-
Zegerid Powder for Oral Solution (Santarus)
DESCRIPTION
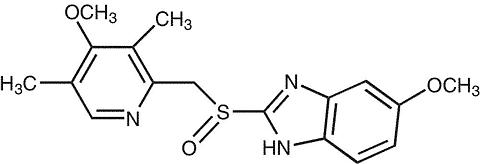
The active ingredient in ZEGERID® (omeprazole) Powder for Oral Suspension, is a substituted benzimidazole, 5-methoxy-2-[[(4-methoxy-3,5-dimethyl-2-pyridinyl)meth-yl]sulfinyl]-1H-benzimidazole, a racemic mixture of two enantiomers that inhibits gastric acid secretion. Its empirical formula is C 17 H 19 N 3 O 3 S, with a molecular weight of 345.42. The structural formula is:
Omeprazole is a white to off-white crystalline powder which melts with decomposition at about 155°C. It is a weak base, freely soluble in ethanol and methanol, and slightly soluble in acetone and isopropanol and very slightly soluble in water. The stability of omeprazole is a function of pH; it is rapidly degraded in acid media, but has acceptable stability under alkaline conditions.
ZEGERID® Powder for Oral Suspension is supplied in unit dose packets as an immediate-release formulation. Each packet contains 40 or 20 mg of omeprazole and the following excipients: sodium bicarbonate, xylitol, sucrose, sucralose, xanthan gum, and flavorings.
CLINICAL PHARMACOLOGY
Omeprazole is acid labile and thus rapidly degraded by gastric acid. ZEGERID® Powder for Oral Suspension is an immediate-release formulation that contains sodium bicarbonate to protect omeprazole from acid degradation.
Pharmacokinetics:
Absorption
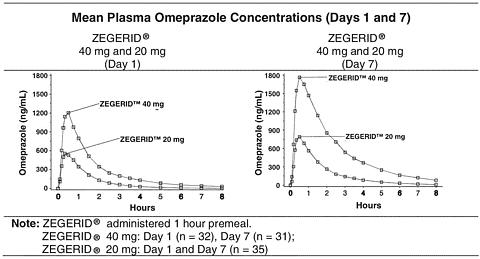
When ZEGERID® is administered on an empty stomach 1 hour prior to a meal, absorption of omeprazole is rapid, with mean peak plasma levels of omeprazole occurring at about 30 minutes (range 10 to 90 minutes) after a single dose or repeated-dose administration (see figures below).
When ZEGERID® 40 mg was administered in a two-dose loading regimen, the AUC(0-inf) (ng[ast ]hr/mL) was 1665 after Dose 1 and 3356 after Dose 2, while Tmax was approximately 30 minutes for both Dose 1 and Dose 2.
Following single or repeated once daily dosing, peak plasma concentrations of omeprazole from ZEGERID® are approximately proportional from 20 to 40 mg doses, but a greater than linear mean AUC (three-fold increase) is observed when doubling the dose to 40 mg. The bioavailability of omeprazole from ZEGERID® Powder for Oral Suspension increases upon repeated administration of ZEGERID®.
Pharmacokinetic Parameters of ZEGERID® Following Oral 40 mg or 20 mg Once-Daily Dosing for 1 and 7 Days Day 1 Parameter40 mg 20 mg AUC(0-inf) (ng*hr/mL)2228 825 Coefficient of variation107% 72% Cmax (ng/mL)1412 672 Coefficient of variation44% 44% Tmax (min)26.6 29.8 T ½ (hr)1.00 0.86 Values represent arithmetic means.Day 7 Parameter40 mg 20 mg AUC(0-inf) (ng*hr/mL)4640 1446 Coefficient of variation59% 61% Cmax (ng/mL)1954 902 Coefficient of variation33% 40% Tmax (min)34.7 28.3 T ½ (hr)1.38 1.08 Values represent arithmetic means.When ZEGERID® is administered 1 hour after a meal, Cmax and AUC are reduced by approximately 62% and 26%, respectively, relative to administration 1 hour prior to a meal.
Distribution
Omeprazole is bound to plasma proteins. Protein binding is approximately 95%.
Metabolism
Absolute bioavailability (compared to intravenous administration) is about 30-40% at doses of 20-40 mg, due in large part to presystemic metabolism.
Excretion
In healthy subjects, the mean plasma half-life is 1 hour (range 0.4 to 3.2 hours), and the total body clearance is 500-600 mL/min.
Following single dose oral administration of omeprazole, little if any unchanged drug is excreted in urine. The majority of the dose (about 77%) is eliminated in urine as at least six metabolites. Two metabolites have been identified as hydroxyomeprazole and the corresponding carboxylic acid. The remainder of the dose was recoverable in feces. This implies a significant biliary excretion of the metabolites of omeprazole. Three metabolites have been identified in plasma -- the sulfide and sulfone derivatives of omeprazole, and hydroxyomeprazole. These metabolites have very little or no antisecretory activity.
Special Populations
Geriatric
The elimination rate of omeprazole was somewhat decreased in the elderly, and bioavailability was increased. Omeprazole was 76% bioavailable when a single 40-mg oral dose of omeprazole (buffered solution) was administered to healthy elderly subjects, versus 58% in young subjects given the same dose. Nearly 70% of the dose was recovered in urine as metabolites of omeprazole and no unchanged drug was detected. The plasma clearance of omeprazole was 250 mL/min (about half that of young subjects) and its plasma half-life averaged one hour, similar to that of young healthy subjects.
Pediatric
The pharmacokinetics of ZEGERID® have not been studied in patients < 18 years of age.
Gender
There are no known differences in the absorption or excretion of omeprazole between males and females.
Hepatic Insufficiency
In patients with chronic hepatic disease, the bioavailability of omeprazole from a buffered solution increased to approximately 100% compared to an I.V. dose, reflecting decreased first-pass effect, and the mean plasma half-life of the drug increased to nearly 3 hours compared to the mean half-life of 1 hour in normal subjects. Plasma clearance averaged 70 mL/min, compared to a value of 500-600 mL/min in normal subjects.
Renal Insufficiency
In patients with chronic renal impairment, whose creatinine clearance ranged between 10 and 62 mL/min/1.73m 2 , the disposition of omeprazole from a buffered solution was very similar to that in healthy subjects, although there was a slight increase in bioavailability. Because urinary excretion is a primary route of excretion of omeprazole metabolites, their elimination slowed in proportion to the decreased creatinine clearance.
Asians
In pharmacokinetic studies of single 20-mg omeprazole doses, an increase in AUC of approximately four-fold was noted in Asian subjects compared to Caucasians.
Dose adjustment, particularly where maintenance of healing of erosive esophagitis is indicated, for the hepatically impaired and Asian subjects should be considered.
Drug-Drug Interactions
When omeprazole 40 mg once daily was given in combination with clarithromycin 500 mg every 8 hours to healthy adult male subjects, the steady-state plasma concentrations of omeprazole were increased by the concomitant administration of clarithromycin (Cmax, AUC(0-24) and T ½ increased 30%, 89%, and 34%, respectively).
Pharmacodynamics:
Mechanism of Action
Omeprazole belongs to a class of antisecretory compounds, the substituted benzimidazoles, that do not exhibit anticholinergic or H2 histamine antagonistic properties, but that suppress gastric acid secretion by specific inhibition of the H+/K+ ATPase enzyme system at the secretory surface of the gastric parietal cell. Because this enzyme system is regarded as the acid (proton) pump within the gastric mucosa, omeprazole has been characterized as a gastric acid-pump inhibitor, in that it blocks the final step of acid production. This effect is dose related and leads to inhibition of both basal and stimulated acid secretion irrespective of the stimulus. Animal studies indicate that after rapid disappearance from plasma, omeprazole can be found within the gastric mucosa for a day or more.
Antisecretory Activity
Results from two studies of the antisecretory effect of repeated once-daily dosing of 40 mg and 20 mg of ZEGERID® in healthy subjects are shown below.
Effect of ZEGERID® on Intragastric pH on Day 7 Parameter40 mg
(N=24)20 mg
(N=28)% Decrease from Baseline for Integrated Gastric Acidity (mmol*hr/L)84% 82% Coefficient of variation20% 24% % Time Gastric pH > 4 *77% 51% (Hours) *(18.6 h) (12.2 h) Coefficient of variation27% 43% Median pH5.2 4.2 Coefficient of variation17% 37% Note: Values represent medians. All parameters were measured over a 24-hour period.* p < 0.05 20 mg vs. 40 mgThe antisecretory effect thus lasts far longer than would be expected from the very short (1 hour) plasma half-life, apparently due to irreversible binding to the parietal H+/K+ ATPase enzyme.
Repeated single daily oral doses of ZEGERID® 40 mg and 20 mg have produced nearly 100% inhibition of 24-hour integrated gastric acidity in some subjects.
In 178 critically ill patients treated with ZEGERID® 40 mg via nasogastric or orogastric tube, the median daily gastric pH was above 4 in >/= 95% of patients over the course of the 14-day trial. The gastric pH was above 4 for almost all patients beginning with the first dose (99% of patients 1-2.5 hours postdose and 92% of patients 6 hours postdose).
Enterochromaffin-like (ECL) Cell Effects
In 24-month carcinogenicity studies in rats, a dose-related significant increase in gastric carcinoid tumors and ECL cell hyperplasia was observed in both male and female animals (see PRECAUTIONS , Carcinogenesis, Mutagenesis, Impairment of Fertility ). Carcinoid tumors have also been observed in rats subjected to fundectomy or long-term treatment with other proton pump inhibitors or high doses of H2-receptor antagonists. Human gastric biopsy specimens have been obtained from more than 3000 patients treated with omeprazole in long-term clinical trials. The incidence of ECL cell hyperplasia in these studies increased with time; however, no case of ECL cell carcinoids, dysplasia, or neoplasia has been found in these patients.
However, these studies are of insufficient duration and size to rule out the possible influence of long-term administration of omeprazole on the development of any premalignant or malignant conditions.
Serum Gastrin Effects
In studies involving more than 200 patients, serum gastrin levels increased during the first 1 to 2 weeks of once-daily administration of therapeutic doses of omeprazole in parallel with inhibition of acid secretion. No further increase in serum gastrin occurred with continued treatment. In comparison with histamine H2-receptor antagonists, the median increases produced by 20 mg doses of omeprazole were higher (1.3 to 3.6 fold vs. 1.1 to 1.8 fold increase). Gastrin values returned to pretreatment levels, usually within 1 to 2 weeks after discontinuation of therapy.
Other Effects
Systemic effects of omeprazole in the CNS, cardiovascular and respiratory systems have not been found to date. Omeprazole, given in oral doses of 30 or 40 mg for 2 to 4 weeks, had no effect on thyroid function, carbohydrate metabolism, or circulating levels of parathyroid hormone, cortisol, estradiol, testosterone, prolactin, cholecystokinin or secretin.
No effect on gastric emptying of the solid and liquid components of a test meal was demonstrated after a single dose of omeprazole 90 mg. In healthy subjects, a single I.V. dose of omeprazole (0.35 mg/kg) had no effect on intrinsic factor secretion. No systematic dose-dependent effect has been observed on basal or stimulated pepsin output in humans. However, when intragastric pH is maintained at 4.0 or above, basal pepsin output is low, and pepsin activity is decreased.
As do other agents that elevate intragastric pH, omeprazole administered for 14 days in healthy subjects produced a significant increase in the intragastric concentrations of viable bacteria. The pattern of the bacterial species was unchanged from that commonly found in saliva. All changes resolved within three days of stopping treatment.
The course of Barrett's esophagus in 106 patients was evaluated in a U.S. double-blind controlled study of omeprazole 40 mg b.i.d. for 12 months followed by 20 mg b.i.d. for 12 months or ranitidine 300 mg b.i.d. for 24 months. No clinically significant impact on Barrett's mucosa by antisecretory therapy was observed. Although neosquamous epithelium developed during antisecretory therapy, complete elimination of Barrett's mucosa was not achieved. No significant difference was observed between treatment groups in development of dysplasia in Barrett's mucosa and no patient developed esophageal carcinoma during treatment. No significant differences between treatment groups were observed in development of ECL cell hyperplasia, corpus atrophic gastritis, corpus intestinal metaplasia, or colon polyps exceeding 3 mm in diameter (see also CLINICAL PHARMACOLOGY , Enterochromaffin-like (ECL) Cell Effects ).
Clinical Studies
Duodenal Ulcer Disease
Active Duodenal Ulcer - In a multicenter, double-blind, placebo controlled study of 147 patients with endoscopically documented duodenal ulcer, the percentage of patients healed (per protocol) at 2 and 4 weeks was significantly higher with omeprazole 20 mg once a day than with placebo (p </= 0.01).
Treatment of Active Duodenal Ulcer
% of Patients HealedOmeprazole
20 mg a.m.
(n = 99)Placebo
a.m.
(n = 48)Week 2* 41 13 Week 4* 75 27 * (p </= 0.01)Complete daytime and nighttime pain relief occurred significantly faster (p </= 0.01) in patients treated with omeprazole 20 mg than in patients treated with placebo. At the end of the study, significantly more patients who had received omeprazole had complete relief of daytime pain (p </= 0.05) and nighttime pain (p </= 0.01).
In a multicenter, double-blind study of 293 patients with endoscopically documented duodenal ulcer, the percentage of patients healed (per protocol) at 4 weeks was significantly higher with omeprazole 20 mg once a day than with ranitidine 150 mg b.i.d. (p < 0.01).
Treatment of Active Duodenal Ulcer
% of Patients HealedOmeprazole
20 mg a.m.
(n = 145)Ranitidine
150 mg b.i.d.
(n = 148)Week 242 34 Week 4* 82 63 * (p < 0.01)Healing occurred significantly faster in patients treated with omeprazole than in those treated with ranitidine 150 mg b.i.d. (p < 0.01).
In a foreign multinational randomized, double-blind study of 105 patients with endoscopically documented duodenal ulcer, 40 mg and 20 mg of omeprazole were compared to 150 mg b.i.d. of ranitidine at 2, 4 and 8 weeks. At 2 and 4 weeks both doses of omeprazole were statistically superior (per protocol) to ranitidine, but 40 mg was not superior to 20 mg of omeprazole, and at 8 weeks there was no significant difference between any of the active drugs.
Treatment of Active Duodenal Ulcer
% of Patients HealedOmeprazole Ranitidine 40 mg
(n = 36)20 mg
(n = 34)150 mg b.i.d.
(n = 35)Week 2* 83 * 83 53 Week 4* 100 * 97 82 Week 8100 100 94 * (p </= 0.01)Gastric Ulcer
In a U.S. multicenter, double-blind, study of omeprazole 40 mg once a day, 20 mg once a day, and placebo in 520 patients with endoscopically diagnosed gastric ulcer, the following results were obtained.
Treatment of Gastric Ulcer
% of Patients Healed
(All Patients Treated)Omeprazole
40 mg q.d.
(n = 214)Omeprazole 20 mg q.d.
(n = 202)Placebo
(n = 104)Week 455.6 ** 47.5 ** 30.8 Week 882.7 ** + 74.8 ** 48.1 ** (p < 0.01) Omeprazole 40 mg or 20 mg versus placebo+ (p < 0.05) Omeprazole 40 mg versus 20 mgFor the stratified groups of patients with ulcer size less than or equal to 1 cm, no difference in healing rates between 40 mg and 20 mg was detected at either 4 or 8 weeks. For patients with ulcer size greater than 1 cm, 40 mg was significantly more effective than 20 mg at 8 weeks.
In a foreign, multinational, double-blind study of 602 patients with endoscopically diagnosed gastric ulcer, omeprazole 40 mg once a day, 20 mg once a day, and ranitidine 150 mg twice a day were evaluated.
Treatment of Gastric Ulcer
% of Patients Healed
(All Patients Treated)Omeprazole
40 mg q.d.
(n = 187)Omeprazole 20 mg q.d.
(n = 200)Ranitidine
150 mg b.i.d.
(n = 199)Week 478.1 ** , ++ 63.5 56.3 Week 891.4 ** , ++ 81.5 78.4 ** (p < 0.01) Omeprazole 40 mg versus ranitidine++ (p < 0.01) Omeprazole 40 mg versus 20 mgGastroesophageal Reflux Disease (GERD)
Symptomatic GERD
A placebo controlled study was conducted in Scandinavia to compare the efficacy of omeprazole 20 mg or 10 mg once daily for up to 4 weeks in the treatment of heartburn and other symptoms in GERD patients without erosive esophagitis. Results are shown below.
% Successful Symptomatic Outcome a Omeprazole
20 mg a.m.Omeprazole
10 mg a.m.Placebo
a.m.All patients46*, **/* 31 **/* 13 (n = 205) (n = 199) (n = 105) Patients with
confirmed GERD56 * , **/*
(n = 115)36 **/*
(n = 109)14
(n = 59)a Defined as complete resolution of heartburn* (p < 0.005) versus 10 mg**/* (p < 0.005) versus placeboErosive Esophagitis
In a U.S. multicenter double-blind placebo controlled study of 40 mg or 20 mg of omeprazole in patients with symptoms of GERD and endoscopically diagnosed erosive esophagitis of grade 2 or above, the percentage healing rates (per protocol) were as follows:
Omeprazole
40 mg
(n = 87)Omeprazole
20 mg
(n = 83)Placebo
(n = 43)Week 445 * 39 * 7 Week 875 * 74 * 14 * (p < 0.01) Omeprazole versus placebo.In this study, the 40-mg dose was not superior to the 20-mg dose of omeprazole in the percentage healing rate. Other controlled clinical trials have also shown that omeprazole is effective in severe GERD. In comparisons with histamine H2-receptor antagonists in patients with erosive esophagitis, grade 2 or above, omeprazole in a dose of 20 mg was significantly more effective than the active controls. Complete daytime and nighttime heartburn relief occurred significantly faster (p < 0.01) in patients treated with omeprazole than in those taking placebo or histamine H2-receptor antagonists.
In this and five other controlled GERD studies, significantly more patients taking 20 mg omeprazole (84%) reported complete relief of GERD symptoms than patients receiving placebo (12%).
Long Term Maintenance Treatment of Erosive Esophagitis
In a U.S. double-blind, randomized, multicenter, placebo controlled study, two dose regimens of omeprazole were studied in patients with endoscopically confirmed healed esophagitis. Results to determine maintenance of healing of erosive esophagitis are shown below.
Life Table Analysis Omeprazole
20 mg q.d.
(n = 138)Omeprazole
20 mg 3 days
per week
(n = 137)Placebo
(n = 131)Percent inendoscopicremission at6 months70 * 34 11 * (p < 0.01) Omeprazole 20 mg q.d. versus Omeprazole 20 mg 3 consecutive days per week or placebo.In an international multicenter double-blind study, omeprazole 20 mg daily and 10 mg daily were compared to ranitidine 150 mg twice daily in patients with endoscopically confirmed healed esophagitis. The table below provides the results of this study for maintenance of healing of erosive esophagitis.
Life Table Analysis Omeprazole
20 mg q.d.
(n = 131)Omeprazole
10 mg q.d.
(n = 133)Ranitidine
150 mg b.i.d.
(n = 128)Percent inendoscopicremission at12 months77 * 58 **/** 46 * (p = 0.01) Omeprazole 20 mg q.d. versus Omeprazole 10 mg q.d. or Ranitidine.**/** (p = 0.03) Omeprazole 10 mg q.d. versus Ranitidine.In patients who initially had grades 3 or 4 erosive esophagitis, for maintenance after healing 20 mg daily of omeprazole was effective, while 10 mg did not demonstrate effectiveness.
Reduction of Risk of Upper Gastrointestinal Bleeding in Critically Ill Patients
A double-blind, multicenter, randomized, non-inferiority clinical trial was conducted to compare ZEGERID® 40 mg oral suspension and intravenous cimetidine for the reduction of risk of upper GI bleeding in critically ill patients (mean APACHE II score = 23.7). The primary endpoint was significant upper gastrointestinal bleeding defined as bright red blood which did not clear after adjustment of the nasogastric tube and a 5 to 10 minute lavage, or persistent Gastroccult® positive coffee grounds for 8 consecutive hours which did not clear with 100 cc lavage. ZEGERID® 40 mg (two doses administered 6 to 8 hours apart on the first day via orogastric or nasogastric tube, followed by 40 mg q.d. thereafter) was compared to continuous I.V. cimetidine (300 mg bolus, and 50 to 100 mg/hr continuously thereafter) for up to 14 days (mean = 6.8 days). A total of 359 patients were studied, age range 16 to 91 (mean = 56 yrs), 58.5% were males, and 64% were Caucasians. The results of the study showed that ZEGERID® was non-inferior to I.V. cimetidine, 10/181(5.5%) patients in the cimetidine group vs. 7/178 (3.9%) patients in the ZEGERID® group experienced clinically significant upper GI bleeding.
INDICATIONS AND USAGE
Duodenal Ulcer
ZEGERID® Powder for Oral Suspension is indicated for short-term treatment of active duodenal ulcer. Most patients heal within four weeks. Some patients may require an additional four weeks of therapy.
Gastric Ulcer
ZEGERID® Powder for Oral Suspension is indicated for short-term treatment (4-8 weeks) of active benign gastric ulcer. (See CLINICAL PHARMACOLOGY , Clinical Studies , Gastric Ulcer .)
Treatment of Gastroesophageal Reflux Disease (GERD)
Symptomatic GERD
ZEGERID® Powder for Oral Suspension is indicated for the treatment of heartburn and other symptoms associated with GERD.
Erosive Esophagitis
ZEGERID® Powder for Oral Suspension is indicated for the short-term treatment (4-8 weeks) of erosive esophagitis which has been diagnosed by endoscopy.
(See CLINICAL PHARMACOLOGY , Clinical Studies .)
The efficacy of ZEGERID® used for longer than 8 weeks in these patients has not been established. In the rare instance of a patient not responding to 8 weeks of treatment, it may be helpful to give up to an additional 4 weeks of treatment. If there is recurrence of erosive esophagitis or GERD symptoms (eg, heartburn), additional 4-8 week courses of omeprazole may be considered.
Maintenance of Healing of Erosive Esophagitis
ZEGERID® Powder for Oral Suspension is indicated to maintain healing of erosive esophagitis. Controlled studies do not extend beyond 12 months.
Reduction of Risk of Upper Gastrointestinal Bleeding in Critically Ill Patients
ZEGERID® is indicated for the reduction of risk of upper gastrointestinal bleeding in critically ill patients.
CONTRAINDICATIONS
ZEGERID® Powder for Oral Suspension is contraindicated in patients with known hypersensitivity to any components of the formulation.
PRECAUTIONS
General
Symptomatic response to therapy with omeprazole does not preclude the presence of gastric malignancy.
Atrophic gastritis has been noted occasionally in gastric corpus biopsies from patients treated long-term with omeprazole.
Each 20 mg and 40 mg dose packet of ZEGERID® contains 460 mg sodium in the form of sodium bicarbonate. This should be taken into consideration for patients on a sodium-restricted diet.
Each 20 mg and 40 mg dose packet of ZEGERID® contains 1680 mg (20 mEq) of sodium bicarbonate. Sodium bicarbonate is contraindicated in patients with metabolic alkalosis and hypocalcemia. Sodium bicarbonate should be used with caution in patients with Bartter's syndrome, hypokalemia, respiratory alkalosis, and problems with acid-base balance. Long-term administration of bicarbonate with calcium or milk can cause milk-alkali syndrome.
Information for Patients
ZEGERID® is supplied as powder for oral suspension. It should be taken on an empty stomach at least one hour prior to a meal. ZEGERID® is available as 20 mg and 40 mg single dose packets.
Directions for use: Empty packet contents into a small cup containing 1-2 tablespoons of water. DO NOT USE OTHER LIQUIDS OR FOODS. Stir well and drink immediately. Refill cup with water and drink.
Drug Interactions
Other
Omeprazole can prolong the elimination of diazepam, warfarin and phenytoin, drugs that are metabolized by oxidation in the liver. There have been reports of increased INR and prothrombin time in patients receiving proton pump inhibitors, including omeprazole, and warfarin concomitantly. Increases in INR and prothrombin time may lead to abnormal bleeding and even death. Patients treated with proton pump inhibitors and warfarin may need to be monitored for increases in INR and prothrombin time. Although in normal subjects no interaction with theophylline or propranolol was found, there have been clinical reports of interaction with other drugs metabolized via the cytochrome P-450 system (eg, cyclosporine, disulfiram, benzodiazepines). Patients should be monitored to determine if it is necessary to adjust the dosage of these drugs when taken concomitantly with ZEGERID®.
Because of its profound and long-lasting inhibition of gastric acid secretion, it is theoretically possible that omeprazole may interfere with absorption of drugs where gastric pH is an important determinant of their bioavailability (eg, ketoconazole, ampicillin esters, and iron salts). In the clinical trials, antacids were used concomitantly with the administration of omeprazole.
Co-administration of omeprazole and clarithromycin have resulted in increases of plasma levels of omeprazole, clarithromycin, and 14-hydroxy-clarithromycin (see also CLINICAL PHARMACOLOGY , Pharmacokinetics ).
Carcinogenesis, Mutagenesis, Impairment of Fertility
In two 24-month carcinogenicity studies in rats, omeprazole at daily doses of 1.7, 3.4, 13.8, 44.0 and 140.8 mg/kg/day (approximately 0.5 to 28.5 times the human dose of 40 mg/day, based on body surface area) produced gastric ECL cell carcinoids in a dose-related manner in both male and female rats; the incidence of this effect was markedly higher in female rats, which had higher blood levels of omeprazole. Gastric carcinoids seldom occur in the untreated rat. In addition, ECL cell hyperplasia was present in all treated groups of both sexes. In one of these studies, female rats were treated with 13.8 mg omeprazole/kg/day (approximately 2.8 times the human dose of 40 mg/day, based on body surface area) for one year, then followed for an additional year without the drug. No carcinoids were seen in these rats. An increased incidence of treatment-related ECL cell hyperplasia was observed at the end of one year (94% treated vs 10% controls). By the second year the difference between treated and control rats was much smaller (46% vs 26%) but still showed more hyperplasia in the treated group. An unusual primary malignant tumor in the stomach was seen in one rat (2%). No similar tumor was seen in male or female rats treated for two years. For this strain of rat no similar tumor has been noted historically, but a finding involving only one tumor is difficult to interpret. In a 52-week toxicity study in Sprague-Dawley rats, brain astrocytomas were found in a small number of males that received omeprazole at dose levels of 0.4, 2, and 16 mg/kg/day (about 0.1 to 3.3 times the human dose of 40 mg/day, based on body surface area). No astrocytomas were observed in female rats in this study. In a 2-year carcinogenicity study in Sprague-Dawley rats, no astrocytomas were found in males and females at the high dose of 140.8 mg/kg/day (about 28.5 times the human dose of 40 mg per day, based on body surface area). A 78-week mouse carcinogenicity study of omeprazole did not show increased tumor occurrence, but the study was not conclusive. A 26-week p53 (+/-) transgenic mouse carcinogenicity study was not positive. Omeprazole was positive for clastogenic effects in an in vitro human lymphocyte chromosomal aberration assay, in one of two in vivo mouse micronucleus tests, and in an in vivo bone marrow cell chromosomal aberration assay. Omeprazole was negative in the in vitro Ames Salmonella typhimurium assay, an in vitro mouse lymphoma cell forward mutation assay and an in vivo rat liver DNA damage assay.
Omeprazole at oral doses up to 138.0 mg/kg/day (about 28 times the human dose of 40 mg per day, based on body surface area) was found to have no effect on fertility and reproductive performance.
Pregnancy
Pregnancy Category C
There are no adequate and well-controlled studies on the use of omeprazole in pregnant women. The vast majority of reported experience with omeprazole during human pregnancy is first trimester exposure and the duration of use is rarely specified, e.g., intermittent vs. chronic. An expert review of published data on experiences with omeprazole use during pregnancy by TERIS - the Teratogen Information System - concluded that therapeutic doses during pregnancy are unlikely to pose a substantial teratogenic risk (the quantity and quality of data were assessed as fair).
Three epidemiological studies compared the frequency of congenital abnormalities among infants born to women who used omeprazole during pregnancy to the frequency of abnormalities among infants of women exposed to H2-receptor antagonists or other controls. A population-based prospective cohort epidemiological study from the Swedish Medical Birth Registry, covering approximately 99% of pregnancies, reported on 955 infants (824 exposed during the first trimester with 39 of these exposed beyond first trimester, and 131 exposed after the first trimester) whose mothers used omeprazole during pregnancy. In utero exposure to omeprazole was not associated with increased risk of any malformation (odds ratio 0.82, 95% CI 0.50-1.34), low birth weight or low Apgar score. The number of infants born with ventricular septal defects and the number of stillborn infants was slightly higher in the omeprazole exposed infants than the expected number in the normal population. The author concluded that both effects may be random.
A retrospective cohort study reported on 689 pregnant women exposed to either H2-blockers or omeprazole in the first trimester (134 exposed to omeprazole). The overall malformation rate was 4.4% (95% CI 3.6-5.3) and the malformation rate for first trimester exposure to omeprazole was 3.6% (95% CI 1.5-8.1). The relative risk of malformations associated with first trimester exposure to omeprazole compared with nonexposed women was 0.9 (95% CI 0.3-2.2). The study could effectively rule out a relative risk greater than 2.5 for all malformations. Rates of preterm delivery or growth retardation did not differ between the groups.
A controlled prospective observational study followed 113 women exposed to omeprazole during pregnancy (89% first trimester exposures). The reported rates of major congenital malformations was 4% for the omeprazole group, 2% for controls exposed to nonteratogens, and 2.8% in disease-paired controls (background incidence of major malformations 1-5%). Rates of spontaneous and elective abortions, preterm deliveries, gestational age at delivery, and mean birth weight did not differ between the groups. The sample size in this study has 80% power to detect a 5-fold increase in the rate of major malformation.
Several studies have reported no apparent adverse short term effects on the infant when single dose oral or intravenous omeprazole was administered to over 200 pregnant women as premedication for cesarean section under general anesthesia.
Teratology studies conducted in pregnant rats at omeprazole doses up to 138 mg/kg/day (about 28 times the human dose of 40 mg/day, based on body surface area) and in pregnant rabbits at doses up to 69 mg/kg/day (about 28 times the human dose of 40 mg per day, based on body surface area) did not disclose any evidence for a teratogenic potential of omeprazole.
In rabbits, omeprazole in a dose range of 6.9 to 69.1 mg/kg/day (about 2.8 to 28 times the human dose of 40 mg per day, based on body surface area) produced dose-related increases in embryo-lethality, fetal resorptions and pregnancy disruptions. In rats, dose-related embryo/fetal toxicity and postnatal developmental toxicity were observed in offspring resulting from parents treated with omeprazole at 13.8 to 138.0 mg/kg/day (about 2.8 to 28 times the human dose of 40 mg per day, based on body surface area).
Chronic use of sodium bicarbonate may lead to systemic alkalosis and increased sodium intake can produce edema and weight increase. There are no adequate and well-controlled studies in pregnant women. Because animal studies and studies in humans cannot rule out the possibility of harm, omeprazole should be used during pregnancy only if the potential benefit to pregnant women justifies the potential risk to the fetus.
Nursing Mothers
Omeprazole concentrations have been measured in breast milk of a woman following oral administration of 20 mg. The peak concentration of omeprazole in breast milk was less than 7% of the peak serum concentration. The concentration will correspond to 0.004 mg of omeprazole in 200 mL of milk. In rats, omeprazole administration during late gestation and lactation at doses of 13.8 to 138 mg/kg/day (about 2.8 to 28 times the human dose of 40 mg per day, based on body surface area) resulted in decreased weight gain in pups. Because omeprazole is excreted in human milk, because of the potential for serious adverse reactions in nursing infants from omeprazole, and because of the potential for tumorigenicity shown for omeprazole in rat carcinogenicity studies, a decision should be taken to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother. In addition, sodium bicarbonate should be used with caution in nursing mothers.
Pediatric Use
Clinical studies have been conducted evaluating omeprazole in pediatric patients. There are no adequate and well-controlled studies in pediatric patients with ZEGERID®.
Geriatric Use
Omeprazole was administered to over 2000 elderly individuals (>/= 65 years of age) in clinical trials in the U.S. and Europe. There were no differences in safety and effectiveness between the elderly and younger subjects. Other reported clinical experience has not identified differences in response between the elderly and younger subjects, but greater sensitivity of some older individuals cannot be ruled out.
Pharmacokinetic studies with buffered omeprazole have shown the elimination rate was somewhat decreased in the elderly and bioavailability was increased. The plasma clearance of omeprazole was 250 mL/min (about half that of young subjects). The plasma half-life averaged one hour, about the same as that in nonelderly, healthy subjects taking ZEGERID®. However, no dosage adjustment is necessary in the elderly. (See CLINICAL PHARMACOLOGY .)
ADVERSE REACTIONS
Omeprazole was generally well tolerated during domestic and international clinical trials in 3096 patients.
In the U.S. clinical trial population of 465 patients, the following adverse experiences were reported to occur in 1% or more of patients on therapy with omeprazole. Numbers in parentheses indicate percentages of the adverse experiences considered by investigators as possibly, probably or definitely related to the drug.
Omeprazole (n = 465) Placebo
(n = 64)Ranitidine
(n = 195)Headache6.9 (2.4) 6.3 7.7 (2.6) Diarrhea3.0 (1.9) 3.1 (1.6) 2.1 (0.5) Abdominal Pain2.4 (0.4) 3.1 2.1 Nausea2.2 (0.9) 3.1 4.1 (0.5) URI1.9 1.6 2.6 Dizziness1.5 (0.6) 0.0 2.6 (1.0) Vomiting1.5 (0.4) 4.7 1.5 (0.5) Rash1.5 (1.1) 0.0 0.0 Constipation1.1 (0.9) 0.0 0.0 Cough1.1 0.0 1.5 Asthenia1.1 (0.2) 1.6 (1.6) 1.5 (1.0) Back Pain1.1 0.0 0.5 The following adverse reactions which occurred in 1% or more of omeprazole-treated patients have been reported in international double-blind, and open-label, clinical trials in which 2,631 patients and subjects received omeprazole.
Incidence of Adverse Experiences >/= 1%
Causal Relationship not AssessedOmeprazole
(n = 2631)Placebo
(n = 120)Body as a Whole, site unspecifiedAbdominal pain5.2 3.3 Asthenia1.3 0.8 Digestive SystemConstipation1.5 0.8 Diarrhea3.7 2.5 Flatulence2.7 5.8 Nausea4.0 6.7 Vomiting3.2 10.0 Acid regurgitation1.9 3.3 Nervious System/PsychiatricHeadache2.9 2.5 A controlled clinical trial conducted in 359 critically ill patients, comparing ZEGERID® 40 mg once daily to I.V. cimetidine 1200 mg/day for up to 14 days, demonstrated that the adverse event profile for ZEGERID® was similar to that of I.V. cimetidine.
The incidence and total number of AEs experienced by >/= 3% of patients in either group are presented in the table below by relationship to trial drug, body system, and preferred term.
Number (%) of Critically Ill Patients with Frequently Occurring
(>/= 3%) Adverse Events by Body System and Preferred TermZEGERID®
(N=178)Cimetidine
(N=181)MedDRABody SystemAll AEs All AEs Preferred Termn (%) n (%) BLOOD AND LYMPHATIC SYSTEM DISORDERSAnaemia NOS14 (7.9) 14 (7.7) Anaemia NOS Aggravated4 (2.2) 7 (3.9) Thrombocytopenia18 (10.1) 11 (6.1) CARDIAC DISORDERSAtrial Fibrillation11 (6.2) 7 (3.9) Bradycardia NOS7 (3.9) 5 (2.8) Supraventricular Tachycardia6 (3.4) 2 (1.1) Tachycardia NOS6 (3.4) 6 (3.3) Ventricular Tachycardia8 (4.5) 6 (3.3) GASTROINTESTINAL DISORDERS *Constipation8 (4.5) 8 (4.4) Diarrhoea NOS7 (3.9) 15 (8.3) Gastric Hypomotility3 (1.7) 6 (3.3) GENERAL DISORDERS AND
ADMINISTRATION SITE CONDITIONSHyperpyrexia8 (4.5) 3 (1.7) Oedema NOS5 (2.8) 11 (6.1) Pyrexia36 (20.2) 29 (16.0) INFECTIONS AND INFESTATIONSCandidal Infection NOS3 (1.7) 7 (3.9) Oral Candidiasis7 (3.9) 1 (0.6) Sepsis NOS9 (5.1) 9 (5.0) Urinary Tract Infection NOS4 (2.2) 6 (3.3) INVESTIGATIONSLiver Function Tests NOS Abnormal3 (1.7) 6 (3.3) METABOLISM AND NUTRITION DISORDERSFluid Overload9 (5.1) 14 (7.7) Hyperglycaemia NOS19 (10.7) 21 (11.6) Hyperkalaemia4 (2.2) 6 (3.3) Hypernatraemia3 (1.7) 9 (5.0) Hypocalcaemia11 (6.2) 10 (5.5) Hypoglycaemia NOS6 (3.4) 8 (4.4) Hypokalaemia22 (12.4) 24 (13.3) Hypomagnesaemia18 (10.1) 18 (9.9) Hyponatraemia7 (3.9) 5 (2.8) Hypophosphataemia11 (6.2) 7 (3.9) PSYCHIATRIC DISORDERSAgitation6 (3.4) 16 (8.8) RESPIRATORY, THORACIC AND MEDIASTINAL DISORDERSAcute Respiratory Distress Syndrome6 (3.4) 7 (3.9) Nosocomial Pneumonia20 (11.2) 17 (9.4) Pneumothorax NOS1 (0.6) 8 (4.4) Respiratory Failure3 (1.7) 6 (3.3) SKIN AND SUBCUTANEOUS TISSUE DISORDERSDecubitus Ulcer6 (3.4) 5 (2.8) Rash NOS10 (5.6) 11 (6.1) VASCULAR DISORDERSHypertension NOS14 (7.9) 6 (3.3) Hypotension NOS17 (9.6) 12 (6.6) * Clinically significant UGI bleeding was considered an SAE but it is not included in this table.Additional adverse experiences occurring in < 1% of patients or subjects in domestic and/or international trials conducted with omeprazole, or occurring since the drug was marketed, are shown below within each body system. In many instances, the relationship to omeprazole was unclear.
Body As a Whole
Allergic reactions, including, rarely, anaphylaxis (see also Skin below), fever, pain, fatigue, malaise, abdominal swelling.
Cardiovascular
Chest pain or angina, tachycardia, bradycardia, palpitation, elevated blood pressure, and peripheral edema.
Gastrointestinal
Pancreatitis (some fatal), anorexia, irritable colon, flatulence, fecal discoloration, esophageal candidiasis, mucosal atrophy of the tongue, dry mouth. During treatment with omeprazole, gastric fundic gland polyps have been noted rarely. These polyps are benign and appear to be reversible when treatment is discontinued.
Gastroduodenal carcinoids have been reported in patients with Zollinger-Ellison syndrome on long-term treatment with omeprazole. This finding is believed to be a manifestation of the underlying condition, which is known to be associated with such tumors.
Hepatic
Mild and, rarely, marked elevations of liver function tests [ALT (SGPT), AST (SGOT), (gamma)-glutamyl transpeptidase, alkaline phosphatase, and bilirubin (jaundice)]. In rare instances, overt liver disease has occurred, including hep-atocellular, cholestatic, or mixed hepatitis, liver necrosis (some fatal), hepatic failure (some fatal), and hepatic encephalopathy.
Metabolic/Nutritional
Hyponatremia, hypoglycemia, and weight gain.
Musculoskeletal
Muscle cramps, myalgia, muscle weakness, joint pain, and leg pain.
Nervous System/Psychiatric
Psychic disturbances including depression, aggression, hallucinations, confusion, insomnia, nervousness, tremors, apathy, somnolence, anxiety, dream abnormalities; vertigo; paresthesia; and hemifacial dysesthesia.
Respiratory
Epistaxis, pharyngeal pain
Skin
Rash and rarely, cases of severe generalized skin reactions including toxic epidermal necrolysis (TEN; some fatal), Stevens-Johnson syndrome, and erythema multiforme (some severe); purpura and/or petechiae (some with rechallenge); skin inflammation, urticaria, angioedema, pruritus, alopecia, dry skin, and hyperhidrosis
Special Senses
Tinnitus, taste perversion
Ocular
Blurred vision, ocular irritation, dry eye syndrome, optic atrophy, anterior ischemic optic neuropathy, optic neuritis and double vision.
Urogenital
Interstitial nephritis (some with positive rechallenge), urinary tract infection, microscopic pyuria, urinary frequency, elevated serum creatinine, proteinuria, hematuria, glycosuria, testicular pain, and gynecomastia.
Hematologic
Rare instances of pancytopenia, agranulocytosis (some fatal), thrombocytopenia, neutropenia, anemia, leucocytosis, and hemolytic anemia have been reported.
The incidence of clinical adverse experiences in patients greater than 65 years of age was similar to that in patients 65 years of age or less.
Additional adverse reactions that could be caused by sodium bicarbonate, include metabolic alkalosis, seizures, and tetany.
OVERDOSAGE
Reports have been received of overdosage with omeprazole in humans. Doses ranged up to 2400 mg (120 times the usual recommended clinical dose). Manifestations were variable, but included confusion, drowsiness, blurred vision, tachycardia, nausea, vomiting, diaphoresis, flushing, headache, dry mouth, and other adverse reactions similar to those seen in normal clinical experience. (See ADVERSE REACTIONS .) Symptoms were transient, and no serious clinical outcome has been reported when omeprazole was taken alone. No specific antidote for omeprazole overdosage is known. Omeprazole is extensively protein bound and is, therefore, not readily dialyzable. In the event of overdosage, treatment should be symptomatic and supportive.
As with the management of any overdose, the possibility of multiple drug ingestion should be considered. For current information on treatment of any drug overdose, a certified Regional Poison Control Center should be contacted. Telephone numbers are listed in the Physicians' Desk Reference (PDR) or local telephone book.
Single oral doses of omeprazole at 1350, 1339, and 1200 mg/kg were lethal to mice, rats, and dogs, respectively. Animals given these doses showed sedation, ptosis, tremors, convulsions, and decreased activity, body temperature, and respiratory rate and increased depth of respiration.
In addition, a sodium bicarbonate overdose may cause hypocalcemia, hypokalemia, hypernatremia, and seizures.
DOSAGE AND ADMINISTRATION
Short-Term Treatment of Active Duodenal Ulcer
The recommended adult oral dose of ZEGERID® is 20 mg once daily. Most patients heal within four weeks. Some patients may require an additional four weeks of therapy. (See INDICATIONS AND USAGE .)
Gastric Ulcer
The recommended adult oral dose is 40 mg once a day for 4-8 weeks. (See CLINICAL PHARMACOLOGY , Clinical Studies , Gastric Ulcer , and INDICATIONS AND USAGE , Gastric Ulcer .)
Gastroesophageal Reflux Disease (GERD)
The recommended adult oral dose for the treatment of patients with symptomatic GERD and no esophageal lesions is 20 mg daily for up to 4 weeks. The recommended adult oral dose for the treatment of patients with erosive esophagitis and accompanying symptoms due to GERD is 20 mg daily for 4 to 8 weeks. (See INDICATIONS AND USAGE .)
Maintenance of Healing of Erosive Esophagitis
The recommended adult oral dose is 20 mg daily. (See CLINICAL PHARMACOLOGY , Clinical Studies .)
Reduction of Risk of Upper Gastrointestinal Bleeding in Critically Ill Patients
The recommended adult oral dose of ZEGERID® is 40 mg initially, followed by 40 mg after 6 to 8 hours as a loading dose on the first day, then 40 mg once daily for up to 14 days. (See CLINICAL PHARMACOLOGY , Clinical Studies .) The use of ZEGERID® in critically ill patients beyond 14 days has not been evaluated.
Preparation and Administration of Suspension
ZEGERID® is supplied as unit dose packets containing an immediate-release omeprazole powder for oral suspension (40 mg or 20 mg). It should be taken on an empty stomach at least 1 hour prior to a meal. For patients receiving continuous NG/OG tube feeding, enteral feeding should be suspended approximately 3 hours before and 1 hour after administration of ZEGERID®.
Directions for use: Empty packet contents into a small cup containing 1-2 tablespoons of water. DO NOT USE OTHER LIQUIDS OR FOODS. Stir well and drink immediately. Refill cup with water and drink.
If ZEGERID® is to be administered through a nasogastric or orogastric tube, the suspension should be constituted with approximately 20 mL of water. DO NOT USE OTHER LIQUIDS OR FOODS. Stir well and administer immediately. An appropriately-sized syringe should be used to instill the suspension in the tube. The suspension should be washed through the tube with 20 mL of water.
HOW SUPPLIED
ZEGERID® is a white flavored powder packaged in individual dose packets. It is supplied as follows:
NDC 68012-052-30 Cartons of 30: 20 mg unit dose packets
NDC 68012-054-30 Cartons of 30: 40 mg unit dose packets
Storage
Store ZEGERID® in its original individual packets. Store at 25°C (68-77°F): excursions permitted to 15-30°C (59-86°F). [see USP Controlled Room Temperature]
Santarus, Inc.®
ZEGERID® is a trademark of Santarus, Inc.
Manufactured for: Santarus, Inc.,
San Diego, CA 92130 · 1-888-778-0887
By: Patheon Inc., Whitby, Ontario L1N 5Z5, Canada
Subscribe to the "News" RSS Feed 
TOP ۞
