)155 ± 73
(69-325)*Differences were statistically significant (p < 0.05) by Dunnett's procedure comparing all treatments to the propofol-propofol/N 2 O (induction and maintenance) group. Results for comparisons greater than one hour after anesthesia show no differences between groups and considerable variability within groups.In 88 unpremedicated outpatients, anesthesia was initiated with thiopental 3-9 mg/kg or desflurane in O 2 . Anesthesia was maintained with isoflurane 0.7-1.4% in N 2 O 60%, desflurane 1.8-7.7% in N 2 O 60%, or desflurane 4.4-11.9% in O 2 .
EMERGENCE AND RECOVERY TIMES IN OUTPATIENT SURGERY
46 MALES, 42 FEMALES, AGES 19-70
TIMES IN MINUTES: MEAN ± SD (RANGE)Induction:Thiopental Thiopental Thiopental Desflurane/O 2 Maintenance:Isoflurane/N 2 O Desflurane/N 2 O Desflurane/O 2 Desflurane/O 2 Number of Pts:N = 23 N = 21 N = 23 N = 21 Median age43
(20-70)40
(22-67)43
(19-70)41
(21-64)Anesthetic
Time49 ± 23
(11-94)50 ± 19
(16-80)50 ± 27
(16-113)51 ± 23
(19-117)Time to open
eyes13 ± 7
(5-33)9 ± 3 *
(4-16)12 ± 8
(4-39)8 ± 2 *
(4-13)Time to state
name17 ± 10
(6-44)11 ± 4 *
(6-19)15 ± 10
(6-46)9 ± 3 *
(5-14)Time to walk195 ± 67
(124-365)176 ± 60
(101-315)168 ± 34
(119-258)181 ± 42
(92-252)Time to fit for
discharge205 ± 53
(153-365)202 ± 41
(144-315)197 ± 35
(155-280)194 ± 37
(134-288)*Differences were statistically significant (p < 0.05) by Dunnett's procedure comparing all treatments to the thiopental-isoflurane/N 2 O (induction and maintenance) group. Results for comparisons greater than one hour after anesthesia show no differences between groups and considerable variability within groups.Recovery from anesthesia was assessed at 30, 60, and 90 minutes following 0.5 MAC desflurane (3%) or isoflurane (0.6%) in N 2 O 60% using subjective and objective tests. At 30 minutes after anesthesia, only 43% of the isoflurane group were able to perform the psychometric tests compared to 76% in the desflurane group (p < 0.05).
RECOVERY TESTS: PERCENT OF PREOPERATIVE BASELINE VALUES
16 MALES, 22 FEMALES, AGES 20-65
PERCENT: MEAN ± SD60 minutes
After Anesthesia90 minutes
After AnesthesiaMaintenance:Desflurane/N 2 O Isoflurane/N 2 O Desflurane/N 2 O Isoflurane/N 2 O Confusion (DELTA)66±6 47±8 75±7 * 56±8 Fatigue (DELTA)70±9 * 33±6 89±12 * 47±8 Drowsiness (DELTA)66±5 * 36±8 76±7 * 49±9 Clumsiness (DELTA)65±5 49±8 80±7 * 57±9 Comfort (DELTA)59±7 * 30±6 60±8 * 31±7 DSST **/* score74±4 * 50±9 75±4 * 55±7 Trieger Tests **/* **/*67±5 74±6 90±6 83±7 (DELTA) Visual analog scale (values from 0-100; 100=baseline)**/* DSST = Digit Symbol Substitution Test**/* **/* Trieger Test = Dot Connecting Test* Differences were statistically significant (p < 0.05) using a two-sample t-testSUPRANE® (desflurane, USP) was studied in twelve volunteers receiving no other drugs. Hemodynamic effects during controlled ventilation (PaCO 2 38mm Hg) were:
HEMODYNAMIC EFFECTS OF DESFLURANE DURING CONTROLLED VENTILATION
12 MALE VOLUNTEERS, AGES 16-26
MEAN ± SD (RANGE)Heart Rate
(beats/min)Mean Arterial
Pressure (mmHg)Cardiac Index
(L/min/m 2 )Total MAC
EquivalentEnd-Tidal
% Des/O 2End-Tidal
%Des/N 2 OO 2 N 2 O O 2 N 2 O O 2 N 2 O 0 0%/21% 0%/0% 69 ± 4
(63-76)70 ± 6
(62-85)85 ± 9
(74-102)85 ± 9
(74-102)3.7 ± 0.4
(3.0-4.2)3.7 ± 0.4
(3.0-4.2)0.8 6%/94% 3%/60% 73 ± 5
(67-80)77 ± 8
(67-97)61 ± 5 *
(55-70)69 ± 5 *
(62-80)3.2 ± 0.5
(2.6-4.0)3.3 ± 0.5
(2.6-4.1)1.2 9%/91% 6%/60% 80 ± 5 *
(72-84)77 ± 7
(67-90)59 ± 8 *
(44-71)63 ± 8 *
(47-74)3.4 ± 0.5
(2.6-4.1)3.1 ± 0.4 *
(2.6-3.8)1.7 12%/88% 9%/60% 94 ± 14 *
(78-109)79 ± 9
(61-91)51 ± 12 *
(31-66)59 ± 6 *
(46-68)3.5 ± 0.9
(1.7-4.7)3.0 ± 0.4 *
(2.4-3.6)*Differences were statistically significant (p<0.05) compared to awake values, Newman-Keul's method of multiple comparison. When the same volunteers breathed spontaneously during desflurane anesthesia, systemic vascular resistance and mean arterial blood pressure decreased; cardiac index, heart rate, stroke volume, and central venous pressure (CVP) increased compared to values when the volunteers were conscious. Cardiac index, stroke volume, and CVP were greater during spontaneous ventilation than during controlled ventilation.
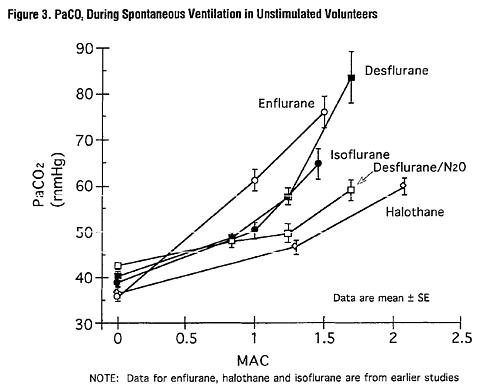
During spontaneous ventilation in the same volunteers, increasing the concentration of SUPRANE® (desflurane, USP) from 3% to 12% decreased tidal volume and increased arterial carbon dioxide tension and respiratory rate. The combination of N 2 O 60% with a given concentration of desflurane gave results similar to those with desflurane alone. Respiratory depression produced by desflurane is similar to that produced by other potent inhalation agents.
The use of desflurane concentrations higher than 1.5 MAC may produce apnea.
CLINICAL TRIALS
SUPRANE® (desflurane, USP) was evaluated in 1,843 patients including ambulatory (N=1,061), cardiovascular (N=277), geriatric (N=103), neurosurgical (N=40), and pediatric (N=235) patients. Clinical experience with these patients and with 1,087 control patients in these studies not receiving desflurane are described below. Although desflurane can be used in adults for the inhalation induction of anesthesia via mask, it produces a high incidence of respiratory irritation (coughing, breathholding, apnea, increased secretions, laryngospasm). For incidence, see ADVERSE REACTIONS . Oxyhemoglobin saturation below 90% occurred in 6% of patients (from pooled data, N = 370 adults).
Ambulatory Surgery
SUPRANE® (desflurane, USP) plus N 2 O was compared to isoflurane plus N 2 O in multicenter studies (21 sites) of 792 ASA physical status I, II, or III patients aged 18-76 years (median 32).
INDUCTION: Anesthetic induction begun with thiopental and continued with desflurane was associated with a 7% incidence of oxyhemoglobin saturation of 90% or less (from pooled data, N = 307) compared with 5% in patients in whom anesthesia was induced with thiopental and isoflurane (from pooled data, N = 152).
MAINTENANCE & RECOVERY: SUPRANE® (desflurane, USP) with or without N 2 O or other anesthetics was generally well tolerated. There were no differences between desflurane and the other anesthetics studied in the times that patients were judged fit for discharge.
In one outpatient study, patients received a standardized anesthetic consisting of thiopental 4.2-4.4 mg/kg, fentanyl 3.5-4.0 µg/kg, vecuronium 0.05-0.07 mg/kg, and N 2 O 60% in oxygen with either desflurane 3% or isoflurane 0.6%. Emergence times were significantly different; but times to sit up and discharge were not different (see Table).
RECOVERY PROFILES AFTER DESFLURANE 3% IN
N 2 O 60% vs ISOFLURANE 0.6% IN N 2 O 60%
IN OUTPATIENTS
16 MALES, 22 FEMALES, AGES 20-65
MEAN ± SDIsoflurane Desflurane Number21 17 Anesthetic time (min)127 ± 80 98 ± 55 Recovery time to:Follow commands (min)11.1 ± 7.9 6.5 ± 2.3 * Sit up (min)113 ± 27 95 ± 56 Fit for discharge (min)231 ± 40 207 ± 54 * Difference was statistically significant from the isoflurane group (p < 0.05), unadjusted for multiple comparisons.
Cardiovascular Surgery
Desflurane was compared to isoflurane, sufentanil or fentanyl for the anesthetic management of coronary artery bypass graft (CABG), abdominal aortic aneurysm, peripheral vascular and carotid endarterectomy surgery in 7 studies at 15 centers involving a total of 558 patients. In all patients except the desflurane vs sufentanil study, the volatile anesthetics were supplemented with intravenous opioids, usually fentanyl. Blood pressure and heart rate were controlled by changes in concentration of the volatile anesthetics or opioids and cardiovascular drugs if necessary. Oxygen (100%) was the carrier gas in 253 of 277 desflurane cases (24 of 277 received N 2 O/O 2 ).
ARDIOVASCULAR PATIENTS BY AGENT AND TYPE OF SURGERY
418 MALES, 140 FEMALES, AGES 27-87 (MEDIAN 64)13 Centers 1 Center 1 Center Type of
SurgeryIsoflurane DesfluraneSufentanil DesfluraneFentanyl DesfluraneCABG58 57 100 100 25 25 Abd Aorta29 25 - - - - Periph Vasc24 24 - - - - Carotid Art45 46 - - - - -- -- -- -- -- -- Total156 152 100 100 25 25 No differences were found in cardiovascular outcome (death, myocardial infarction, ventricular tachycardia or fibrillation, heart failure) among desflurane and the other anesthetics.
INDUCTION: Desflurane should not be used as the sole agent for anesthetic induction in patients with coronary artery disease or any patients where increases in heart rate or blood pressure are undesirable. In the desflurane vs sufentanil study, anesthetic induction with desflurane without opioids was associated with new transient ischemia in 14 patients vs 0 in the sufentanil group. In the desflurane group, mean heart rate, arterial pressure, and pulmonary blood pressure increased and stroke volume decreased in contrast to no change in the sufentanil group. Cardiovascular drugs were used frequently in both groups: especially esmolol in the desflurane group (56% vs 0%) and phenylephrine in the sufentanil group (43% vs 27%). When 10 µg/kg of fentanyl was used to supplement induction of anesthesia at one other center, continuous 2-lead ECG analysis showed a low incidence of myocardial ischemia and no difference between desflurane and isoflurane. If desflurane is to be used in patients with coronary artery disease, it should be used in combination with other medications for induction of anesthesia, preferably intravenous opioids and hypnotics.
MAINTENANCE & RECOVERY: In studies where desflurane or isoflurane anesthesia was supplemented with fentanyl, there were no differences in hemodynamic variables or the incidence of myocardial ischemia in the patients anesthetized with desflurane compared to those anesthetized with isoflurane.
During the precardiopulmonary bypass period, in the desflurane vs sufentanil study where the desflurane patients received no intravenous opioid, more desflurane patients required cardiovascular adjuvants to control hemodynamics than the sufentanil patients. During this period, the incidence of ischemia detected by ECG or echocardiography was not statistically different between desflurane (18 of 99) and sufentanil (9 of 98) groups. However, the duration and severity of ECG-detected myocardial ischemia was significantly less in the desflurane group. The incidence of myocardial ischemia after cardiopulmonary bypass and in the ICU did not differ between groups.
Geriatric Surgery
SUPRANE® (desflurane, USP) plus N 2 O was compared to isoflurane plus N 2 O in a multicenter study (6 sites) of 203 ASA physical status II or III elderly patients, aged 57-91 years (median 71).
INDUCTION: Most patients were premedicated with fentanyl (mean 2 µg/kg), preoxygenated, and received thiopental (mean 4.3 mg/kg IV) or thiamylal (mean 4 mg/kg IV) followed by succinylcholine (mean 1.4 mg/kg IV) for intubation.
MAINTENANCE & RECOVERY: Heart rate and arterial blood pressure remained within 20% of preinduction baseline values during administration of SUPRANE® (desflurane, USP) 0.5-7.7% (average 3.6%) with 50-60% N 2 O. Induction, maintenance, and recovery cardiovascular measurements did not differ from those during isoflurane/N 2 O administration nor did the postoperative incidence of nausea and vomiting differ. The most common cardiovascular adverse event was hypotension occurring in 8% of the SUPRANE® patients and 6% of the isoflurane patients.
Neurosurgery
SUPRANE® (desflurane, USP) was studied in 38 patients aged 26-76 years (median 48 years), ASA physical status II or III undergoing neurosurgical procedures for intracranial lesions.
INDUCTION: Induction consisted of standard neuroanesthetic techniques including hyperventilation and thiopental.
MAINTENANCE: No change in cerebrospinal fluid pressure (CSFP) was observed in 8 patients who had intracranial tumors when the dose of desflurane was 0.5 MAC in N 2 O 50%. In another study of 9 patients with intracranial tumors, 0.8 MAC desflurane/air/O 2 did not increase CSFP above postinduction baseline values. In a different study of 10 patients receiving 1.1 MAC desflurane/air/O 2 , CSFP increased 7 mm Hg (range 3-13 mm Hg increase, with final values of 11-26 mm Hg) above the predrug values.
All volatile anesthetics may increase intracranial pressure in patients with intracranial space occupying lesions. In such patients, desflurane should be administered at 0.8 MAC or less, and in conjunction with a barbiturate induction and hyperventilation (hypocapnia) in the period before cranial decompression. Appropriate attention must be paid to maintain cerebral perfusion pressure. The use of a lower dose of desflurane and the administration of a barbiturate and mannitol would be predicted to lessen the effect of desflurane on CSFP.
Under hypocapnic conditions (PaCO 2 27 mm Hg) desflurane 1 and 1.5 MAC did not increase cerebral blood flow (CBF) in 9 patients undergoing craniotomies. CBF reactivity to increasing PaCO 2 from 27 to 35 mm Hg was also maintained at 1.25 MAC desflurane/air/O 2 .
Pediatric Surgery
SUPRANE® (desflurane, USP) or halothane with or without N 2 O was used to anesthetize 235 patients aged 2 weeks-12 years (median 2 years), ASA physical status I or II.
INDUCTION: SUPRANE® (desflurane, USP) is not recommended for induction of general anesthesia in infants or pediatric patients because of a high incidence of moderate to severe laryngospasm, coughing, breathholding, and secretions. The occurrence of oxyhemoglobin desaturation was 26%. For incidence, see ADVERSE REACTIONS .
MAINTENANCE & RECOVERY: The concentration of SUPRANE® (desflurane, USP) required for maintenance of general anesthesia is age-dependent (see INDIVIDUALIZATION OF DOSE ). Changes in blood pressure during maintenance of and recovery from anesthesia with desflurane/N 2 O/O 2 are similar to those observed with halothane/N 2 O/O 2 . Heart rate during maintenance of anesthesia is approximately 10 beats per minute faster with desflurane than with halothane. Patients were judged fit for discharge from post-anesthesia care units within one hour with both desflurane and halothane. There were no differences in the incidence of nausea and vomiting between patients receiving desflurane or halothane.
INDIVIDUALIZATION OF DOSE
(Also see DOSAGE AND ADMINISTRATION )
Preanesthetic Medication: Issues such as whether or not to premedicate and the choice of premedicant(s) must be individualized. In clinical studies, patients scheduled to be anesthetized with desflurane frequently received IV pre-anesthetic medication, such as opioid and/or benzodiazepine.
INDUCTION: In adults, some premedicated with opioid, a frequent starting concentration was 3% desflurane, increased in 0.5-1.0% increments every 2 to 3 breaths. End-tidal concentrations of 4-11% SUPRANE® (desflurane, USP) with and without N 2 O, produced anesthesia within 2 to 4 minutes. When desflurane was tested as the primary anesthetic induction agent, the incidence of upper airway irritation (apnea, breathholding, laryngospasm, coughing and secretions) was high (see ADVERSE REACTIONS ). During induction in adults, the overall incidence of oxyhemoglobin desaturation (SpO 2 < 90%) was 6%.
After induction in adults with an intravenous drug such as thiopental or propofol, desflurane can be started at approximately 0.5-1 MAC, whether the carrier gas is O 2 or N 2 O/O 2 .
MAINTENANCE: Surgical levels of anesthesia in adults may be maintained with concentrations of 2.5-8.5% SUPRANE® (desflurane, USP) with or without the concomitant use of nitrous oxide. In children, surgical levels of anesthesia may be maintained with concentrations of 5.2-10% SUPRANE® with or without the concomitant use of nitrous oxide.
During the maintenance of anesthesia, increasing concentrations of SUPRANE® (desflurane, USP) produce dose-dependent decreases in blood pressure. Excessive decreases in blood pressure may be due to depth of anesthesia and in such instances may be corrected by decreasing the inspired concentration of SUPRANE®.
Concentrations of desflurane exceeding 1 MAC may increase heart rate. Thus with this drug, an increased heart rate may not serve reliably as a sign of inadequate anesthesia. SUPRANE® (desflurane, USP) decreases the doses of neuromuscular blocking agents required (see PRECAUTIONS , Drug Interactions ).
INDICATIONS AND USAGE
SUPRANE® (desflurane, USP) is indicated as an inhalation agent for induction and/or maintenance of anesthesia for inpatient and outpatient surgery in adults (see PRECAUTIONS ).
SUPRANE® (desflurane, USP) is not recommended for induction of anesthesia in pediatric patients because of a high incidence of moderate to severe upper airway adverse events (see WARNINGS ). After induction of anesthesia with agents other than SUPRANE®, and tracheal intubation, SUPRANE® is indicated for maintenance of anesthesia in infants and children.
CONTRAINDICATIONS
SUPRANE® (desflurane, USP) should not be used in patients with a known or suspected genetic susceptibility to malignant hyperthermia.
Known sensitivity to SUPRANE® (desflurane, USP) or to other halogenated agents.
WARNINGS
Pediatric Use: SUPRANE® (desflurane, USP) is not recommended for induction of general anesthesia via mask in infants or children because of the high incidence of moderate to severe laryngospasm in 50% of patients, coughing 72%, breathholding 68%, increase in secretions 21% and oxyhemoglobin desaturation 26%.
SUPRANE® (desflurane, USP) should be administered only by persons trained in the administration of general anesthesia, using a vaporizer specifically designed and designated for use with desflurane. Facilities for maintenance of a patent airway, artificial ventilation, oxygen enrichment, and circulatory resuscitation must be immediately available. Hypotension and respiratory depression increase as anesthesia is deepened.
PRECAUTIONS
During the maintenance of anesthesia, increasing concentrations of SUPRANE® (desflurane, USP) produce dose-dependent decreases in blood pressure. Excessive decreases in blood pressure may be related to depth of anesthesia and in such instances may be corrected by decreasing the inspired concentration of SUPRANE®.
Concentrations of desflurane exceeding 1 MAC may increase heart rate. Thus an increased heart rate may not be a sign of inadequate anesthesia.
In patients with intracranial space occupying lesions, SUPRANE® (desflurane, USP) should be administered at 0.8 MAC or less, in conjunction with a barbiturate induction and hyperventilation (hypocapnia). Appropriate measures should be taken to maintain cerebral perfusion pressure (see CLINICAL TRIALS , Neurosurgery ).
In patients with coronary artery disease, maintenance of normal hemodynamics is important to the avoidance of myocardial ischemia. Desflurane should not be used as the sole agent for anesthetic induction in patients with coronary artery disease or patients where increases in heart rate or blood pressure are undesirable. It should be used with other medications, preferably intravenous opioids and hypnotics (see CLINICAL TRIALS , Cardiovascular Surgery ).
Inspired concentrations of SUPRANE® (desflurane, USP) greater than 12% have been safely administered to patients, particularly during induction of anesthesia. Such concentrations will proportionately dilute the concentration of oxygen; therefore, maintenance of an adequate concentration of oxygen may require a reduction of nitrous oxide or air if these gases are used concurrently.
The recovery from general anesthesia should be assessed carefully before patients are discharged from the post anesthesia care unit (PACU).
SUPRANE® (desflurane, USP), like some other inhalational anesthetics, can react with desiccated carbon dioxide (CO 2 ) absorbents to produce carbon monoxide which may result in elevated levels of carboxyhemoglobin in some patients. Case reports suggest that barium hydroxide lime and soda lime become desiccated when fresh gases are passed through the CO 2 absorber cannister at high flow rates over many hours or days. When a clinician suspects that CO 2 absorbent may be desiccated, it should be replaced before the administration of SUPRANE® (desflurane, USP).
As with other halogenated anesthetic agents, SUPRANE® (desflurane, USP) may cause sensitivity hepatitis in patients who have been sensitized by previous exposure to halogenated anesthetics (see CONTRAINDICATIONS ).
Drug Interactions
No clinically significant adverse interactions with commonly used preanesthetic drugs, or drugs used during anesthesia (muscle relaxants, intravenous agents, and local anesthetic agents) were reported in clinical trials. The effect of desflurane on the disposition of other drugs has not been determined.
Like isoflurane, desflurane does not predispose to premature ventricular arrhythmias in the presence of exogenously infused epinephrine in swine.
BENZODIAZEPINES AND OPIOIDS (MAC REDUCTION):
Benzodiazepines (midazolam 25-50 µg/kg) decrease the MAC of desflurane by 16% as do the opioids (fentanyl 3-6 µg/kg) by 50% (see DOSAGE AND ADMINISTRATION ).
NEUROMUSCULAR BLOCKING AGENTS:
Anesthetic concentrations of desflurane at equilibrium (administered for 15 or more minutes before testing) reduced the ED 95 of succinylcholine by approximately 30% and that of atracurium and pancuronium by approximately 50% compared to N 2 O/opioid anesthesia. The effect of desflurane on duration of nondepolarizing neuromuscular blockade has not been studied.
DOSAGE OF MUSCLE RELAXANT CAUSING 95%
DEPRESSION IN NEUROMUSCULAR BLOCKADEDesflurane Mean ED 95 (µg/kg) Concentration Pancuronium Atracurium Succinylcholine 0.65 MAC 60%
N 2 O/O 226 123 - 1.25 MAC 60%
N 2 O/O 218 91 - 1.25 MAC O 222 120 362 Dosage reduction of neuromuscular blocking agents during induction of anesthesia may result in delayed onset of conditions suitable for endotracheal intubation or inadequate muscle relaxation, because potentiation of neuromuscular blocking agents requires equilibration of muscle with the delivered partial pressure of desflurane.
Among nondepolarizing drugs, only pancuronium and atracurium interactions have been studied. In the absence of specific guidelines:
- For endotracheal intubation, do not reduce the dose of nondepolarizing muscle relaxants or succinylcholine.
- During maintenance of anesthesia, the dose of nondepolarizing muscle relaxants is likely to be reduced compared to that during N 2 O/opioid anesthesia. Administration of supplemental doses of muscle relaxants should be guided by the response to nerve stimulation.
Malignant Hyperthermia: In susceptible individuals, potent inhalation anesthetic agents may trigger a skeletal muscle hypermetabolic state leading to high oxygen demand and the clinical syndrome known as malignant hyperthermia. In genetically susceptible pigs, desflurane induced malignant hyperthermia. The clinical syndrome is signalled by hypercapnia, and may include muscle rigidity, tachycardia, tachypnea, cyanosis, arrhythmias, and/or unstable blood pressure. Some of these nonspecific signs may also appear during light anesthesia: acute hypoxia, hypercapnia, and hypovolemia.
Treatment of malignant hyperthermia includes discontinuation of triggering agents, administration of intravenous dantrolene sodium, and application of supportive therapy. (Consult prescribing information for dantrolene sodium intravenous for additional information on patient management.) Renal failure may appear later, and urine flow should be monitored and sustained if possible.
Renal or Hepatic Insufficiency
Nine patients receiving SUPRANE® (desflurane, USP) (N=9) were compared to 9 patients receiving isoflurane, all with chronic renal insufficiency (serum creatinine 1.5-6.9 mg/dL). No differences in hematological or biochemical tests, including renal function evaluation, were seen between the two groups. Similarly, no differences were found in a comparison of patients receiving either SUPRANE® (desflurane, USP) (N=28) or isoflurane (N=30) undergoing renal transplant.
Eight patients receiving SUPRANE® (desflurane, USP) were compared to six patients receiving isoflurane, all with chronic hepatic disease (viral hepatitis, alcoholic hepatitis, or cirrhosis). No differences in hematological or biochemical tests, including hepatic enzymes and hepatic function evaluation, were seen.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Animal carcinogenicity studies have not been performed with SUPRANE® (desflurane, USP). In vitro and in vivo genotoxicity studies did not demonstrate mutagenicity or chromosomal damage by SUPRANE®. Tests for genotoxicity included the Ames mutation assay, the metaphase analysis of human lymphocytes, and the mouse micronucleus assay.
Fertility was not affected after 1 MAC-Hour per day exposure (cumulative 63 and 14 MAC-Hours for males and females, respectively). At higher doses, parental toxicity (mortalities and reduced weight gain) was observed which could affect fertility.
Teratogenic Effects: No teratogenic effect was observed at approximately 10 and 13 cumulative MAC-Hour exposures at 1 MAC-Hour per day during organogenesis in rats or rabbits. At higher doses increased incidences of post-implantation loss and maternal toxicity were observed. However, at 10 MAC-Hours cumulative exposure in rats, about 6% decrease in the weight of male pups was observed at preterm caesarean delivery.
Pregnancy Category B: There are no adequate and well-controlled studies in pregnant women. SUPRANE® (desflurane, USP) should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Rats exposed to desflurane at 1 MAC-hour per day from gestation day 15 to lactation day 21, did not show signs of dystocia. Body weight of pups delivered by these dams at birth and during lactation were comparable to that of control pups. No treatment related behavioral changes were reported in these pups during lactation.
Labor and Delivery: The safety of desflurane during labor or delivery has not been demonstrated.
Nursing Mothers: The concentrations of desflurane in milk are probably of no clinical importance 24 hours after anesthesia. Because of rapid washout, desflurane concentrations in milk are predicted to be below those found with other volatile potent anesthetics.
Geriatric Use: The average MAC for SUPRANE® (desflurane, USP) in a 70 year old patient is two-thirds the MAC for a 20 year old patient (see DOSAGE AND ADMINISTRATION ).
Pediatric Use: SUPRANE® (desflurane, USP) is not recommended for induction of general anesthesia via mask in pediatric patients because of the high incidence of moderate to severe laryngospasm, coughing, breathholding and increase in secretions and oxyhemoglobin desaturation (see WARNINGS ).
Neurosurgical Use: SUPRANE® (desflurane, USP) may produce a dose-dependent increase in cerebrospinal fluid pressure (CSFP) when administered to patients with intracranial space occupying lesions. Desflurane should be administered at 0.8 MAC or less, and in conjunction with a barbiturate induction and hyperventilation (hypocapnia) until cerebral decompression in patients with known or suspected increases in CSFP. Appropriate attention must be paid to maintain cerebral perfusion pressure (see CLINICAL TRIALS , Neurosurgery ).
ADVERSE REACTIONS
Adverse event information is derived from controlled clinical trials, the majority of which were conducted in the United States. The studies were conducted using a variety of premedications, other anesthetics, and surgical procedures of varying length. Most adverse events reported were mild and transient, and may reflect the surgical procedures, patient characteristics (including disease) and/or medications administered.
Of the 1,843 patients exposed to SUPRANE® (desflurane, USP) in clinical trials, 370 adults and 152 children were induced with desflurane alone and 687 patients were maintained principally with desflurane. The frequencies given reflect the percent of patients with the event. Each patient was counted once for each type of adverse event. They are presented in alphabetical order according to body system.
PROBABLY CAUSALLY RELATED: Incidence greater than 1%.Induction (use as a mask inhalation agent):ADULT PATIENTS (N=370):Coughing 34%, breathholding 30%, apnea 15%,
increased secretions * , laryngospasm * ,
oxyhemoglobin desaturation (SpO 2 <90%) *
pharyngitis *PEDIATRIC PATIENTS (N=152):Coughing 72%, breathholding 68%, laryngospasm
50%, oxyhemoglobin desaturation (SpO 2 <90%)
26%, increased secretions 21%, bronchospasm * .
(See WARNINGS )Maintenance or RecoveryADULT AND PEDIATRIC PATIENTS (N=687):Body as a Whole:Headache.Cardiovascular:Bradycardia, hypertension, nodal arrhythmia,
tachycardia.Digestive:Nausea 27%, vomiting 16%.Nervous system:Increased Salivation.Respiratory:Apnea * , breathholding,
cough increased * ,
laryngospasm * , pharyngitis.Special Senses:Conjunctivitis (conjunctival hyperemia)* Incidence of events: 3%-10%
PROBABLY CAUSALLY RELATED: Incidence less than 1% and reported in 3 or more patients, regardless of severity (N=1,843) Adverse reactions reported only from postmarketing experience or in the literature, not seen in clinical trials, are considered rare and are italicized.Cardiovascular:Arrhythmia, bigeminy, abnormal electrocardiogram,
myocardial ischemia, vasodilation.Digestive:Hepatitis .Nervous System:Agitation, dizziness.Respiratory:Asthma, dyspnea, hypoxia.CAUSAL RELATIONSHIP UNKNOWN: Incidence less than 1% and reported in 3 or more patients, regardless of severity (N=1,843)Body as a Whole:Fever.Cardiovascular:Hemorrhage, myocardial
infarct.Metabolic and Nutrition:Increased creatinine phosphokinase.Musculoskeletal System:Myalgia.Skin and Appendages:Pruritis.See PRECAUTIONS for information regarding pediatric use and malignant hyperthermia.
Laboratory Findings: Transient elevations in glucose and white blood cell count may occur as with use of other anesthetic agents.
DRUG ABUSE AND DEPENDENCE
The potential drug abuse liability, and dependence associated with SUPRANE® (desflurane, USP) have not been studied.
OVERDOSAGE
In the event of overdosage, or suspected overdosage, take the following actions: discontinue administration of SUPRANE® (desflurane, USP), maintain a patent airway, initiate assisted or controlled ventilation with oxygen, and maintain adequate cardiovascular function.
DOSAGE AND ADMINISTRATION
Deliver SUPRANE® (desflurane, USP) from a vaporizer specifically designed and designated for use with desflurane.
The administration of general anesthesia must be individualized based on the patient's response (see INDIVIDUALIZATION OF DOSE ). The following two tables provide mean relative potency based upon age and drug interaction studies in predominately ASA physical status I or II patients.
EFFECT OF AGE ON MAC OF DESFLURANE
MEAN ± SD (percent atmospheres)AgeN O 2 100% N N 2 O 60% 2 weeks6 9.2 ± 0.0 - - 10 weeks5 9.4 ± 0.4 - - 9 months4 10.0 ± 0.7 5 7.5 ± 0.8 2 years3 9.1 ± 0.6 - - 3 years- - 5 6.4 ± 0.4 4 years4 8.6 ± 0.6 - - 7 years5 8.1 ± 0.6 - - 25 years4 7.3 ± 0.0 4 4.0 ± 0.3 45 years4 6.0 ± 0.3 6 2.8 ± 0.6 70 years6 5.2 ± 0.6 6 1.7 ± 0.4 N = number of crossover pairs (using up-and-down method of quantal response)
Opioids or benzodiazepines decrease the amounts of SUPRANE® (desflurane, USP) required to produce anesthesia. The following table is based on studies of drug interaction (MAC reduction).
SUPRANE® (desflurane, USP) MAC WITH FENTANYL OR MIDAZOLAM
MEAN ± SD (percent reduction)Dose18-30 years31-65 yearsNo fentanyl6.4 ± 0.06.3 ± 0.43 µg/kg fentanyl3.5 ± 1.9
(46%)3.1 ± 0.6
(51%)6 µg/kg fentanyl3.0 ± 1.2
(53%)2.3 ± 1.0
(64%)No midazolam6.9 ± 0.15.9 ± 0.625 µg/kg midazolam-4.9 ± 0.9
(16%)50 µg/kg midazolam-4.9 ± 0.5
(17%)SUPRANE® (desflurane, USP) decreases the doses of neuromuscular blocking agents required (see PRECAUTIONS , Drug Interactions ).
During the maintenance of anesthesia with inflow rates of 2 L/min or more, the alveolar concentration of desflurane will usually be within 10% of the inspired concentration. (F A /F I , see Figure 1 in Pharmacokinetics section.)
HOW SUPPLIED
SUPRANE® (desflurane, USP), NDC 10019-641-24, is packaged in amber-colored bottles containing 240 mL desflurane.
SAFETY AND HANDLING
Occupational Caution: There is no specific work exposure limit established for SUPRANE® (desflurane, USP). However, the National Institute for Occupational Safety and Health Administration has recommended an 8-hr, time-weighted average limit of 2 ppm for halogenated anesthetic agents in general (0.5 ppm when coupled with exposure to N 2 O).
The predicted effects of acute overexposure by inhalation of SUPRANE® (desflurane, USP) include headache, dizziness or (in extreme cases) unconsciousness.
There are no documented adverse effects of chronic exposure to halogenated anesthetic vapors ( W aste A nesthetic G ases or WAGs) in the workplace. Although results of some epidemiological studies suggest a link between exposure to halogenated anesthetics and increased health problems (particularly spontaneous abortion), the relationship is not conclusive. Since exposure to WAGs is one possible factor in the findings for these studies, operating room personnel, and pregnant women in particular, should minimize exposure. Precautions include adequate general ventilation in the operating room, the use of a well-designated and well-maintained scavenging system, work practices to minimize leaks and spills while the anesthetic agent is in use, and routine equipment maintenance to minimize leaks.
STORAGE
Store at room temperature, 15°-30°C (59°-86°F). SUPRANE® (desflurane, USP) has been demonstrated to be stable for the period defined by the expiration dating on the label. The bottle cap should be replaced after each use of SUPRANE®.
Manufactured for
Baxter Healthcare Corporation
Deerfield, IL 60015 USA
by: Baxter Healthcare Corporation of Puerto Rico
Guayama, Puerto Rico 00784 USA
Revised: January 2001
For Product Inquiry 1 800 ANA DRUG
(1-800-262-3784)
400-447-08
Subscribe to the "News" RSS Feed 
TOP ۞
